I suggest you do more digging with PCSK9. It’s not just some isolated protein that affects LDL.
Yes, that was HMCGR inhibition in the brain and the effect was miniscule, just like every other gene on cognition (about 10 000 genes determine variation in cognition):
The effect in context:
In the general population (18-65) reaction time increases by 2.8 ms a year.
And the study found an increase of 0.067 milliseconds per 1 SD decrease (38.7 mg/dL) in LDL-C in total. So if you have 2 SD lower LDL-c you have 0.14 ms increase in reaction time. And HMCGR inhibition showed improved memory performance:
0.14 ms slower reaction time from two standard deviations lower LDL. But improved memory performance.
Just use rosuvastatin and it will be ok.
It’s not miniscule. It’s small but it’s moderate negative effects when you account for positive cerebrovascular effects masking the total net effects. That’s only one issue.
As an example of many, new onset diabetes is a risk factor for statins that only have known HMGCoA as a specific target.
You’re looking at things in a very isolated manner.
0.14 ms slower reaction time in total, when reaction time increases by 2.8 ms a year is a miniscule effect. And you already know you can mitigate some of the risk from using statins that have a harder time crossing the BBB.
Statins aren’t risk free. There are trade offs with everything. The risk is low though and most do not get side effects.
Diabetes risk can be mitigated by using a CGM every now and then.
The risk is low in what time frame?
What is the proposed benefit in absolute risk reduction as opposed to LDL 75 and pattern A?
The reaction time increase is a lifetime total increase of 0.14 ms. That is very low.
By low risk I mean 90% do not get side effects.
Not just reaction time. Look at the other potential cognitive factors and dementia in those “lifetime” risks.
Then look at net cognitive effects in statins. Still real. Note that using statins are not equivalent to Mendelian randomization.
I know that’s why it’s better to use a statin that does not as easily cross the BBB. I have an APOE ε4 allele, so I care about cognition risk. If I could do a Desmosterol test I would do that.
Ultimately, my main point is the theoretical absolute risk reduction is minuscule, when compared to already low LDL and favorable phenotype. You haven’t mentioned exactly what that ARR is.
At some point, additional potential risks that are well known vs additional potential marginal benefit must be factored in. Why trade potential for one small benefit for multiple potential risks?
Diabetes accelerates cognitive decline particularly in Apoe4 but pretty much all folks.
Sure, I might think differently if I can’t measure desmosterol levels. I kind of believe in the lipid increasing risk of dementia hypothesis though.
We don’t like to see absolute concentrations of desmosterol below 0.8 mg/L in our patients. We also treat patients with one or two copies of the APOE e4 alleles or a family history of dementia with kid gloves and make sure they have a desmosterol level greater than 1.0 mg/L.
You could measure diabetes risk with a CGM though? If you saw glucose increasing or A1C from statin use?
I’ve been through why Attia is biased and miscites several papers with verifiably factually incorrect statements in the opposite direction when it comes to CGM use in nondiabetics.
You’re again looking at diabetes in isolation. It’s a very complex disease.
Yes, but couldn’t you use a CGM or measure A1C to see if you have a side effect from statins relating to diabetes?
A1c isn’t as accurate as you think. I suggest you really dig into all these tests you propose based on “influencer” opinion that isn’t necessarily even applicable to your situation.
As for AD, brain insulin resistance is much more complex than I’d like to explain in depth, you cannot necessarily assume the lack of peripheral insulin resistance to non existent brain insulin resistance.
The mistake we make with statins is in just looking at goal numbers instead of risk factors. Stop looking just at numbers and consider whether people have other risks such as high blood pressure, smoking, FH, etc. For those at high risk, statins are appropriate and the benefit/ risk works. For those at low risk, statins aren’t worth the side effect risks and shouldn’t be prescribed. The exception would be Very high LDL levels which are certainly not attributable to rapamycin alone.
The focus on numbers only is inappropriate and has no justification without considering the patient as a whole. Statins can be life saving, but only when used in appropriate situations, which does not include trying to get a low risk patient down to some absurdly low number requiring high drug doses leading to side effects.
How are we measuring LDL here? I am only wanting to enter the conversation because I have been on 10mg rosuvastatin for the past year now. I am 25, exercise regularly, eat healthy and have no family history of CVD or HF.
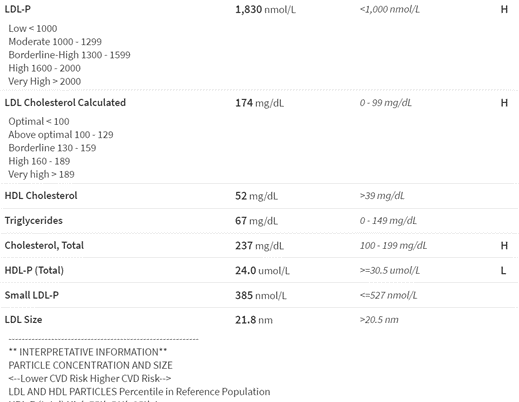
But when I did my blood work last year (pre statin), my NMR lipoprofile was the following:
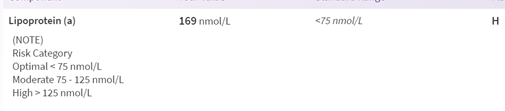
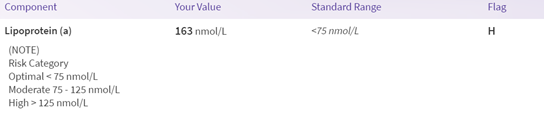
and my Lp(a) was :
Now after being concerned about the Lp(a) being high and my LDL-P and size, I asked what I could do. The doctor put me on 10mg Rosuvastatin(before this, I tried changes in diet and exercise and saw no difference).
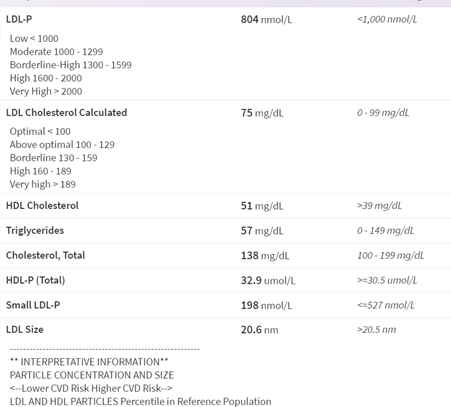
My bloodwork at 2 months on 10mg rosuvastatin:
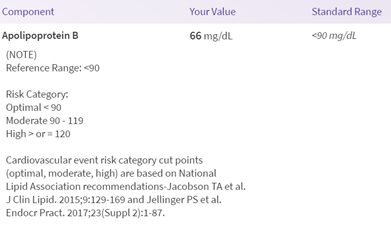
My ApoB( now I only asked for this as they didn’t do it pre statin and didnt realize the importance of knowing my ApoB) :
My Lp(a):
The only side effects I have noticed was just cramps occasionally. I have no other noticeable effects on anything else. I go for my yearly physical and will redo blood work, but for me I thought the benefit was worth the perceived “risk”. Now, I am on a low dose so the “risks” are not as high, compared to people doing higher doses.
Also: I am just showing my values for people to see how statin’s have effected me, not looking for medical advice
I can’t dispense medical advice over the internet and almost certainly people will start showing me their lipid labs if I start doing so. All I can say is if one has multiple risk-enhancing factors, one of which is high Lp(a), then it is worth a discussion with your doc and preferably with a lipidologist.
I’d also mention statins increase Lp(a) somewhat - an independent risk factor. If one can afford it, PCSK9 inhibitors may be an option for those with high cholesterol (pre-statin) and high Lp(a). That’s a general statement.
Right, unfortunately though PCSK9 are expensive and insurance will only cover it if you are deemed stain intolerable by still having high LDL levels and are on highest dose of statin.(part of me thought of just saying I was taking my statin but not, and have my LDL levels high so I could try to get a PCSK9 inhibitor)
To me, I think the only thing I am worried about is the long term use of statin, or if it is worth trying to be intermittent on it over the years. But with my high Lp(A) and no treatments for that, I think I will just be on my statin until we get a better therapy.
I’ll mention this - some cardiologists have sample PCSK9i for patients who may legitimately need them to try and see if it’s worth it and “statin intolerance” is relatively fuzzy in terms of documentation. Just don’t make a false statement.
They can audit it and I don’t suddenly need people claiming I am helping folks in any capacity to commit insurance fraud when I clearly am not implying that at all.