I took a look at this study from ITP lab.
Canagliflozin extends life span in genetically heterogeneous male but not female mice
“Cana at 180 ppm (equivalent to 100-300mg/day humans) at 7 months of age until their death. Cana extended median survival of male mice by 14%” (This sexual dimorphism is very strange causing me to question their postulated theories on mortality reduction. Rapamycin is superior in that it delivers enhanced longevity in female mice too)
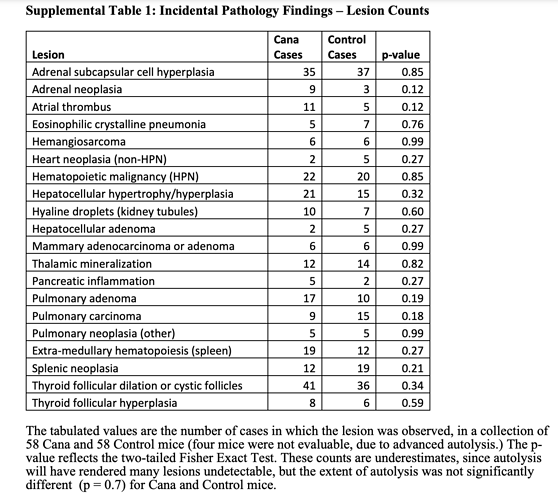
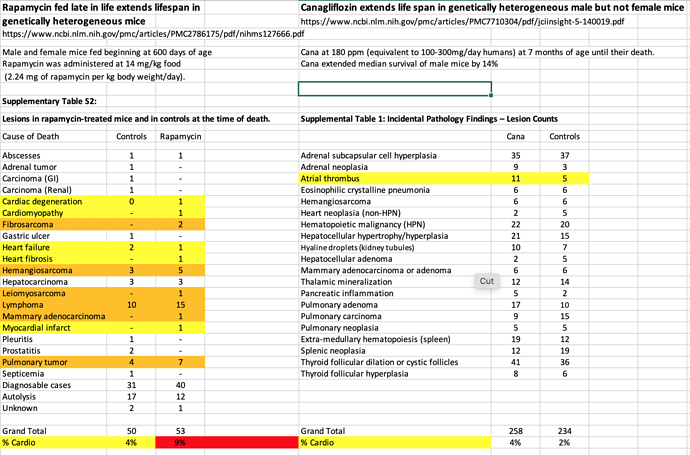
Taking a look at pathology, 90%+ cancer neoplasms.
And compared to Rapamycin study, looking to see if any different signal re cardio deaths. Seems like perhaps less cardio mediated deaths, but likely dosen’t reach significance.
Although the study authors state CANA and Rapamycin pathology outcomes similar.
“Terminal (end-of-life) necropsies for each of these 4 drugs (including Rapamycin) including the data on Cana shown here, lead to the same conclusion: the spectrum of lethal and nonlethal
late-life illnesses is not changed in quality or severity, even though the treated mice are older at time of death. Although this conclusion is limited by the low statistical power of small case series, the implication is that the drugs extend healthy life span, i.e., produce longer life span by delaying the onset or progression of the diseases most likely to lead to death or terminal morbidity, most of which are neoplastic disease in UM-HET3 and most other mouse stocks”
mTOR is not measured for this study re explaining life extension.
“These observations thus suggest strongly that the life span benefits of each drug, and presumably the other benefits already shown in acarbose-treated mice, are a consequence of lower maximal postprandial glucose levels. The basis for these protective effects is not completely understood, and may not directly reflect the effects of Cana on glucose homeostasis. Hypothetically, Cana might reduce mortality associated with neoplasia in mice by modulating glucose metabolism in tumor cells. The metabolic requirements of rapidly dividing cancer cells are quite distinct from those of normal cells, most of which are ordinarily nonmitotic”
Although they did mention mTOR1 referencing another study.
“Cana suppressed hepatic TORC1 signaling, while increasing AMPK activity in this
tissue; both effects are associated with life span extension in mice and other organisms (47)”