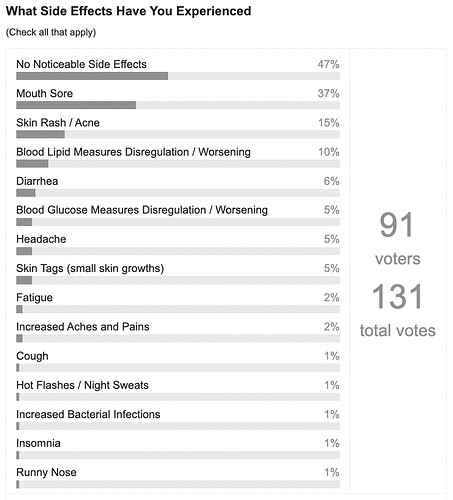
As you can see above, in a small survey of rapamycin users done in August, 2022, most people experience no noticeable side effects when dosing in the typical range currently being dosed for anti-aging applications (3mg to 10mg, single dose per week).
The side effects that people do experience are mostly very mild and temporary. Most people continue to take the medication and the problems (e.g. canker sore, small rash) typically go away over a few days with no treatment or minor treatment.
A small percent of people (approx. 3% or so from my estimation) have some side effect significant enough to make them want to stop taking the medication. I’ve also heard of one instance where a person suffered from significant skin rashes so decided to stop the medication quite quickly after initiating it. The side effects seem to be highly personalized and frequently not extremely dose dependent. While the Mannick study of 2014 of a rapalog (acts like rapamycin) saw higher side effect levels at higher dosages, in the experiences from people we’ve seen talked with it seems like the vast majority (95%+) start with lower medication levels, then slowly increase, and may occasionally get mild side effects like a canker sore that goes away - they don’t typically see higher side effect profiles as they ramp up the dose.
I personally have had a single canker sore (technical name aphthous ulcers). It happened early on when I started rapamycin. I think it was when I was at a couple of milligrams (mg) of rapamycin. It started a day after I took the rapamycin, and slowly got better over the next few days. I haven’t had it since (its been nearly two years, and I’m now up to a dose of around 10mg per week, all in one dose. Other people, like Peter Attia, have mentioned occasionally getting canker sores on rapamycin during times of high stress, eg, getting head-butted by your child during play.
Skin rashes are also something I get occasionally which seem highly tied to my rapamycin use. I get a small rash about the size of a quarter on my wrist under where my Fitbit sits. I’ve never had these until I started rapamycin. They come on after I take rapamycin. I use cortisol cream on the rash and it mostly goes away usually within a few days. A few people have reported more persistent and larger rashes developing.
Doctor Green has the largest practice prescribing rapamycin for aging users - with over 700 patients, so he is, theoretically in a good position to have detailed information on the topic of side effects and their frequency and type, if he is keeping detailed records on all his patients throughout the year. Here is a recent note from him (forwarded to me by one of his patients):
From Dr. Alan Green: Five Year Update, October 2021
Increased Risk Bacterial Infection
Five years and 760 patients have revealed that the single major risk of weekly Rapamycin is increased risk of bacterial infection." He suggests having antibiotics (like azithromycin) on hand.
[Note: There is some very significant disagreement about Dr. Green’s above statement, by other medical professionals I’ve talked to with experience with rapamycin. Bacterial infections, and use of antibiotics to treat them, is extremely common in the USA. I found it very hard to get good numbers on the typical percent of a population in the US that get bacterial infections each year, but this document from PEW Trusts suggests that antibiotics in the US are prescribed at a rate of 838 for every 1,000 people (measured in 2015) - which suggests upwards of 84% of Americans (or at least their prescribing doctors) think they have a bacterial infection each year severe enough to require antibiotics. Dr. Green has suggested only 5% to 10% of his patients get bacterial infections in any year, which suggests a much lower than average rate of infection than normal for rapamycin users. Moreover, it is not something that the users of rapamycin that participate in forums suggest is a common issue. So, take this with a grain of salt until more data is provided by Dr. Green.]
Dr. Alan Green has also responded by saying this in an interview in 2017:
What are the side-effects?
The side effects of daily rapamycin are TOTALLY different from the side-effects of weekly rapamycin. Daily rapamycin is used to reduce both mTORC1 and mTORC2. Rapamycin was introduced in 1999 to reduce mTORC2 for organ transplant.
