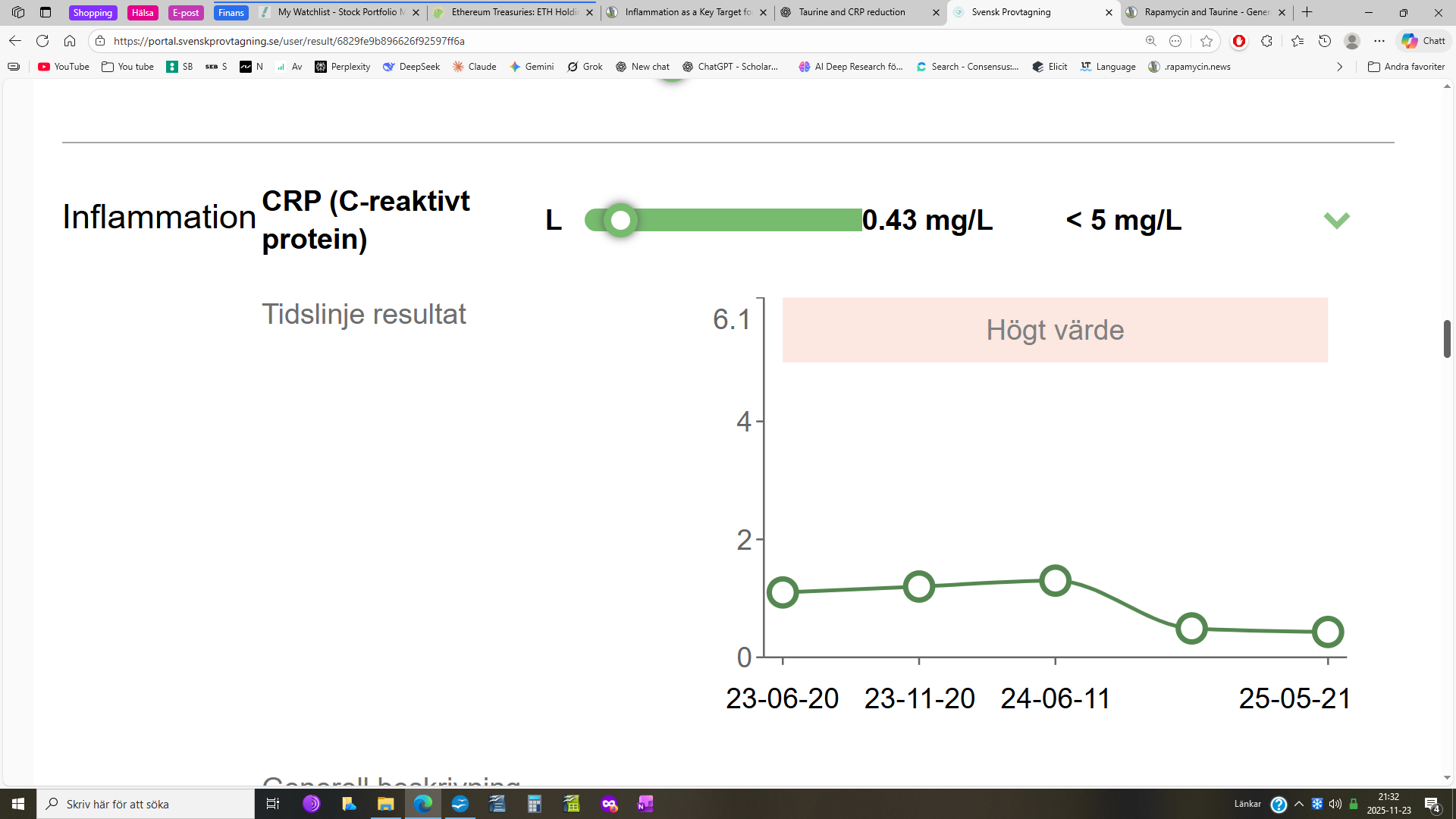
IMO: In this forum, we seem to be more obsessed with lowering cholesterol than lowering CRP.
This, I think, is a mistake. Also note that CRP is included in the Morgan Levine chronological age clock; cholesterol is not.
Below are the edited responses from ChatGPT 5 (paid).
If anyone wants to see the complete, more nuanced response, plug the queries into your favorite AI program.
Query: 'Which do you think is more damaging to healthspan and lifespan, high cholesterol levels or chronic inflammation?"
Answer: “Short answer: chronic inflammation is probably more fundamentally damaging, but in real life, it’s usually the combination of high cholesterol (especially apoB/LDL) plus chronic inflammation that does the most harm to healthspan and lifespan. If I had to choose one axis to obsess over for someone with heart disease, I’d actually say, “High apoB/LDL in an inflamed environment is the real killer.”
So: treat both; don’t pick a favorite.”
Chronic inflammation – why many people now see it as “more fundamental”
Chronic, low-grade inflammation (often measured by hs-CRP, IL-6, TNF-α, etc.):
Is associated with:
CVD events independent of LDL.
Frailty, sarcopenia, cognitive decline, diabetes, and overall mortality in older adults.
Trials like CANTOS (canakinumab) and COLCOT/LoDoCo2 (low-dose colchicine) showed that targeting inflammation in people with already low LDL still reduces heart attacks and strokes.
That tells us inflammation is not just a bystander.
In aging medicine, we sometimes talk about “inflammaging”:
Chronic inflammatory tone gradually:
Damages vessels.
Impairs immune function.
Interferes with repair processes.
Promotes insulin resistance.
It’s plausibly involved in neurodegeneration, cancer promotion, osteoporosis, and frailty, not just clogged arteries.
So while high LDL is mostly about vascular risk, chronic inflammation hits many organ systems at once. That’s why many longevity people would say: if you forced them to pick a single underlying villain, inflammation is “more global”.
Query: “What blood test best measures inflammation?”
Answer: High-sensitivity C-reactive protein (hs-CRP) – the longevity favorite
What it measures: A liver protein that rises when the body is inflamed.
Why it’s favored:
Detects low-grade, chronic inflammation (values in the 0.5–10 mg/L range).
Strongly associated with cardiovascular risk and overall mortality, even after adjusting for cholesterol and other risk factors.
For someone interested in healthspan and lifespan, this is usually the single most informative, practical marker to track over time.