In the overall scheme of things, we know very little, and the little that we think we know is usually overturned by ongoing studies and evidence. So there’s that and the best doctors deal with it.
Without creating another debate, I too believe inflammatory markers are more important than lipid levels. There is a group of doctors from Australia that are fans of the Keto Diet, that think lipid levels are misunderstood.
For some interesting viewing check “Low Carb Down Under” on Youtube.
https://www.youtube.com/results?search_query=low+carb+down+under
And, in particular as to cholesterol:
Dr. Paul Mason - “Why your doctor thinks cholesterol is bad - Big Pharma deception”
Who knew? There are 2 types of saturated fats, an odd and an even. Apparently, according to this study in Nature, the odd guys found in beef and butter have all kinds of benefits, but the evens, not so much. They claim that due to warnings over saturated fats that the levels of these good C15’s are dropping. Maybe too much .
Similar paper here, and would explain why rapamycin might help:
Diet, and how it relates to CVD, is an unresolved topic.
Here’s a look at how high carb/ high fiber directly impacts brachial artery flow. Pretty impressive.
Almost certainly due to Covid so don’t get discouraged.
Eyes closed must be much harder without the visual cues to assist.
Back to lipids/CVD/rapamycin:
This MD/Phd physician/researcher explains the cholesterol U-curve extremely well in very practical terms.
This “controversy” was all the rage on the internet about a year ago because of people misinterpreting the studies and concluding that mid-range cholesterol is “optimal” and that we shouldn’t lower it past a certain point. The apparent controversy was put to rest. I recommend watching all the way to the end because he continues to make excellent points (i.e. weight-mortality curve is also U-shaped, etc).
Bottom line – LOWERING CHOLESTEROL/ApoB DOES NOT INCREASE MORTALITY. If you watch the video, he goes through the observational studies in a very practical, understandable way:
Thanks. Will watch it for sure.
Very good analysis, this guy is an AMAZING presenter. I always suspected the low end of some of these observational U curves was confounded.
I just discovered his channel recently, but he has a treasure trove of excellent analyses on all kinds of nutrition-related topics.
ok, not rapamycin specific, but more on CAC as CVD tracking biomarker. And it’s not all lipids…you have to look at your CAC score to get a better understanding of risk, but NODODY does them.
Progression of Coronary Artery Calcium and Risk of FirstMyocardial Infarction in Patients ReceivingCholesterol-Lowering Therapy
https://www.ahajournals.org/doi/epdf/10.1161/01.ATV.0000127024.40516.ef
Objective—Statins reduce cardiovascular risk and slow progression of coronary artery calcium (CAC). We investigated whether CAC progression and low-density lipoprotein (LDL) reduction have a complementary prognostic impact.
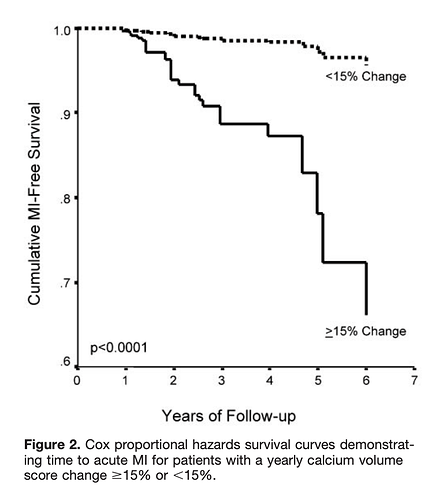
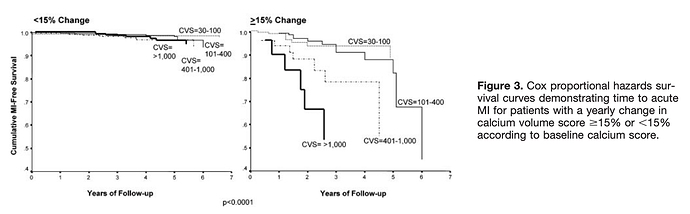
Methods and Results—We measured the change in CAC in 495 asymptomatic subjects submitted to sequential electron-beam tomography (EBT) scanning. Statins were started after the initial EBT scan. Myocardial infarction (MI)was recorded in 41 subjects during a follow-up of 3.2 years. Mean LDL level did not differ between groups (118+/-25 mg/dL versus 122+/-30 mg/dL, MI versus no MI). On average, MI subjects demonstrated a CAC change of 42%+/- 23% yearly; event-free subjects showed a 17%+/- 25% yearly change (P0.0001). Relative risk of having an MI in the presence of CAC progression was 17.2-fold (95% CI: 4.1 to 71.2) higher than without CAC progression(P0.0001). In a Cox proportional hazard model, the follow-up score (P0.034) as well as a score change> 15% per year (P0.001) were independent predictors of time to MI.
