You just refuse to recognize the preponderance of the evidence that lower LDL is beneficial.
Statins lower LDL and reduce all-cause mortality. Lower ApoB is better.
I’m sorry, I will just take the opinion of the vast majority of doctors that endorse lower LDL as being better and prescribe statins to keep it at a healthy level.
I don’t think he is refuting “lower” LDL with favorable phenotype in general - it’s refuting “lower is always better” with statins. It’s more of a question what exactly “optimal” is in what situation and what intervention. It’s a complex question with no proven answers. It’s especially problematic when people aren’t fully informed.
The most simplest question is we know HMGCoA inhibition via statin in isolation (even with avoiding crossing the BBB) increases the risk of diabetes, Lp(a), and PCSK9 at the very least (not exhaustive list), how is that benign? These are all potential independent risk factors any way you slice it. The most likely net beneficial tradeoff for one who is fully informed is key in the selection of intervention.
My recommendation is at the very least reading the entire copy of the newest edition of Therapeutic Lipidology to start an informed discussion with your doc, preferably while picking apart the references to avoid textbook errata, errors in line of clinical reasoning, and such. Unfortunately, most people do not like to read and start jumping to unsupported conclusions about a complex topic that has a lot of caveats. It’s not much different than accepting the terms and conditions without reading - even then it’s not a perfect solution - but it’s a good start if you want to increase your odds drastically to avoid making the wrong decision based on faulty conclusions.
I just posted an article from a cardiologist, with which I’m in complete agreement, that statins are totally appropriate in the right patients and under the right circumstances.
I’ve been primarily concerned with the low risk patient who gets a jump in LDL from rapamycin.
You clearly don’t read my posts and merely cherry pick your comments.
BTW, I think it’s worth noting - as much as this sounds like an extraordinary claim - I suspect the vast majority of doctors and even cardiologists in general actually aren’t reading a standard lipidology text or equivalent due to a priority of reading issue when it comes to preventative medicine. Gotten the usual demonstrable misinformation or illusory knowledge many times. This isn’t as common for many other parts of medicine but perhaps the more compelling the hypothesis the more likely it happens to some degree.
I’ve surveyed plenty of cardiologists (including my experience with attendings at academic institutions who are “well-decorated” and go to extraordinary length to be intellectually honest about their limitations, private practice, and just “preventative cardiology” docs etc) and lipidologists personally. That’s why I specifically mention a lipidologist consult as an ideal line of a decision tree for most people, particularly when it is borderline with multiple risk enhancing factors.
With additional resources and interest - I’d recommend participating in conferences with folks who could or are already involved in decision-tree style guideline committees to really debate the finer points down. I’ve done that once and the experience is much more eye opening.
I am not convinced that lower is not better. All of the most recent studies that I have found still say this. I am completely unconvinced that the U-shaped curve which has recently become popular is true. The evidence, IMO, still indicates that lower is better.
The U-shaped evidence ignores many of the confounding factors of their results.
In this case, I use confounding to mean: “Confounding is a distortion (inaccuracy) in the estimated measure of association that occurs when the primary exposure of interest is mixed up with some other factor that is associated with the outcome”.
If you have muscle cramps that is a genuine negative side effect you could do without.
Maybe you should therefore see if your insurance will cover a PCSK9 inhibitor.
We know zero LDL is essentially “deadly” or “failure to thrive” if you prefer more technical speak. That’s far more than enough to say that it’s not a straight line down through extrapolation as is claimed.
Let’s start with this - if more information comes out for safety - I’d change my mind on determining how low the LDL range is for “optimal” and I’d consider an additional intervention with known side effects.
In the meantime - why do you worry about a tiny potential absolute risk reduction when we compare LDL 75 with favorable phenotype vs LDL 40? One can always change their strategy as new information comes out. I’m not inherently anti-statin either - I recommend statins all the time to those who are indicated for it but there are plenty of people who should be on it where no amount of reasoning will help them help themselves. The key is recognizing clear limitations and real known risks, while being open-minded and flexible. Even those with a high risk tolerance should at least calculate the theoretical absolute risk reduction. Yet very few people want to do their homework.
A natural human tendency towards interventionism should be recognized, particularly without full information and “knowing” where to draw the line of what one “knows”, which can lead to net harm. If there were more compelling risks of not acting - which I also recognize as a risk - I’d be more willing to intervene personally.
As an example, we know from fairly well-done longitudinal studies in vegans without statins who tend to be very low cholesterol (can be below 70 over a lifetime) and those with too low cholesterol from high dose statins (these are people indicated for one) get more brain bleeds and slightly increased risk of osteoporosis. There is enough suggestive evidence for me to be wary.
