Thanks for this info. I use the Aktiia blood pressure monitor which measures BP 24/7 non-inflationary at the wrist.
They just released a new updated version in the UK, people can use a forwarding service to get it, if app is found in their local app / google play store.
Thanks for the advice; it looks amazing; how accurate is it? The reviews are extremely bad, especially many reviews mention a 10–15 mm Hg difference between Aktiia and their traditional BP inflatable cuff:
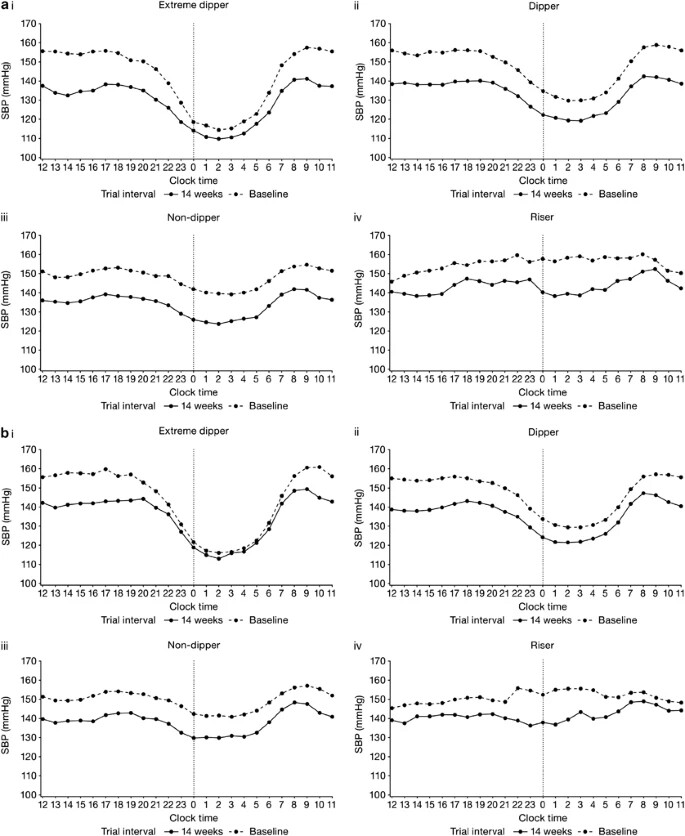
I dug more, almost all research papers on Aktiia are conducted by… Aktiia. One recent exception is Evaluation of the ability of a commercially available cuffless wearable device to track blood pressure changes. They found that the daytime average found by Aktiia was correct but that the night-time one was significantly off (+15.5 mmHg). They concluded: “This cuffless wearable device did not accurately track night-time BP decline and results suggested it was unable to track medication-induced BP changes.”
Aktiia answered: Inadequate study designs for the evaluation of blood pressure monitoring devices and their potential misleading conclusions - PMC
I find their answer unconvincing… They even “agree with the results showing that the nighttime dip measured by Aktiia was significantly smaller compared to ABPM”
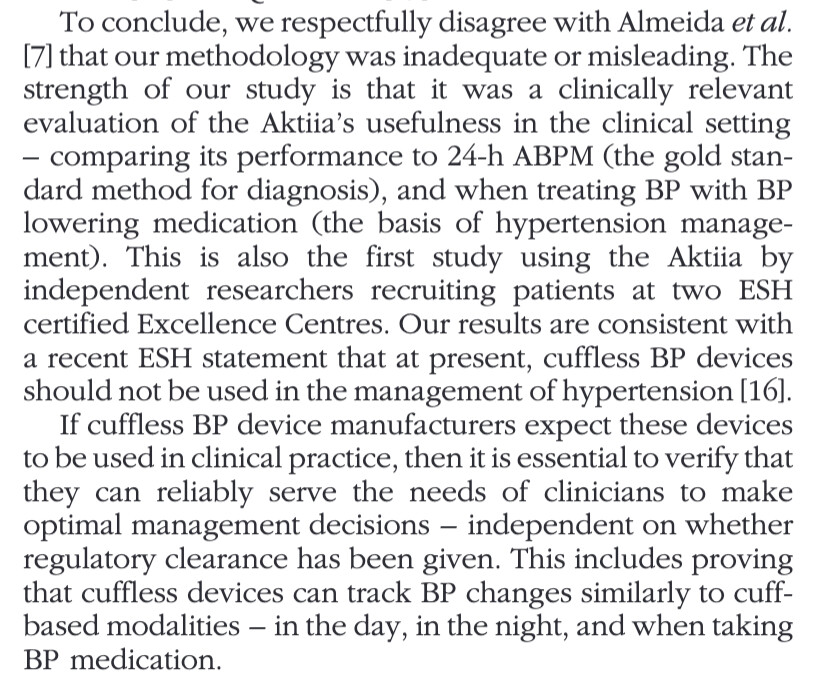
The researchers answered to Aktiia: Reply to ‘Inadequate study designs for the evaluation of blood pressure monitoring devices and their potential misleading conclusions’:
Still, I’m tempted to buy one… At least the above paper shows that the daytime average is correct and it’s good to know that night-time values are probably overstated.
