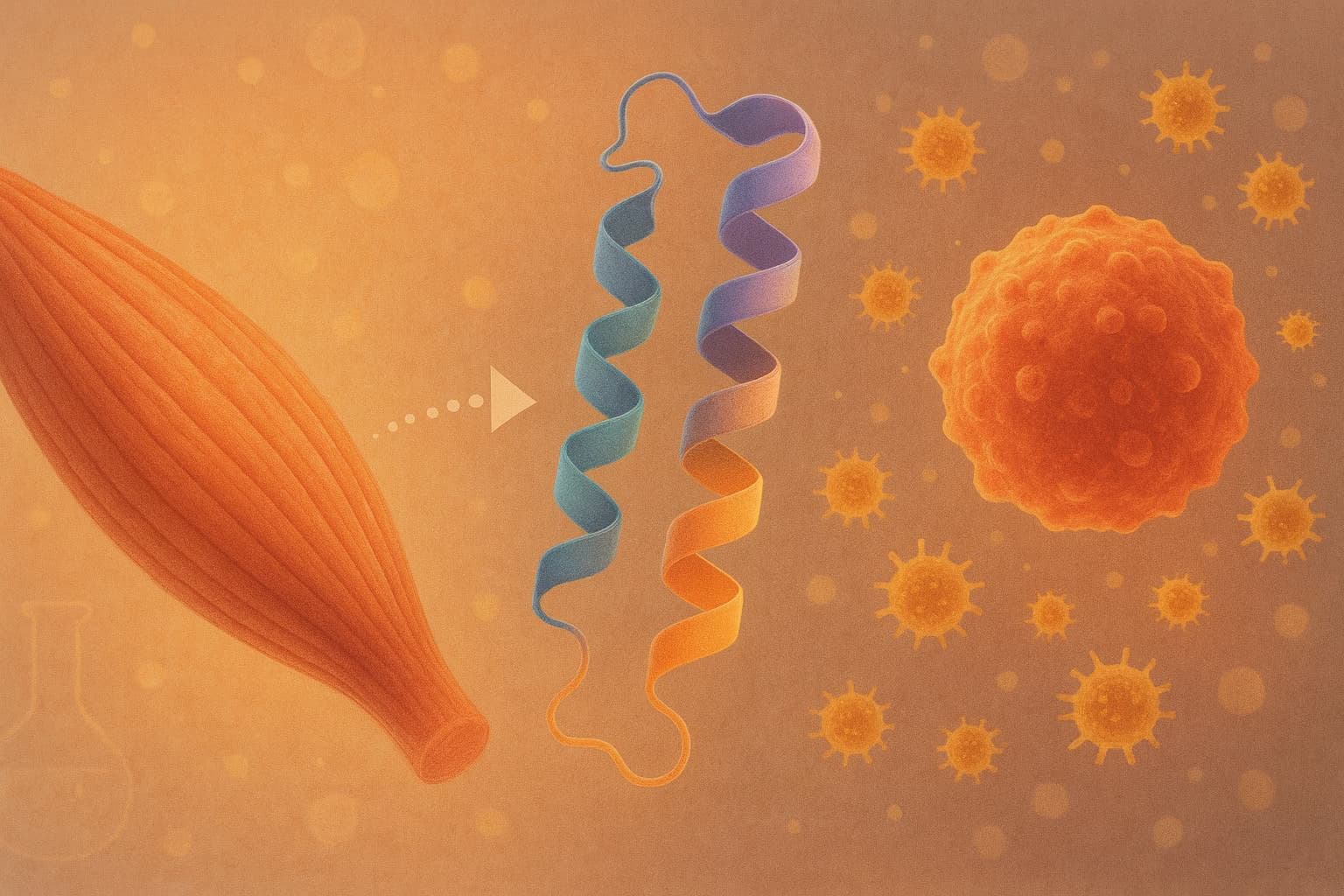
A research team in China has engineered a new long-acting version of Irisin, the exercise-induced myokine long linked to metabolic regulation and anti-inflammatory effects. Native Irisin acts rapidly but disappears from circulation within an hour, severely limiting any clinical use. The new construct—an albumin-binding domain (ABD)–Irisin fusion—extends the hormone’s half-life by roughly 30-fold while preserving biological activity.
The study, published in Nature Communications Biology, begins with the longstanding observation that Irisin positively influences adipose browning, mitochondrial function, and inflammatory signaling. But the peptide’s instability in the bloodstream has prevented translation into therapy. By attaching a small albumin-binding sequence to Irisin, the researchers created a molecule that “hitchhikes” on serum albumin, avoiding rapid renal clearance and enabling durable tissue exposure. A similar approach is already used as a half-life extension strategy for other peptides (GLP-1, IgA, G-CSF, endolysins).
Pharmacokinetic testing in mice showed that while native Irisin cleared within 0.3–0.4 hours, the ABD-Irisin variant circulated for ~10–11.5 hours, a leap similar to what albumin-fusion strategies have achieved for other peptide therapeutics. Tissue-distribution imaging confirmed broader and longer exposure in liver, kidney, and lung.
Functional tests used a lipopolysaccharide (LPS) challenge to trigger whole-body inflammation. Both native Irisin and the new engineered form reduced inflammatory cytokines, but the long-acting variant produced a substantially stronger reduction in IL-6, alongside clearer improvements in spleen morphology and organ histology.
Single-cell RNA sequencing of bone-marrow immune populations revealed the deepest mechanistic insight. LPS exposure triggered a classic inflammatory cascade, including neutrophil activation, JAK-STAT signaling, and TLR4–NF-κB pathway engagement. ABD-Irisin broadly suppressed these signatures, shifting granulocytes and B cells toward a less inflammatory transcriptional state. The authors emphasize that the enhanced effect is driven primarily by extended exposure, not greater per-molecule potency.
Potential Health & Longevity Applications of a Long-Acting Irisin Drug
If the pharmacokinetic gains translate to humans, a long-acting Irisin analog could open a new therapeutic category: exercise-mimetic myokine drugs aimed not at disease treatment but at healthspan extension. For future therapeutic development in the longevity space, this points to a realistic strategy: long-acting myokine analogues (Irisin, IL-6 variants, IL-15, etc.) rather than repeated bolus injections of short-lived peptides.
1. Chronic low-grade inflammation (“inflammaging”)
Irisin’s ability to down-regulate TLR4–NF-κB signaling suggests possible use in reducing the background inflammatory tone that accelerates cardiovascular disease, metabolic deterioration, and immune aging.
2. Muscle-to-metabolism signaling enhancement
A stable Irisin analog could mimic part of exercise’s endocrine signature—supporting mitochondrial function, energy expenditure, and adipose tissue remodeling—especially in individuals unable to maintain high training volumes.
3. Metabolic resilience and body-composition optimization
Comparable to GLP-1 agonists but through a distinct pathway, long-acting Irisin could complement efforts to maintain lower visceral fat, higher metabolic flexibility, and healthier insulin dynamics.
4. Immune balance in aging
The scRNA-seq data hint at a drug that could soften maladaptive myeloid activation and preserve better immune equilibrium over time.
While early and preclinical, this work positions Irisin as a credible candidate in the emerging class of longevity-oriented biologics designed to reproduce key molecular benefits of exercise in a pharmacologically durable form.
Source Research Paper (open access):
ChatGPT5.1 Analysis of paper:
Related Reading: