You added weight loss…that is associated with inhibition.
Re intervention, I haven’t settled into my thinking on this yet, haven’t dug deep enough, completed a full thought experiment, but some initial considerations.
Interestingly, the oncologist in the cancer/GFJ study I had a brief exchange with, didn’t mention CVD as a concern in his Rapamycin patients…only anemia and ILD. I am inferring on CVD here.
Have read a great many “chronic rapamycin” human studies, don’t recall much on CVD. Extrapolate in this vacuum anything about far weaker intermittent dosing?
If CVD is driven by metabolic syndrome, a “diabetic” profile, and having dysregulated glucose and TG, yet all other markers are excellent (weight, BP, HDL) then “technically” we haven’t tipped the CVD balance?
Frontiers | Rapamycin: A Bacteria-Derived Immunosuppressant That Has Anti-atherosclerotic Effects and Its Clinical Application | Pharmacology (2019)
“Several lines of evidence have demonstrated that rapamycin possess multiple protective effects against atherosclerosis through various molecular mechanisms.”
Do we defacto assume we are blunting cancer with dysregulation, therefore turn our attention to other mortality pathways?
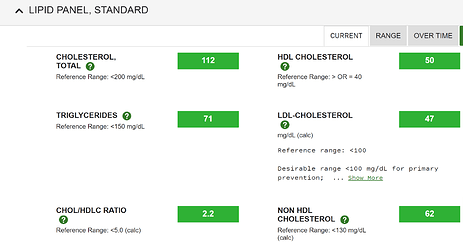
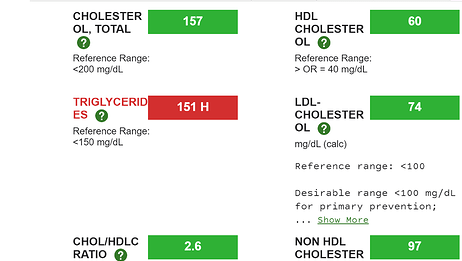
Should I get a lipid subclass analysis…sd-LDL/APOB/ox-LDL to check if tipped into atherogenic risk? TG, TG/HDL are strongly correlated to atherogenic particles.
Looking through the literature for secondary hypertriglyceridemia, cutoffs start at 150 mg/dL. My last TG was 52? Lots of runway??
Relationship between subclasses low-density lipoprotein and carotid plaque
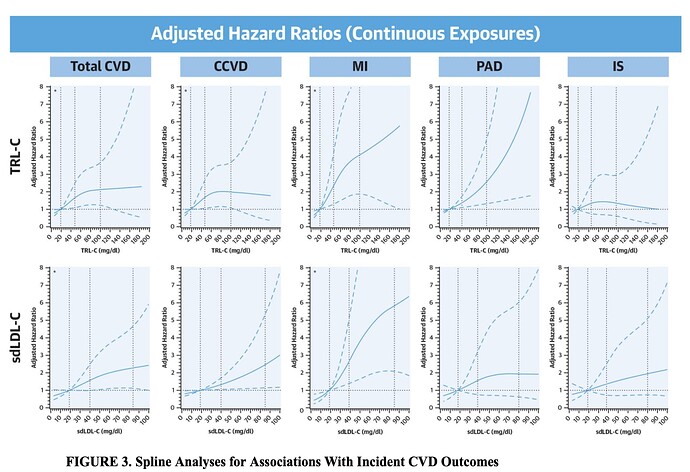
Triglyceride-Rich Lipoprotein Cholesterol, Small Dense LDL Cholesterol, and Incident Cardiovascular Disease
“The risk of both composite outcomes significantly increased across quartiles of TRL-C and sdLDL-C. TRL-C was significantly associated with myocardial infarction (MI) and peripheral artery disease (PAD) hazard ratio [HR]Q4: 3.05, PAD HRQ4: 2.58, whereas sdLDL-C was significantly associated with MI alone (HRQ4: 3.71) Both markers weakly associated with ischemic stroke (IS) Association patterns were similar for continuous exposures and, for TRL-C, among subjects with low atherogenic particle concentrations (apolipoprotein B <100 mg/dl).”
Relationship between subclasses low-density lipoprotein and carotid plaque
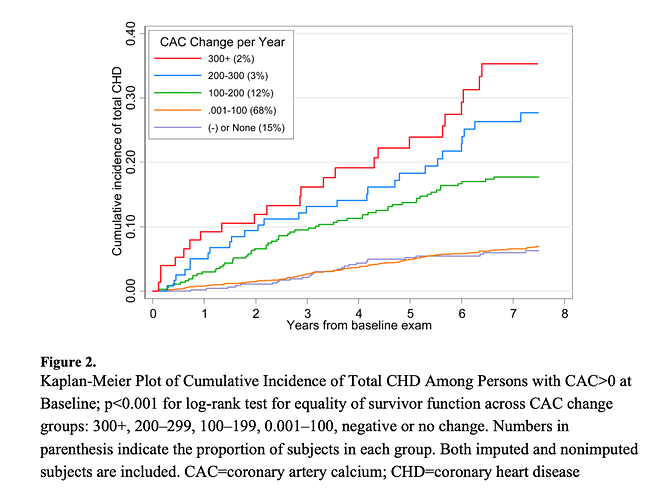
Is CT cardio “the” definitive answer?? Would I wait a year and get another CT cardio scan? Keeping progression to < 15%/yr is excellent in those with CAC > 0.
Progression of Coronary Calcium and Incident Coronary Heart Disease Events: The Multi-Ethnic Study of Atherosclerosis
Check my liver and kidney markers are improving, then that’s significant pro health positive. They are intertwined with a great many health pathways.
