You might also consider making a liposomal solution. Look it up. I’ve done it before with vitamin c and others.
I have the same problem too, I don’t have the knowledge of drug chemistry so I am struggling for making solution/tablet/gel…
I plan to read the following book to fill up my knowledge gap, I just finished the first 3 chapter, it’s easy to read if you have biochemistry background.
An Introduction to Medicinal Chemistry by Graham Patrick
That sounds cool, do we need advanced tools to make liposomal solution?
Don’t get me wrong, I just took my weekly rapamycin this morning. Im just saying we’re just on the edge of available evidence taking weekly rapamycin for longevity. We can be confident it’s safe, we’ve got animal data for longevity, and that’s great. But longevity effects of injected seems like you’d be flying blind.
I may be wrong, but I thought Rapa needs to be enteric coated to protect from stomach acid?
Recommended reading related to bioavailability of orally taken rapamycin:
Here: New Peter Attia interview w/Matt Kaeberlein, inferior bioavailability of encapsulated rapa
Here: Rapamycin and NanoCrystal Formulations
Here: Bioavailability of Rapamycin From Compounding Pharmacy
I use a Blend Tec (High speed) blender to make liposomal supplements. I don’t do this for rapamycin…but I do take it with GF juice to increase bioavailability.
World_Traveler, Do you mind sharing your powder source? And, can you give more information about the good results you’ve had with your rapa cream? Thanks.
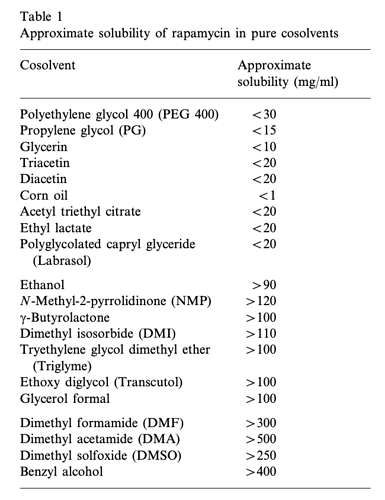
Most compounds w weak ethanol and no water solubility usually suspend in peg400. This is common for stuff like sarms/ped5 inhibitors.
I have powder headed my way. Ill let you know if peg 400 works
New plan.
Make a small batch of solution with rapa powder in ethanol/PEG. Keep refridgerated.
Make up capsules as required - measure solution into: size 0 clear licaps® Liquid-Filled Capsules
Put these size 0 ‘liquid safe’ caps inside: size 000 DRcaps® delay release acid resistant
Just waiting for the caps to arrive.
Hopefully the rapamycin in solution and the use of delayed release acid resistant capsules will avoid potential issues with bioavailability.
Are you getting the rapamycin powder analyzed for purity and and common contaminants? @Mac wrote a good post on his process for doing this, and his results: Sirolimus Powder - 3rd party analysis
Also, FYI: I Do Not Recommend buying rapamycin powder from this Chinese seller (Zhejiang Multinpharma)
No, I’m not getting the powder tested despite being aware of the risks.
Turns out I bought from the same supplier as MAC. People have shared purity reports of other compounds that have been supplied by them and as far as I can tell they are fairly consistent.
Just had capsules delivered today - didn’t realise size 000 would be quite that large!
Are you aware how small an amount of 100mg of purified rapamycin is?
See attached photo;
100mg of purified rapamycin;
I found a video about how to make liposomes, for people want to make their own homemade liposomal ingredient, the procedure looks very easy.
The materials and tools required:
- Lecithin powder
- Active ingredients (rapamycin, trehalose, ect.)
- High speed blender (as @bizgoz mentioned)
- Ultrasonic cleaner
I plan to make liposomal trehalose, liposomal rapamycin cream, liposomal dasatinib face cream and liposomal RiverTown Hair Repigmentation formulation Reverse Gray Hair, Hair Repigmentation
Thanks for sharing this cool technique.