Reduction of mTORC2 has significant side-effects. People can review elsewhere the side effects of reducing mTORC2. Almost all the harmful side-effects of rapamycin use are from lowering mTORC2 and all the beneficial anti-aging effects are from lowering mTORC1.
Weekly rapamycin is designed to lower mTORCl and preserve activity of mTORC2. Dosing interval of one week is based upon the rapamycin half-life of about 65 hours.
It is required to delay the next dose until there is a low blood level of rapamycin so as not to interfere with production of new mTORC2.
There are side effects from reducing MTORC1. The major side-effect of lowering mTORC1 is reducing the activity of the INNATE IMMUNE SYSTEM. The innate immune system is the first line of defense against bacterial infections and it involves neutrophils and macrophages, but not lymphocytes or antibodies. In my practice, everybody is warned of this danger and given a prescription of prophylactic antibiotics, (Z-pak) to have on hand and warned to aggressively treat fever or local signs of bacterial infection. My guess is 5-10% of patients might get a bacterial infection in a year and rapamycin increases the risk of serious bacterial infection. However, bacterial infections respond very well to prompt antibiotics.
On the other hand, the acquired immune system (lymphocytes) is improved as an anti-senescence effect and the risk of viral infection is reduced.
Very high levels of reduction of mTORC1 may cause aphthous stomatitis (canker sores). This is unusual at anti-aging preventive doses.
Aside from increased risk bacterial infections; there are minimal side-effects of weekly rapamycin as used in low doses to prevent age-related disease.
An off-target side effect of rapamycin is it’s an excellent anti-fungal agent. Longstanding cases of nail fungus (onychomycosis) are improved after prolonged treatment.
Different people’s side effect experiences with rapamycin:
Some people see an increase in their lipid level measurements (LDL and triglycerides), especially on higher doses of rapamycin.
I just had labs and my cholesterol readings went up some since I started Rapamycin. See discussion about this on this thread: Rapamycin and Cholesterol Levels? Any impact for you?
There is evidence (see study here) that suggests that even with higher lipid levels, rapamycin still actually decreases risk of cardiovascular disease. There is an ongoing discussion on rapamycin and cardiovascular risk in our forums.
I’ve experienced a development of acne which appears to coincide with my biweekly sirolimus dosing regimens. (from this thread - Rapamycin and Acne)
I had a rash on my scalp. It only bothered me when I put a brush through my hair. It didn’t change the texture, no-one could see it, and it has slowly become less and less. I’m pretty sure it was the Rapa.
I have been taking metformin for 12 years or more and rapamycin (Sirolimus) for the last 6 months or so. I had a couple of bad experiences with Sirolimus when I reached only 2mg (once per week). Most people are on 5mg plus. Some are as high as 20mg/week. My normal insulin level is very low, (2 U/L) and I believe that is why I have a low tolerance for Sirolimus (it sends insulin even lower). So to anyone contemplating using it, I would suggest to have your insulin level checked first and proceed with caution.
I’ve been taking Rapamycin now for a few weeks, I’m up to 8mg every second week. I’ve had an unusually frequent runny nose which is a known side effect, see: https://www.mayoclinic.org/.../side-effects/drg-20068199
I don’t feel it on the day but I don’t feel great the next day, I just feel a little off but not terrible. I also use health trackers both whoop and Garmin so I see my hrv, body battery and RHR all decrease the next day so it correlates. For me anyway
This person below was very light (around 100lbs) and ramped quickly up to a relatively high dose (4mg to 6mg):
Returning symptoms I experienced (up until 3-4 days after taking my dose, some a bit longer):
- Insomnia - I will be fully awake until 6-7AM in the morning (until 3-4 days after taking my dose).
- rash on my hand (strangely enough at a place where as a child I had eczema).
- Itchy minor rash at one of my feet
- Increased heart rate, at some moments really noticeable.
- Intense hot flashes/night sweats - I will end up drenched in sweat.
- Intense coughing at night for a few hours (had this twice, paired with the symptoms above).
Two canker sores over 16 months. Started at 5mg/WK and up to 15mg. Sores were around 8mg but none since going higher.
sirolimus reduced arthritus, and improved heart circulation, but at 4 mg dose I got a severe chest rash or hives 2 days after a dose. It fully cleared up after 14 days on a steroid. I will restart soon on a lower dose and be vigilant.
I have been taking 6 mg rapa once weekly for 2 years with zero side effects.