Do a DEXA scan and check for fat mass, visceral and subcutaneous, observe if metabolic syndrome trending? Make sure not building any fat around organs, eg NAFLD, not visible in the mirror, which is major risk factor diabetes/CVD?
Of course full inflammation markers.
“Evidence has demonstrated that elevated levels of circulating inflammatory biomarkers such as high-sensitivity C-reactive protein (hsCRP) or interleukin-6 (IL-6) independently predict the risk of atherosclerotic cardiovascular disease”
And what about “glucose”? If glucose rising yet loosing weight? Fasting glucose, hbA1c, both?
Check my pancreas marker (c peptide) to make sure beta cells are fine and not being blunted by insulin signalling, ergo, trending to diabetic?Fasting, hbA1c, AUC, cutoffs?
“HbA1c levels were positively associated with carotid atherosclerosis, as assessed by carotid IMT, in an elderly population with normoglycemia. However, fasting insulin and glucose levels were not associated with carotid IMT.”
Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk
“Hemoglobin A1c and cardiovascular disease risk factors were assessed from 1995 to 1997, and cardiovascular disease events and mortality were assessed during the follow-up period to 2003. In men and women, the relationship between hemoglobin A1c and cardiovascular disease (806 events) and between hemoglobin A1c and all-cause mortality (521 deaths) was continuous and significant throughout the whole distribution. The relationship was apparent in persons without known diabetes.”
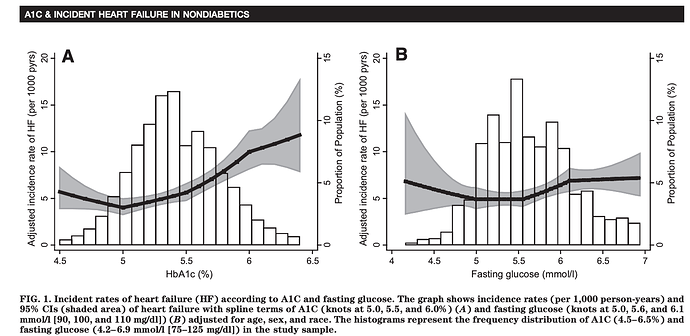
The Association of Hemoglobin A1c With Incident Heart Failure Among People Without Diabetes: The Atherosclerosis Risk in Communities Study
“Elevated A1C (5.5–6.0%) was associated with incident heart failure in a middle-aged population without diabetes, suggesting that chronic hyperglycemia prior to the development of diabetes contributes to development of heart failure. The association of A1C with risk of heart failure in our study was independent of hypertension, obesity, other traditional cardiovascular risk factors, and insulin concentration, suggesting direct effects of hyperglycemia on the development of
heart failure”
My hbA1c is 5.0…more runway??
If actual true anemia, then what, take IV iron therapy?
And if crossed into risky lymphopenia, does one react, or consider it rejuvenation of HSC for better immune function?
The ITP didn’t intervene and “treat” the mice when dysregulated on Rapamycin, yet they lived longer.
Can Dr B be wrong, some of these dysregulated markers aren’t “benevolent”? He claims below (2019 paper) “no hyperglycemic effects or rapamycin/everolimus in healthy people”?
Reports are now he’s taking 2mg/day? Surely, this is going to significantly dysregulate glucose and lipids, venturing into “chronic” vs “intermittent” preaching.
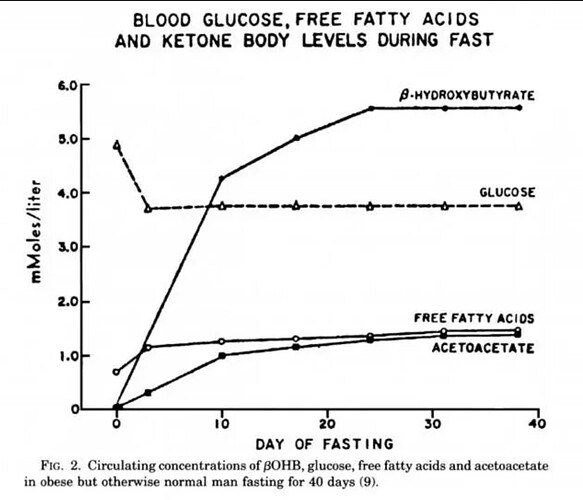
Fasting and rapamycin: diabetes versus benevolent glucose intolerance (2019)
“No hyperglycemic effects of rapamycin/everolimus have been detected in healthy people. For antiaging purposes, rapamycin/everolimus can be administrated intermittently (e.g., once a week) in combination with intermittent carbohydrate restriction, physical exercise, and metformin.”
“Hyperglycemia may be a marker of beneficial processes, given that rapamycin ameliorates nephropathy, despite elevating blood glucose levels in a mouse model of type 2 diabetes”
“Furthermore, a mechanistic study in humans showed that prolonged treatment with rapamycin causes hyperglycemia by decreasing insulin production, and insulin production depends on mTORC1. Thus, inhibition of mTORC2 by rapamycin has not yet been proved in humans”
That dosen’t seem true:
In human endothelial cells rapamycin causes mTORC2 inhibition and impairs cell viability and function
“A prolonged treatment with rapamycin impairs endothelial function and hinders cell viability. Endothelial damage seems dependent on mTORC2 inhibition”
More Dr B:
"Lamming et al. concluded that rapamycin prolongs life span, despite inducing diabetes-like symptoms. As I previously discussed, perhaps life span is extended “owing to,” not “despite,” these symptoms. Once again, whereas type 2 diabetes shortens life span, rapamycin prolongs it (despite, or maybe owing to, benevolent metabolic alterations).
At the end of the day, living longer for humans is all about all cause mortality reduction.
For humans, I don’t think we can tip the pendulum all the way over to single minded cancer blunting like the wild type mice, and must consider ALL mortality pathways.