Can confirm Rapamycin is soluble in Peg400. I added 300mg to 30ml PEG 400. Heated in microwave 20 seconds and it dissolved and has been stable in solution for @ 10mg/ml.
Note: I added .2ml benzyl alcohol to maintain sterility
This will be a long post… but please read in its entirety!
Biochemist here, keep in mind that there are a few factors you should consider when using an injectable solution. It was my job for years to formulate injections for mice, and while I don’t recommend you homebrew drugs, I have a feeling you’re gonna do it anyways, so might as well give a guide.
-
First, consider equivalent dose. For instance, consider an oral drug that is only 1% bioavailable. That means out of a hypothetical dose of 1 mg, you will be getting 0.01 mg circulating in your bloodstream. This is why oral doses are quite high, as it is mostly to compensate for poor absorption and effective dose. In most cases, an injected drug is 100% bioavailable. This is especially so for a lipophilic drug such as rapamycin and its analogues when suspended in a lipophilic carrier such as PEG 400 or oil. You bypass first-pass metabolism, or unmetabolized drug that simply passes through you in stool or urine. Therefore, it would be important to reference what a 6-7 mg dose of oral rapamycin translates to in regard to bloodstream circulation, and aim to mimic that ballpark in your injected dose.
-
Second, lipophilic injections are typically sustained doses. With an oral dose of a typical drug, peak levels are reached usually within a couple hours, and then peters off rapidly. Rapamycin is unique in that its oral half life is already long, about 3 days for elimination. An injected solution, if it is intramuscular or subcutaneous, will likely last much longer than that, and may reach an even higher peak due to the increased bioavailability.
-
Injection vehicle properties affect release profile. Selecting the injection vehicle can prolong the release profile of a drug. For instance, a highly lipophilic drug suspended in a slightly lipophilic vehicle will have a quicker release time than in a highly lipophilic vehicle. Rapamycin is highly lipophilic, so that’s already a given. Furthermore, the viscosity will also have an impact on release time, with the more viscous solution being the more slow to release. The best example of this is comparing suspensions in MCT oil versus castor oil; castor oil prolongs the release of an injection considerably, but it also flows like glue.
-
Blood levels must be closely monitored to be within the therapeutic window. This is the most important factor. The dose is the poison. Typically, blood levels of a particular drug are closely monitored in a patient to ensure that circulating levels do not exceed a certain threshold, called the therapeutic window. Going outside that window can either mean ineffectiveness if you dose too weakly, or serious harm if you dose too strongly. Fortunately, rapamycin blood testing is available! Usually we monitor blood levels for a peak and trough level, based on the half life. So, if one were to inject rapamycin, which has a half-life of about 3 days, I would hazard a guess that an IM peak would be reached somewhere between 1-3 days after injection. So, I suppose one could take a blood test at 2 days after injection and another right before the next injection for a trough level to ensure you aren’t exceeding the safe baseline. Also keep in mind that consecutive doses will accumulate raise your baseline over time until a steady-state is reached, so after 3-5 doses it would be good to do another trough check.
Considering that rapamycin is preferred to be dosed and eliminated quickly, I wouldn’t recommend injections whatsoever. But! This is a forum of mad scientists, so if you’re gonna do it, just please consider these points. The whole point of weekly dosing is that daily or constant dosing gives you quite detrimental side effects (we aren’t organ transplant patients, after all).
So, if I were to hypothetically do it (even though I don’t condone it), I would suspend in MCT oil or similar (viscosity ~27 mPa.s compared to PEG 400 between 90-110 mPa.s), lowball the dose at around 1 mg, and monitor the peak and trough level via blood test after 2 days of initial dose and right before the next dose. If the dose looks too low, I would try to adjust the dose and do another peak/trough test until it looks good. Then, after about a month and a half, I would re-check the trough to see what the steady-state level is, and reduce if necessary.
EDIT: Apparently some madman did it already… see here.
