Are you aware how small an amount of 100mg of purified rapamycin is?
See attached photo;
100mg of purified rapamycin;
Are you aware how small an amount of 100mg of purified rapamycin is?
See attached photo;
100mg of purified rapamycin;
I found a video about how to make liposomes, for people want to make their own homemade liposomal ingredient, the procedure looks very easy.
The materials and tools required:
I plan to make liposomal trehalose, liposomal rapamycin cream, liposomal dasatinib face cream and liposomal RiverTown Hair Repigmentation formulation Reverse Gray Hair, Hair Repigmentation
Thanks for sharing this cool technique.
Can confirm Rapamycin is soluble in Peg400. I added 300mg to 30ml PEG 400. Heated in microwave 20 seconds and it dissolved and has been stable in solution for @ 10mg/ml.
Note: I added .2ml benzyl alcohol to maintain sterility
This will be a long post… but please read in its entirety!
Biochemist here, keep in mind that there are a few factors you should consider when using an injectable solution. It was my job for years to formulate injections for mice, and while I don’t recommend you homebrew drugs, I have a feeling you’re gonna do it anyways, so might as well give a guide.
First, consider equivalent dose. For instance, consider an oral drug that is only 1% bioavailable. That means out of a hypothetical dose of 1 mg, you will be getting 0.01 mg circulating in your bloodstream. This is why oral doses are quite high, as it is mostly to compensate for poor absorption and effective dose. In most cases, an injected drug is 100% bioavailable. This is especially so for a lipophilic drug such as rapamycin and its analogues when suspended in a lipophilic carrier such as PEG 400 or oil. You bypass first-pass metabolism, or unmetabolized drug that simply passes through you in stool or urine. Therefore, it would be important to reference what a 6-7 mg dose of oral rapamycin translates to in regard to bloodstream circulation, and aim to mimic that ballpark in your injected dose.
Second, lipophilic injections are typically sustained doses. With an oral dose of a typical drug, peak levels are reached usually within a couple hours, and then peters off rapidly. Rapamycin is unique in that its oral half life is already long, about 3 days for elimination. An injected solution, if it is intramuscular or subcutaneous, will likely last much longer than that, and may reach an even higher peak due to the increased bioavailability.
Injection vehicle properties affect release profile. Selecting the injection vehicle can prolong the release profile of a drug. For instance, a highly lipophilic drug suspended in a slightly lipophilic vehicle will have a quicker release time than in a highly lipophilic vehicle. Rapamycin is highly lipophilic, so that’s already a given. Furthermore, the viscosity will also have an impact on release time, with the more viscous solution being the more slow to release. The best example of this is comparing suspensions in MCT oil versus castor oil; castor oil prolongs the release of an injection considerably, but it also flows like glue.
Blood levels must be closely monitored to be within the therapeutic window. This is the most important factor. The dose is the poison. Typically, blood levels of a particular drug are closely monitored in a patient to ensure that circulating levels do not exceed a certain threshold, called the therapeutic window. Going outside that window can either mean ineffectiveness if you dose too weakly, or serious harm if you dose too strongly. Fortunately, rapamycin blood testing is available! Usually we monitor blood levels for a peak and trough level, based on the half life. So, if one were to inject rapamycin, which has a half-life of about 3 days, I would hazard a guess that an IM peak would be reached somewhere between 1-3 days after injection. So, I suppose one could take a blood test at 2 days after injection and another right before the next injection for a trough level to ensure you aren’t exceeding the safe baseline. Also keep in mind that consecutive doses will accumulate raise your baseline over time until a steady-state is reached, so after 3-5 doses it would be good to do another trough check.
Considering that rapamycin is preferred to be dosed and eliminated quickly, I wouldn’t recommend injections whatsoever. But! This is a forum of mad scientists, so if you’re gonna do it, just please consider these points. The whole point of weekly dosing is that daily or constant dosing gives you quite detrimental side effects (we aren’t organ transplant patients, after all).
So, if I were to hypothetically do it (even though I don’t condone it), I would suspend in MCT oil or similar (viscosity ~27 mPa.s compared to PEG 400 between 90-110 mPa.s), lowball the dose at around 1 mg, and monitor the peak and trough level via blood test after 2 days of initial dose and right before the next dose. If the dose looks too low, I would try to adjust the dose and do another peak/trough test until it looks good. Then, after about a month and a half, I would re-check the trough to see what the steady-state level is, and reduce if necessary.
EDIT: Apparently some madman did it already… see here.
Granted, it’s still n=1, but apparently the guy tolerated a 15 mg injection. Absolutely insane.
Thanks so much for posting some good in depth information. @MAC has actually been dosing this regularly for past six months or so and seems to be doing pretty well. We don’t recommend it, but people are trying new things and reporting their results.
What are your opinions on using DMSO as the main reagent for the formulation?
That @MAC guy is wild! I saw his post after I had replied. Very impressed by how thorough he is about monitoring his treatment, though he does a lot of other things I have concerns about.
Regarding DMSO, it’s not an ideal vehicle due to its cytotoxicity. Most pharmaceutical formulations only use DMSO to aid in solubility, and typically around 10% v/v. He seems to be injecting it in 100% DMSO, and I’m surprised he is tolerating it so far.
Most have injection site reactions from that much DMSO, and I believe someone also mentions that to him. What I suspect is that @MAC may have used degraded DMSO over time. 100% DMSO is very light-sensitive, and degrades rapidly. I do not know if he stores his solution in an amber or opaque bottle, but one of his pictures shows a regular glass jar. The freeze/thaw cycles might have also contributed to degradation, and I believe he also states he uses a “glass vial” of sorts. For a multi-dose container, this isn’t ideal as exposure to humidity/oxygen/contamination from the air can hasten the “spoilage” of the solution, which is why sealed vials with septa mats are used.
He mentions that he had such intense pain when he began injecting that he could barely walk, which gradually reduced over time. That is not normal, and likely due to the near-pure DMSO he was injecting. He may have damaged his injection site tissues to the point where he may have built up a “tolerance” only because he has become less sensitive to the pain. The rapamycin might also be irritating him, but I’d consider altering his formula.
Perhaps he could try out a different formulation without DMSO to see if it makes a difference. I’d personally try to solubilize in MCT oil first, and only add a maximum of 10% v/v DMSO if solubility is an issue. Typically, benzyl benzoate between 10-40% is also added as a preservative and would help stabilize rapamycin.
I am also very concerned as to whether or not he is using aseptic/sterile technique in his preparations. I get the impression he is just mixing it and injecting it… which is terrifying to me.
Pure DSMO injections as blank reference cause no pain. It’s the rapamycin bolus to the tissue. As I continued my protocol, it appears my tissues became accustomed to the cellular rapamycin already in circulation, and lately, IM injections are relatively quite painless +/-
Currently this far along, there are no ongoing visible (bruising, etc) or physiological signs (gait, soreness) or symptoms related to the IM injection site re possible “tissue” damage, other than typical sting and small bump at the injection site. And lately, stinging and bump is often completely lacking.
The DSMO is stored in original dark glass bottle and blackout container. Prepared doses are frozen until taken. See other post re preparation protocol.
https://sci-hub.hkvisa.net/10.1016/s0378-5173(00)00617-7
Please suggest a high solubility, high concentration, safer solution, that allows target dose and VERY low injection dosing volume (fraction of mL).
Preferred, what is your reference? I am taking rapamycin for only one reason: longevity enhancement.
What is the rapamycin dosing/AUC that delivers our objective…translation of countless mice longevity studies where mice exposed to ever increasing doses live longer, to human longevity escapism? Are you suggesting the answer to this question?
You realize therapeutic rapamycin dosing (cancer/transplant) is a continuous high AUC dosing protocol? Trough levels (AUC proxy) are maintained for years at 5-15 ng/mL? These are not an “eliminated quickly” protocol.
Injections are one of the most commonly used methods of delivering drugs in the world. They might have less compliance than say oral, but this is not a compliance forum…this is a biohacker/longevity forum.
As you know, bioavailability of IM and IV are almost 100%.
Recent FDA approved sirolimus formulation for IV delivery:
I am just running an outside the box sortie experiment…no idea where this goes, benefits, outcome, or duration. Just sharing my n=1 and the rationale behind it, and hoping to move the needle.
I recently saw your post regarding that, and I am impressed. Everyone has a different tolerance, so as long as it doesn’t seem to cause you any issues it should be OK to continue. Just keep an eye out for any signs of cytotoxicity, as those symptoms are typically more long-term side effects.
Good to hear, I was a bit thrown off by that glass jam jar. I’m assuming the poly bag that you store your syringes in is also blackout.
Regarding a viable vehicle, I don’t know. That’s why I said I’d personally try to solubilize in MCT oil, as I’m curious as to what the solubility limit would be. Corn oil is quite a piss-poor oil solvent, and I don’t believe anyone in pharma uses that as a vehicle (not sure why they included it in that paper).
It would have been more helpful if they tried to solubilize in common oily injection vehicles such as grapeseed, cottonseed, or MCT oil, but I suppose I have to find out myself at some point. I am considering compounding some solutions as an experiment, particularly with castor oil which has great sustained-release properties. I cannot deny your argument in favor of injections instead of the oral route, so I would like to help out in that regard since it’s in my field of work. I’m a young scientist, though (in other words, broke), so it may take me a bit to gather the resources.
Interesting that benzyl alcohol can solubilize rapamycin better than DMSO, though! Benzyl alcohol/benzyl benzoate are common preservatives to add to injectable formulations. This makes me think that a blend of 10% DMSO, 10-40% benzyl benzoate/alcohol, and a carrier oil like MCT or castor oil might just work, as I had initially speculated.
At the concentrations you are using (37.5 mg/mL), I think it may be possible to formulate a depot injection, similar to testosterone cypionate. I would have to do a calculation referencing the pKa and pharmacokinetics of rapamycin to estimate how such a depot injection would perform. I’ll definitely keep you posted if I have the time to do it. Quite exciting!
When I stated that it is preferred to be dosed and eliminated quickly, I am referring to the nasty side effects of long-term daily dosing experienced by organ transplants. Namely, hyperglycemia/hypertriglycerimia, weakened immune system, and increased rate of infections.
This is why the weekly/periodic dosing schedule exists - to avoid the side effects while retaining the benefits. The longevity benefits are thought to be due to mTORC1 inhibition, but rapamycin also has the off-target of mTORC2 inhibition, which is the likely model for why the aforementioned side effects occur.
By injecting high-dose rapamycin, you are effectively putting yourself at risk for these side effects. Granted, I agree with you that the weekly oral dosing is suboptimal, and there certainly is a need for better therapies.
I acknowledge that such dosing protocols exist that are comparable to what you are currently doing, but we are not cancer or organ transplant patients. Yes, those patients do take rapamycin for years, but it is quite a miserable experience for a lot of them.
I am in no way disparaging you for what you are doing. I think you’re quite the badass biohacker! I’m just expressing my own concerns over such a therapy as a clinical scientist, but I don’t think the fact that I wear a white labcoat to work should invalidate your approach to your own personal health.
It is indeed interesting that they are rolling out an IV protocol for rapamycin. But keep in mind, IV is fundamentally different from IM. IV is considered a short-release route of administration, while IM is a sustained-release. IM must first diffuse through muscle tissue and then into the bloodstream, while IV just goes directly into the bloodstream. As such, the peak concentration is reached far more quickly in IV, and also gets eliminated that much more quickly than IM.
Furthermore, it seems they are doing one dose per week for two weeks, then one week off. So, in effect, it isn’t that much different from the high-dose weekly protocols that some have on this forum.
better to take it with 200 to 400 mg ketoconazole available(unless they are out of stock) from india like Reliable… where i bought mine.
even though rapamycin has greater solubility in benzyl alcohol i have read that it is not as readily released from that as it is using some other agents in which it has a lower solubility than benzyl
FWIW use DMSO dissolved and carry the rapamycin.
yes i have been making an injectable solution or whatever u want to call it from powder from China.Trying to make nano micellar solutions. Have read that Nanoemulsions are even better though difficult and need be much more precise than just micellar solutions. Seems to me that just taking it orally esp if using just the straight powder is a real waste and doubt that sublingual is going to be any help either.
just how would u go about looking for signs of cytotoxity or whatever without a lot of expense and going thru a royal pain in the ass ! ALso to the remark
" I wouldn’t recommend injections whatsoever. " Studies done with mice say just putting it with their food had no effect at all while intraperiontal injections which are not really suitable for humans i would not think because for one - horrible unbearable pain, had much effect. But for sure subcutaneous, im or iv if u can do it yourself - like i mean hit a vein which i can’t, injections would all be way better than oral and save u money as rapamycin even as wholesale powder is NOT cheap.
’
So, to address your first response regarding benzyl alcohol - yes, it has slower release time. This is because “like dissolves like” applies here.
The more similar a compound’s kinetics and properties are to its solvent (i.e. lipophilicity, surface charge/area, viscosity), the more readily it will dissolve in said solvent and reject others. This is the basis for most long-acting injections like testosterone, which is usually esterified into compounds like testosterone cypionate, which is many times more lipophilic than plain testosterone and thus will separate more slowly from its preferred solvent, oil.
Now, whether or not you want sustained, gradual release of rapamycin like this is debatable. I have no idea about the pharmacokinetics of such an injectable preparation of rapamycin, but if it ends up being similar to a long-acting injectable, you’d essentially be replicating a daily dosing regimen that cancer/transplant patients use, which has its own issues.
To address your second reply regarding nanoemulsions, I think you may be misunderstanding the purpose of such preparations. They are not typically intended for injection.
Injectable preparations are considered 100% bioavailable. This is because you use a parenteral route, bypassing saliva, bile acids, and liver metabolism. In other words, you avoid anything that could potentially degrade or inactivate your active drug.
Nanoemulsions are intended to make up for the limited bioavailability of oral preparations. Most drugs have poor solubility in aqueous solvents, especially so for rapamycin, so the idea is to encapsulate them in a carrier lipid which is also miscible with water; this allows the drug to be more readily absorbed by the intestines.
Creating nanoemulsions, or even micellar ones, requires very precise and controlled laboratory conditions. It isn’t something that can be achieved at home, unless you bootleg some specialized lab equiment (which you usually need a license for, even secondhand).
So, for IM and SC, nanoemulsions wouldn’t make much sense since you’re not injecting into aqueous environments. For IV, it would matter since blood is aqueous, so you may see nanoemulsions used here in order to bridge the aqueous solubility issue. Most people here seem to be aiming for IM or SC, which is far easier to prepare and use than IV. Furthermore, IV preparations need to be used fresh every time since aqueous solvents have very short shelf lives, so it would be extremely difficult to do at home.
And yes, taking the raw powder orally, even when packed into a capsule, is basically like ingesting nothing. Most of it will be destroyed in bile acids, and most capsules marketed as “enteric-coated” are actually fake, since you’d need a pharmaceutical license to make enteric capsules due to regulations in the US. However, I do have methods for preparing enteric-coated tablets at home which can bypass the stomach acids, so let me know if you’d like a how-to for that. I can’t guarantee that it’d have the same performance as the factory-prepared ones, but you can get pretty damn close.
Just keep in mind… making your own medicine is illegal. So, if you purchase any medicine-making equipment, it will put you on a list. The FDA and DEA do not fuck around with homemade drugs. If they suspect you are making drugs of any kind, be wary of getting raided. Usually most people will fly under their radar, but if you have an online record of buying pharmaceutical equipment (ESPECIALLY tablet/pill presses) without a license… yeah… they might start monitoring you. Buying the ingredients is fine, but buying equipment implicates you as a manufacturer and/or distributor.
When your tissues start to necrose, deteriorate, or other similar effect. Cytotoxic just means that cells begin to malfunction and die. I’m assuming you’re talking with regard to DMSO, which is generally safe when kept to a concentration of 10% or lower. However, even at 100%, you should be fine as long as you rotate sites and keep injection volume low. It just tends to sting like a bitch, but tolerance can vary between individuals such as with MAC, who has no reaction to it. Cytotoxicity really only appears if the same site is exposed repeatedly over a long period of time. To date, only a few cases of this have been reported from people drinking bottles of the stuff for some reason.
This is just a disclaimer that I usually have to put because of my background. The pharmacokinetics of injectable rapamycin in humans, aside from a few IV trials, has not been well-investigated. We have no idea how IM or SC administration would perform. Therefore, I cannot recommend it.
The reason I still give advice is because of harm-reduction. That is, if people are going to self-experiment anyways, they should at least know how to do it properly in order to reduce the overall risk.
I suppose the economics of it would be better, but keep in mind what I mentioned earlier regarding pharmacokinetics. Saving money per dose is a rather tiny detail compared to the overall unknown of such a radical treatment. I’d be more concerned about the impact on your overall health rather than price per bioavailable dose, since the former can end up costing you far more than you’d save on a kilo of powder.
most all tests with animals are injections and much about the success of that way but very little or none the other way being oral. people are animals/whats good for the goose is good for the gander to put it in old simplified wise tales language.
Dan - almost all the rapamycin mouse studies have been using oral dosing of rapamycin. We have a full list of the studies here if you want to learn about them: List of all the Mouse Studies Showing Rapamycin Lifespan Extension
You really don’t seem to understand much about rapamycin and the risks that you are taking, and don’t seem to have much interest in learning about them. You are taking extremely high risks and the outcome is not likely to be good, or a longer life. I think what you are doing is really reckless. The contributor who posted above is a biochemist who works in this field and works daily with these types of drug issues he discusses above. If you don’t want to listen to educated, thoughtful feedback from people on rapamycin use, this may not be the forum for you. We don’t want to see anyone hurt or die from reckless rapamycin use.
i have been doing it for a year or so and from the many articles on internet i use propylene glycol, polysorbate 80=tween 80 and alcohol of which i use isopropyl as it is cheaper but u can use either that or ethyl if u want to pay more. I NEVER ever had any plans to do it orally since it is much more effective and superior and sensible to do it by injection as most all animal and mice/rat tests are done by injection and compared to oral its a no brainer. I also bought mine from a chinese supplier of which i trust from buying other chemicals etc. for over 8 years; i have had results and side effects and blood tests results just as to be expected from internet reports so i feel confident my rapa is sufficiently good . if u insist on doing it the inferior oral way i have briefly read similar scientific reports on internet which have shown directly how to formulate it to be significantly superior to the commercial rapammune or however u spell it oral product… i also do mine with 200mg ketoconazole every 5 days averaging about 20 to 30mg rapa with some breaks and delays because of the horrible mainly mouth sores problem enough so as to even make it quite difficult to eat. Finally i said well i am going to wait till all these mouth sores are gone before doing any more which took over 2 months. i can just imagine what these mice and rats are going thru since scaling to them they were doing much more than my measly 20 to 30 mg. and not only that every day! Now even so i am planning to cut back and have to say only 7 to 10mg every 5 days with ketoconazole. Even that measly tiny amount has been enough to still get mouth sores though at least for me.
,
i have read articles on mouse studies and most all of them were intra-periontal injections which are usually not done to humans. The foremost article i read when they just put it with their food by what’s the word ‘gavage’ or something and the results were not effective. so i guess it just depends upon what articles u choose to read. My thinking is always rational and logical and scientific and relative probabilities. The chinese company i use i have dealt with them for over 8 years buying other chemicals so i am confident enough with them. Sure some people have had bad luck from chinese vendors but china is a huge huge country so ofcourse there are going to be some undesirable but i will bet if u take those who have had success is much much greater. To you and others i guess u just don’t trust any foreign country. Do u go thru all that testing etc etc from products from usa vendors - i doubt it. Anyway using sensible probabilities i would say i am taking less chance of undesirable issues than someone who risks death and serious injury from driving an automobile over 10,000 miles a year. As far as scientific and doctors etc who u seem to think know much more why don’t ask one of them the answer to the simple question of 2nd derivative of exp(sqrt(x)) wrt x. And see how many of these ‘bright’ doctors can’t answer that right off the bat or in small amount of time. Yea they are really bright.! Anyway i am not saying anyone else has to do the rapamycin the way i do it. I am just giving my take on the issue. And i even said if u insist on doing orally then go ahead. And i am only doing it for myself only and NOT selling or propose to ever sell it to anyone else.
9x(
If your rapamycin powder is accurately measured, 7 to 10mg with ketoconazole it could be equivalent to up to 40mg to 56mg every 5 days, so an average of almost 10mg/day. This is much higher than the transplant organ patients use (and more at the levels used in cancer studies) and so you are likely getting very significant immune system suppression on an ongoing basis. This is very high risk.
Below are some examples in a high dose (e.g. 10mg/day) everolimus study for cancer patients where there were multiple life-threatening situations, including a relatively sudden death of a 27 year old woman due to e-coli sepsis.
Rapamycin is not a risk-free drug, especially as you increase doses above the regular 5 to 8mg dosing once per week level.
The most common Adverse Effects (AEs) of everolimus therapy were laboratory abnormalities (100% of patients) and infection complications (83 episodes in 15 patients). Infectious episodes of pharyngitis (67%), diarrhea (44%), stomatitis (39%), and bronchitis (39%) were the most common infections. They were mostly mild or moderate in severity (grade 1–2).
In two cases, life-threatening conditions related to mTOR inhibitor treatment were encountered. The first was classified as grade 4 pleuropneumonia and Streptococcus pneumoniae sepsis, whereas the second was classified as death related to AE (grade 5) Escherichia coli sepsis.
A 27-year-old woman with TSC was started on everolimus
treatment because of AML of the left kidney
(60 Å~ 48 Å~ 36mm in size). The other signs of TSC were
facial angiofibroma, hypomelanotic macules of the skin,
and shagreen patch. The diagnosis of TSC was made
12 years earlier when the patient underwent nephrectomy
because of a large tumor of the right kidney. The
patient received everolimus at a dose 10 mg/day and the
trough concentrations of the drug ranged from 4.08 to
5.08 ng/ml. After 3 months of everolimus therapy, a
reduction in AML was observed (40 Å~ 31 Å~ 20mm in
size). During treatment, hypercholesterolemia (309 mg/
dl) and transient leukopenia (3.2 Å~ 109/l) with neutropenia
(1.34 Å~ 109/l) was observed. She also reported
oligomenorrhea. After a gynecological consultation, a
functional ovarian cyst was identified and contraceptives
were prescribed. However, 2 weeks later, she was
admitted to the gynecological unit because of subabdominal
pain and an ovarian cyst (64 Å~ 53mm in seize)
on ultrasound examination. Torsion of the ovarian cyst
was suspected. On the day of admission, WBC was
9.2 Å~ 109/l, the absolute neutrophil count (ANC) was
6.6 Å~ 109/l, the hemoglobin level was 10.8 mg/dl, the
PLT count was − 275 Å~ 109/l, and the C-reactive protein
concentration was 8.0 mg/dl (normal < 5.0 mg/dl). The
patient was advised to continue intake of contraceptives
and everolimus. The next day, the general condition of
the patient aggravated. Her blood pressure was low (85-
/50mmHg). Her WBC and ANC decreased (WBC
−2.4 Å~ 109/l, ANC − 1.8 Å~ 109/l), whereas the hemoglobin
level (11.0 g/dl), the PLT count (185 Å~ 109/l), and coagulation
tests were normal. Computed tomography of the
abdomen and pelvis showed AML of the left kidney (size
as in the previous examination), an ovarian cyst measuring
65 Å~ 50 Å~ 40 mm, and fluid in the retroperitoneal
space with density of the blood. Further aggravation of
her general condition was observed. The patient was
transferred to the ICU and she died after 2 h with
symptoms of shock and multiorgan failure. Blood and
urine cultures collected when she was in the ICU were
positive for Escherichia coli.
Complications of mammalian target of rapamycin inhibitor anticancer treatment among patients with tuberous sclerosis complex are common and occasionally life-threatening
What the hell… you’re injecting with “cheap” isopropanol?
Dear God, when you say “cheap” I hope you don’t mean you’re injecting yourself with the grocery store rubbing alcohol. That is NOT intended for injection! I hope you are aware of the different standards for chemical production. The grocery store isopropanol has tons of contaminants that, when used superficially on skin, don’t cause any issues. However, once ingested or injected, these contaminants can bioaccumulate in your tissues. Not good stuff.
Please attempt to source pharmaceutical ethanol. Your other ingredients are fine provided that they are sterilized and are of pharmaceutical/USP grade, but isopropanol is just horrible to use as an injection. For one, it’s toxic; this is not going to be great for your health even at low doses.
I can think of exactly zero pharmaceutical companies that make anything injectable for humans that contains isopropanol.
You’re flying completely blind. There have been absolutely no studies in humans of the pharmacokinetics of injectable rapamycin. Furthermore, your excipients can drastically alter the pharmacokinetics in ways you cannot possibly predict without a laboratory environment.
Furthermore, as RapAdmin says, most of the mice studies are not injected - they are fed it in chow. Even among mice, injections are sparse since it is quite labor intensive to inject hundreds of mice each and every day of the study.
It is by no means a “no-brainer,” because you have completely nil data on how it will work in your body.
Furthermore, how are you ensuring your injections are sterile? I see no mention of your procedures at all. I hope you aren’t doing it in a non-sterile manner, as that risks horrific infections. Given that you state you get your advice from the “internet,” I have a bad feeling about your answer…
I seriously doubt the credibility of both your vendor and your supposed test results.
Side effects and blood test results can only go so far in determining your overall health. The question is what blood tests, and what side effects. Most people, for instance, feel perfectly fine inhaling carbon monoxide, until they pass out immediately after. How you “feel” and what you “believe” are never good measures of how you actually are.
Oral routes are not inferior. They are simply different routes of administration. Injections simply increase bioavailability and/or release profiles. In my opinion, there really isn’t a reason to opt for injections when you can achieve a therapeutic dose via the oral route just as effectively. This, of course, depends on what your end goal is, but I suspect your goal isn’t based on any scientific rationale, but rather dollars per dose. That is not a healthy nor safe way to look at this.
Never briefly read. Thoroughly read. Skimming details leads to disastrous consequences, especially for homebrewed medicine.
Dear Lord! You’re taking 20 to 30 milligrams!? And not only that, but injecting it? No wonder you have mouth sores so severe you cannot eat! That is a serious side effect, not a minor one!
The reason mouth sores appear is partly due to immune suppression, where viruses in your mouth become opportunistic. It’s an indicator that your immune system may be severely compromised. This is not ideal at all.
Furthermore, your dose is many times higher than even the most dire cases of organ transplant patients! How did you arrive at a 20-30 mg dose? What kind of papers are you reading!?
Repeat that last part, but slowly.
The fact that you did not take the time to even Google the definition of gavage before posting concerns me, as that says to me you aren’t really reading or understanding these scientific papers well.
That is not how it works at all. You don’t choose what to read. You. Just. Read.
You can’t cherry pick articles that support what you want to believe. That’s not science, that’s confirmation bias.
I don’t even know how to respond to this.
I’m not even sure you fully understand how ridiculous “relative probabilities” sounds.
Don’t trust, verify. Self-medication is not a “just trust me bro” thing. Not at all.
Not just some people. A damn lot of people.
You’re forgetting that different countries have different laws. And Chinese laws are certainly not up to the standards of pharmaceutical standards elsewhere in the world.
US vendors must pass through far more strict and controlled regulations and quality standards than that of other countries. Even with India, the products that are exported to Europe or the US have to be held to a much higher standard than what is sold within India or other non-western markets. It just isn’t comparable.
How the F did you come up with that math? Sensible probabilities? Brother, you don’t even know what you’re doing to your own body.
That doesn’t even make any damn sense! Knowing basic calculus doesn’t mean you automatically know how to prepare sterile pharmaceutical preparations, let alone know how such an experimental regimen will affect your body.
In addition, nearly every pharmaceutical expert knows how to do that basic derivation. That’s high school calculus, I mean come on! Knowing it off the bat is not impressive.
What is impressive is whether or not you can do this on the fly:
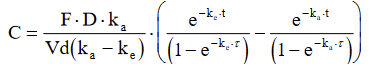
Now you don’t need to solve this. None of us do this by hand, we use calculators. However, do you recognize this formula? I’ll give you some credit if you at least know what it is.
In any case, I think you should look up a guy named David D. and his friend Justin K. But I doubt you can figure out what I mean by that.