Conclusions—Progression of CAC was significantly greater in patients receiving statins who had an MI compared with event-free subjects despite similar LDL control. Continued expansion of CAC may indicate failure of some patients to benefit from statin therapy and an increased risk of having cardiovascular events
The relative risk of suffering a MI in the presence of CVS progression was 17.2-fold higher than that of subjects without progression.
For patients with intercurrent CVS progression > 15% per year, the time to MI and the frequency of MI were greatest for patients with baseline CVS 400. In the patients with CVS change > 15%, the relative risk of first MI was 3.8-fold, 6.4-fold, and 12.0-fold higher when the baseline CVS was 101 to 400, 401 to 1000, and 1,000, respectively.
The risk of hard events was significantly higher in the presence of CVS progression despite low LDL serum levels, although the interaction of CVS change and LDL level on treatment was highly significant. The latter observation strongly suggests that a combination of serum markers and vascular markers may constitute a better way to gauge therapeutic effectiveness than ISOLATED measurement of lipid levels
Thanks for the tip, will have a look.
One additional comment…fast forward, and paradoxically, treatment with statins will INCREASE your CAC score. And so will elevated endurance exercise…it’s a plaque stabilization mechanism. It is well documented in the literature re endurance exercise and CAC score, and does not correlate with longevity in those with high VO2max capabilities throughout life. Another paradox.
Very new paper.
Physical activity and the progression of coronary artery calcification
Prospective cohort study of men and women free of overt cardiovascular disease who underwent comprehensive health screening examinations between 1 March 2011 and 31 December 2017.
We analyzed 25,485 participants with at least two CAC score measurements. Compared with participants who were inactive, the estimated adjusted 5-year average increases in CAC in moderately active and HEPA participants were 3.20 (0.72, 5.69) and 8.16 (4.80, 11.53). Higher physical activity was association with faster progression of CAC scores both in participants with CAC=0 at baseline and in those with prevalent CAC.
Conclusion: We found a positive, graded association between physical activity and the prevalence and the progression of CAC, regardless of baseline CAC scores.
Very interesting. Great presenter. Will definitely have to check out some of his other things.
This is certainly interesting.
So the baseline CAC score matters and progression > 15% per year matters a great deal. This seems to be the case even in the face of low LDL levels.
Maybe LDL is a poor marker compared to some other measures. Maybe some people are so genetically prone to CVD that nothing much stops the progression.
The score certainly has value and is underutilized.
ABSOLUTELY, something found in repeated future studies (this study was in 2004)
And yes, that’s why a first MI is found in high and low LDL persons.
That’s a more interesting question…but anyone interested in living longer needs to be checking this marker, and intervene with whatever is in the toolbox (lifestyle, meds).
And there must surely be a genetic component, beyond just classic FH or LPA genes.
The long lived, they have some special CVD deferral genes, this is widely shown in GWAS studies.
Yes, the long lived have a deferral mechanism for basically everything. It’s like they’re on an intrinsic mTOR inhibitor.
They’re healthy and avoid major illnesses for most of their life and then suddenly get something and fall off the cliff.
That’s why I don’t separate healthspan and lifespan the way others seem to do. They’re very related.
I was aware of this paradox but not that statins do the same.
Human mole rat equivalents, who age epigenetically but not by classic markers. Then just keel over at end of life. Lost a couple of relatives near 95 yr old. Got sick and quickly passed away.
I totally agree. Longevity, medically extended, with major comorbidities, reduced independent living, partial cognitive, is not a “lifespan” target. Just a longevity statistic.