This person below was trying a very high dose or rapamycin (slowly working his way up from much lower doses) and began to see side effects at 20mg bi-weekly rapamycin with grapefruit juice (effectively around 60mg or 70mg of rapamycin, an extremely high level):
I just completed my second round of using rapamycin bi-weekly at a dose of 20mg with grapefruit juice. At this dosage, I experienced adverse side effects of diarrhea and slow wound healing. I am now doing a washout period of 30 days or more. (source: this post)
This person below ramped up very quickly to very high doses, which is not recommended:
My wife, with early menopause, tried with 3mg every day for 10 days for 2 months in a row. The first round she got a wicked tongue ulcer. 20 days later she did the protocol again and got swollen glands in her armpits - that stayed painful and swollen even after stopping. She also had a very light but discernable period, each month at the 30 day mark. She has stopped given how uncomfortable and swollen the underarms were… (from this discussion thread)
I just started Sirolimus last week and I’m getting very large cysts (acne) on my forehead. Has anyone developed cystic acne as a side effect of taking rapamycin
Yep. That was the main side effect for me. I got a giant red puffy zit somewhere on my body after the dose. I also started on a low dose and got the my first week on 1mg. It’s just our thing I guess
Had a surreal experience. I go see a dermatologist due to a few skin tags that happened in the last year. She looks at them carefully and immediately asks the question: were you on any kind of immunosuppressant? (Rapamycin isn’t mentioned in any of my health records). She said immunosuppressants like cyclosporine can cause the fat gland outgrowths (skin tags) like the one I have on my front head. Luckily they’re benign. As mentioned earlier, I’m very pleased with the improvement in my creatinine/eGFR and fatty liver. On the downside, I believe immunosuppression with 6mg/once a week dose is real (despite having unchanged WBC numbers) and the human life extension benefits with continuous use haven’t been demonstrated. I always liked how Rapamycin made my face a tad younger and more fresh
I probably won’t take it for the foreseeable future due to a conflict with another drug I’m taking.
I have the exact same skin tags in the exact same place. 5mg rapamycin once a week.
Anyone feel flu/cold achy symptoms the day after taking their very first does? I started yesterday w on 3gms…
There’s an association between rapamycin and interstitial disease of the lungs… keep an eye on it. Seems to be reversible when you stop the medication.
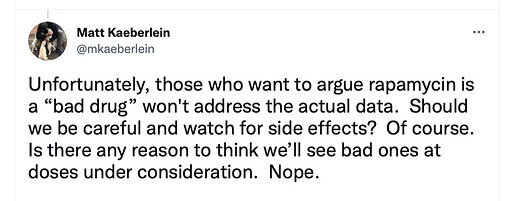
Independently, Matt Kaeberlein, Director, Healthy Aging and Longevity Research Institute University of Washington, and one of the leaders of the Dog Aging Project (studying rapamycin in dog aging) suggests this:
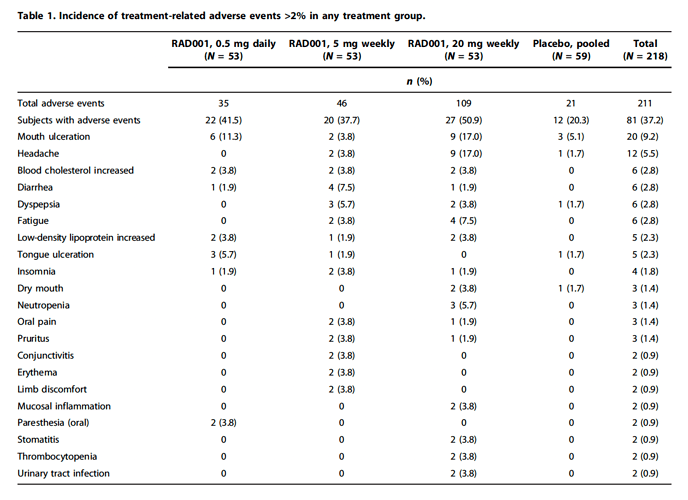
Here are the side effects seen with the rapalog (a drug almost identical to rapamycin) Everolimus (RAD001, Novartis Afinitor) in the famous Mannick 2014 clinical trial (with elderly but healthy people, dosed weekly) where it was shown to improve aging immune systems in people.
Interestingly, they reported only 1 serious adverse event in the study:
Only one severe adverse event was assessed as related to RAD001: mouth ulcers in a subject treated with 20 mg weekly RAD001.
If you are taking rapamycin, please add your own side effects experience by clicking on the “Reply” button and add in your comments below: