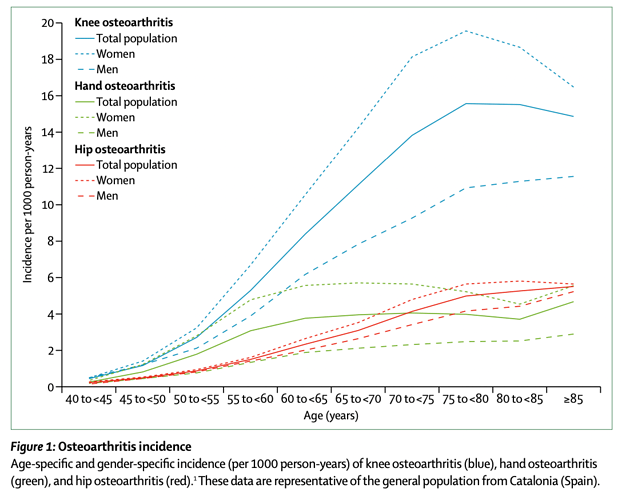
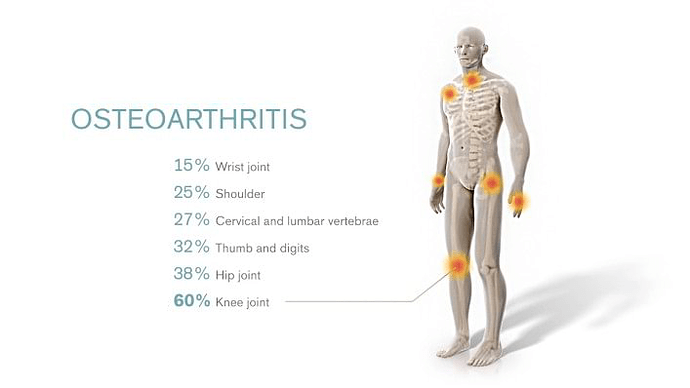
Osteoarthritis is a leading cause of disability and source of societal cost in older adults. Osteoarthritis is a condition that arises increasingly commonly after people age past 50 years, especially in women.
At the American Aging Conference, May 17 to 20, 2022 Dennis Minton is presenting on new research that suggests that rapamycin can delay onset of osteoarthritis.
These preliminary data demonstrate that common marmosets develop bone and cartilage-related hallmarks of OA in an age-related fashion and suggest that treatment with Rapamycin may compress severe OA pathology to late life.
Rapamycin delays age-related osteoarthritis in the common marmoset.
Dennis M Minton, Angela J Marolf, Kelly S Santangelo, Adam B Salmon, and Adam R Konopka,University of Wisconsin-Madison William S. Middleton Memorial Veterans Hospital Colorado State University UT Health San Antonio.
Mechanistic target of rapamycin (mTOR) activity is increased in osteoarthritis (OA), and the mTOR-inhibitor rapamycin (Rap) can attenuate experimental OA in young mice. However, it remains unknown if Rapamycin can protect in a model which better recapitulates the age-related OA most commonly seen in humans.
We evaluated if common marmosets, a translational non-human primate model of aging, can serve as a novel model of age-related OA, and if chronic Rapamycin can decrease OA severity.
Common marmosets (2.6-16.5 years) were orally administered Rapamycin (n=22; 13M/9F; 1mg/kg) or a yogurt vehicle (n=34; 18M/16F) daily from mid-life until natural death. Following necropsy, micro-computed tomography (µCT) and histopathology were performed and graded in a blinded fashion to assign a bone-related OA score and articular cartilage structural damage (ACS) score, respectively. Marmosets were stratified as adult (<8 years), aged (8-12 years), and geriatric (>12 years) for grouped analysis.
In both control (R2=0.18, P=0.01) and Rapamycin-treated (R2=0.54, P=0.0001) marmosets, OA score increased significantly with age. Differences between trendline slopes approached significance between groups (P=0.06), suggesting different OA progression rates between groups, and a longer period unburdened by OA early in life with Rapamycin.
When stratified into age groups, adult Rapamycin-treated marmosets displayed lower OA scores than control (P=0.03), while there was no treatment effect in aged or geriatric marmosets. In the subset of available marmosets (n=36), ACS score correlates with µCT OA score (R2=0.4; P<0.0001). Whole-joint ACS correlated with age in Rapamycin-treated marmosets (R2=0.38, P=0.02) but not in control marmosets (R2=0.12, P=0.12). When stratified by age, there were no significant differences in ACS score in any age bracket, despite adult Rapamycin-treated marmosets displaying ACS scores 50% lower than control (3.10.4 vs 6.02.5; P=0.49).
These preliminary data demonstrate that common marmosets develop bone and cartilage-related hallmarks of OA in an age-related fashion and suggest that treatment with Rapamycin may compress severe OA pathology to late life.
Speaker at American Aging Conference, May, 2022
- Dennis Minton(Speaker)University of Wisconsin-Madison
Related Reading
Rapamycin (RAPA, an mTORC1 pathway blocker) upregulation of Parkin-mediated mitophagy tends to attenuate mitochondrial impairment caused by TNF-α in preosteoblasts. The experiment in vivo demonstrated that the combination therapy with TNF-α neutralizing antibody and RAPA significantly reduced osteoporosis in AIA mice. Drug inhibition of this pathway can be a potential treatment for osteoporosis in patients with RA
.