Granted, it’s still n=1, but apparently the guy tolerated a 15 mg injection. Absolutely insane.
Thanks so much for posting some good in depth information. @MAC has actually been dosing this regularly for past six months or so and seems to be doing pretty well. We don’t recommend it, but people are trying new things and reporting their results.
What are your opinions on using DMSO as the main reagent for the formulation?
That @MAC guy is wild! I saw his post after I had replied. Very impressed by how thorough he is about monitoring his treatment, though he does a lot of other things I have concerns about.
Regarding DMSO, it’s not an ideal vehicle due to its cytotoxicity. Most pharmaceutical formulations only use DMSO to aid in solubility, and typically around 10% v/v. He seems to be injecting it in 100% DMSO, and I’m surprised he is tolerating it so far.
Most have injection site reactions from that much DMSO, and I believe someone also mentions that to him. What I suspect is that @MAC may have used degraded DMSO over time. 100% DMSO is very light-sensitive, and degrades rapidly. I do not know if he stores his solution in an amber or opaque bottle, but one of his pictures shows a regular glass jar. The freeze/thaw cycles might have also contributed to degradation, and I believe he also states he uses a “glass vial” of sorts. For a multi-dose container, this isn’t ideal as exposure to humidity/oxygen/contamination from the air can hasten the “spoilage” of the solution, which is why sealed vials with septa mats are used.
He mentions that he had such intense pain when he began injecting that he could barely walk, which gradually reduced over time. That is not normal, and likely due to the near-pure DMSO he was injecting. He may have damaged his injection site tissues to the point where he may have built up a “tolerance” only because he has become less sensitive to the pain. The rapamycin might also be irritating him, but I’d consider altering his formula.
Perhaps he could try out a different formulation without DMSO to see if it makes a difference. I’d personally try to solubilize in MCT oil first, and only add a maximum of 10% v/v DMSO if solubility is an issue. Typically, benzyl benzoate between 10-40% is also added as a preservative and would help stabilize rapamycin.
I am also very concerned as to whether or not he is using aseptic/sterile technique in his preparations. I get the impression he is just mixing it and injecting it… which is terrifying to me.
Pure DSMO injections as blank reference cause no pain. It’s the rapamycin bolus to the tissue. As I continued my protocol, it appears my tissues became accustomed to the cellular rapamycin already in circulation, and lately, IM injections are relatively quite painless +/-
Currently this far along, there are no ongoing visible (bruising, etc) or physiological signs (gait, soreness) or symptoms related to the IM injection site re possible “tissue” damage, other than typical sting and small bump at the injection site. And lately, stinging and bump is often completely lacking.
The DSMO is stored in original dark glass bottle and blackout container. Prepared doses are frozen until taken. See other post re preparation protocol.
https://sci-hub.hkvisa.net/10.1016/s0378-5173(00)00617-7
Please suggest a high solubility, high concentration, safer solution, that allows target dose and VERY low injection dosing volume (fraction of mL).
Preferred, what is your reference? I am taking rapamycin for only one reason: longevity enhancement.
What is the rapamycin dosing/AUC that delivers our objective…translation of countless mice longevity studies where mice exposed to ever increasing doses live longer, to human longevity escapism? Are you suggesting the answer to this question?
You realize therapeutic rapamycin dosing (cancer/transplant) is a continuous high AUC dosing protocol? Trough levels (AUC proxy) are maintained for years at 5-15 ng/mL? These are not an “eliminated quickly” protocol.
Injections are one of the most commonly used methods of delivering drugs in the world. They might have less compliance than say oral, but this is not a compliance forum…this is a biohacker/longevity forum.
As you know, bioavailability of IM and IV are almost 100%.
Recent FDA approved sirolimus formulation for IV delivery:
I am just running an outside the box sortie experiment…no idea where this goes, benefits, outcome, or duration. Just sharing my n=1 and the rationale behind it, and hoping to move the needle.