Maybe, but the muscle cramps are very infrequent and only occur in my feet or hands. I maybe get them once every couple months. Ill try it though.
Please, that ignores the confounding factors related to the vegan diet.
I am not advocating LDL levels to be outside of the generally accepted “normal” limits.
What I am advocating is that LDL levels are probably better at the lower normal ranges than the higher normal ranges. Certainly, I would not advocate trying to get an LDL level below 40ml/dL is helpful.
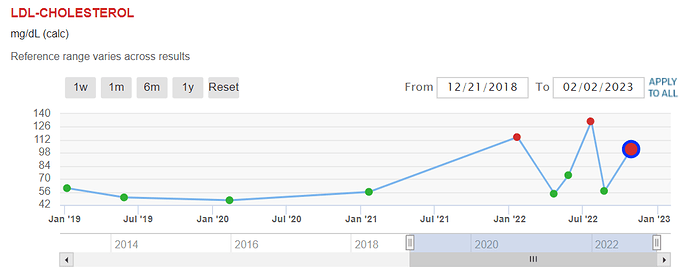
What brings me to this discussion is the general acceptance that rapamycin raising lipid levels is of no concern. Rapamycin has caused my lipid levels to vary widely and generally trend upward. This is of concern to me. Generally speaking, most of my blood markers with regard to epigenetic aging tests have worsened since I started taking rapamycin.
When those side effects happen to those on high dose statins who are not vegans and non-statin-taking vegans (note high dose phytosterols from diet and lack of certain types of saturated fat intake, in general, can cut down LDL a lot, but there are potential issues with that approach in select individuals because phytosterols that do get absorbed are atherogenic) at the same time - I’m not sure how much certainty you can put to “confounding”.
Because there is very limited evidence linking low LDL levels with an increased risk of osteoporosis.
If you can show me any studies with a substantial cohort, RCT, and substantial time I will change my mind.
The other option is to wait for more information while dynamically hedging your bets carefully. I size my bets accordingly to confidence levels with as much quality information from the strongest arguments of both sides to avoid overconfidence.
I’m also concerned about a whole other myriad of issues such as anxiogenic cholecystokinin tetrapeptide levels on depression and suicide (rarely mentioned) just as another example of how complex downstream cholesterol functions can get - among other issues. Again, the issue is a lot more complex than it may seem. Better to assess and evaluate risk carefully. I can’t say for you - but most people are bad at that - it’s like a vast majority will raise their hand in a room of 100 random people asked whether they are an “above average driver”. Almost half of people are clearly wrong and overconfident. The other half may be to some extent as well.
There is some mendelian randomization results on this, and triglycerides seem to be causally associated, LDL only weak evidence:
There was consistent evidence that triglyceride (TG) is causally associated with DS (MR-IVW β for one-s.d. increase in TG = 0.0346, 95% CI 0.0114–0.0578), supported by MR-IVW and GSMR and multiple r2 clumping thresholds. We also observed relatively consistent associations of TG with DSH/suicide (MR-Egger OR = 2.514, CI 1.579–4.003). There was moderate evidence for positive associations of TG with MD and the number of episodes of low mood. For HDL-c, we observed moderate evidence for causal associations with DS and MD. LDL-c and TC did not show robust causal relationships with depression phenotypes, except for weak evidence that LDL-c is inversely related to DSH/suicide. We did not detect significant associations when depression phenotypes were treated as exposures.
Statins tend to lower triglycerides too. And apoB can measure it all.
Just to keep it short - it’s not clear whether it is the statin or LDL lowering that is the cause as you may already know. Again, there are a lot of dimensions involved. Lipids aren’t in isolation - TG vs HDL vs LDL are dynamic to an extent. Not going to get into subfractions. Ultimately, the paper you put forth does not analyze nonlinear relationships.
To be clear, I realize the potential causative and potential confounders involved are complex, hence I adjusted mortality curves for all the potential known acquired low LDL reasons that confound mortality, treatments vs treatment naive, and compared it to known genetic factors to avoid biasing towards higher LDL targets for “healthy” with the assumption of the LDL hypothesis being true where apoB and LDL are a true causative independent factor.
I’m not going to go super in-depth here on the finer points, as this discussion can go on for a very long time and from previous experiences, it’s probably not particularly fruitful for everyone here (not just us) while the benefit from ARR theoretically is marginal assuming the average “healthy” individual and “perfect” lifestyle factors with say LDL 75 and favorable phenotype/no discordance. We’ll agree to disagree if you wish but I suggest one at least compare the theoretical ARR using the sort of validated 30 year Framingham data if one hasn’t yet. It’s a very simple exercise.
It’s your body and your choice. I’m merely describing what I do personally and how I got to it very generally speaking - I have a low risk tolerance. How one decides what to take or not take with their lipidologist is something they will have to decide on their own with their own risk tolerance levels.
I’ll just finally say the common theme I see with lipidologists is the more one reads, the less one thinks one knows. Maybe about half of what one reads ends up being meaningless, but we don’t know which half is the issue so to speak. One of my dad’s best pieces of advice to me before I started med school that keeps ringing true the deeper I get - and he has decades of experience managing clinical trials.
To reduce the risk of being dead wrong, I encourage one to read the newest edition of Therapeutic Lipidology or at least some other up to date text that is essentially equivalent and pick apart the potential errata or flaws in the text, if they haven’t already. Make sure to do one’s homework if one doesn’t. Most people don’t even want to do basic homework so take that into account.
Thank you for the schooling.
But, I think we have lost the thread of the conversation.
Are you saying that low LDL if it is in the recognized normal range by labs such as LabCorp and Quest Diagnostics is worse than higher LDL? And, should we ignore the fact that rapamycin raises LDL in many people?
If you want to prevent aging-related vascular diseases one of the first things to do is keep your lipids in the normal range. Most people with a good lipid profile will not be obese and are probably moderately active or exercise.
BTW, I did take probability and statistics in school. And, it is obvious to me many people do not understand the difference between comparative, relative, and absolute risk.
I am currently taking rapamycin, but the long-term risk factors have not been determined in humans. The long-term risk is not a major factor to me at 82, but, if I was younger I certainly would be keeping an eye on my cholesterol levels regardless of the fact that rapamycin proponents choose to ignore this. In another thread, we have been discussing the long-term negative effects of sleep supplements. The dementia problems don’t show up for decades unless you already have dementia.
Maybe this is the first warning:
For people really into this topic, there “might” be a free download of this textbook at this location: Libgen.rs sourced Textbook: Therapeutic Lipidology, Series: Contemporary Cardiology, Publisher: Humana, Year: 2020
I believe that Rapamycin produces some great benefits, but also has side-effects. Therefore additional treatments need to be added to reduce those side-effects in order to make Rapamycin more effective. This can be seen when Rapamycin is paired with either acarbose or metformin. Maybe a Rapamycin and statin pairing would also be of benefit.
Someone should mention this to Dr. Miller for a trial?
To be clear, I understand people have taken stats in school and I’m not trying to “school” anyone here - it’s rather to help folks understand how they can get involved in learning if they wish to and recognize a knowledge gap, if any. I suspect pretty much everyone here probably has a college education at least if not further - although one doesn’t have to go to college to learn this.
There’s also a difference between advanced stats where someone at a PhD level can easily pick apart incorrectly applied methodology (as well as most masters level of knowledge can probably do it with enough practice - again, one doesn’t have to go to college to learn this and I’m not intending to be exclusionary here) which happens all the time in medical research papers vs undergraduate stats & probability who probably won’t realize it most of the time, especially when applied to medical papers in certain labs without relevant context, assuming they aren’t reading just the title and abstract which seems to happen pretty often.
LCME for docs actually didn’t require stats/biostats back then for the curriculum - so it’s up to old docs who didn’t learn to keep up with CME. Same with docs with just regular biostats knowledge that did not go to a more advanced level. So this is not a doc vs not doc deal. It’s whether someone actually took the time to read through knowledge from textbook/papers with relevant knowledge/etc with understanding of relevant skills, regardless of whether they are a doc or not, and I suspect >9/10 it’s usually someone who does not have those relevant skills and background, even though I try not to assume too much to avoid underestimation, and I’m trying to be as inclusive as possible regarding any mutually interesting discussions because I enjoy the approach to crowdsourcing information and talking to folks on rapa.
I’m not saying low LDL is necessarily better or worse than higher LDL in isolation. It’s a complex situation, hence I mentioned “and favorable phenotype”. We should be concerned about the potential implications of increased LDL from rapa, but we don’t know for sure whether it is “bad” especially with the seemingly transient nature that varies by individual, as well as the apparent general phenotype.
This is the takehome point for me. Thank you everyone who has been participating in this thread. I feel like its a masterclass in heart disease and possible strategies at risk minimization.
I assume Rapa’s mechanism to be an increase in mitochondrial efficiency which increases the Acetyl-CoA level in the cytosol (and as an effect of this the nucleus). That creates more substrate for the creation of cholesterol.
Hence one could expect more cholesterol of various forms.