[EDIT: Peter Attia is bullish on it though: Peter Attia Is Bullish on Aktiia's Continuous Blood Pressure Monitor - PodClips ]
[EDIT2: Eric Topol as well: A continuous blood pressure monitoring bracelet ]
[EDIT3: Bought it, I’ll report after I get it and test it…]
0.45±7.75 systolic and 0.38±6.86 diastolic.
I cannot do any other BP measurement than 24/7 even though it might be slightly less accurate, I think regular cuffs have about the same accuracy as Aktiia. Impossible to get data at night, continuously measuring BP to get as many datapoints with dubious accuracy at daytime as well, would be a grind.
Make sure it is the new version that is water proof etc, I bought just before the announcement and all of the fixes they mention were something I noticed was a problem.
Yes, I bought the “NEW Aktiia 24/7 Blood Pressure Monitor - Medium” but I have no idea when it will be delivered… (It says: “Your pre-order has been received. You will be automatically charged for your order via your selected payment method when your pre-order is released on at a future date.”)
Are you taking an anti-hypertensive drug? If yes, have you noticed a difference in your BP variability and, in particular, in your night-time patterns?
It looks like telmisartan is also better at “smoothing” BP fluctuations, especially at night: Effect of telmisartan vs. ramipril on ‘dipping’ status and blood pressure variability: pooled analysis of the PRISMA studies
According to these papers, CCBs are best for BPV reduction:
- Effect of antihypertensive treatment on 24-h blood pressure variability: pooled individual data analysis of ambulatory blood pressure monitoring studies based on olmesartan mono or combination treatment: “The largest reduction of BPV with treatment was observed in our study in patients taking a two or three drug combination treatment, particularly those combinations including a long-acting ARB (olmesartan) and a dihydropyridine calcium-channel blocker (amlodipine or azelnidipine) and/or a thiazide diuretic (hydrochlorothiazide). Such a result could be expected as consistent with literature reporting calcium-channel blockers, mainly belonging to the dihydropyridine class, as the most effective antihypertensive agents in reducing BPV, whereas ARBs and ACE inhibitors (the prevalent drug classes included in the monotherapy group of our study), have a modest effect on this parameter [11,41–43].”
- Blood Pressure Variability and Therapeutic Implications in Hypertension and Cardiovascular Diseases: “Despite most first-line antihypertensive medications contribute to reduce both short and long term BPV, calcium channel blockers (CCBs) as monotherapy or fixed-combination therapy appear to be the most effective on BPV control.”
Nope, I haven’t tried an anti-hypertensive drug yet, still working on lifestyle changes and optimizing lipids. But I will def work on BP if lifestyle isn’t enough which I don’t think it will.
Thanks. Please report the results of your tests. I’m super interested in seeing the impact of lifestyle changes and drugs on the Aktiia charts.
Looks like the Apple Watch 10, expected for Sept 2024, will have a BP monitor: Apple Watch Plans Hypertension, Sleep Apnea Detection, Other Health Updates - Bloomberg
However, “This sensor will not offer exact numbers the same way the cuff in a doctor’s office does, but it can detect changes and, importantly, elevations in blood pressure” ( New Apple Watch will detect blood pressure and sleep apnea: Report ). Hopefully, in a few years, the Apple Watch will measure both BP and glucose continuously ![]()
I use Aktiia for over a month and I am quite happy with accuracy if not with not being waterproof and very uncomfortable and hard to adjust band (it needs accurate adjustment to be able to measure your BP, it wont measure it if it is too tight or too loose).
I explained in another post that I was testing its optical sensor accuracy with measuring with cuff at the same time and I got results within few points difference, which is good enough IMO.
I am not taking any antihypertensive drugs but sometimes take beta-blocker propranolol for my headache and since it lowers BP this was measured by Aktiia as well and it was measured in the same quantity propranolol studies suggest. The days I take propranolol my daily average drops about 5 points and nighttime BP same. It also detects the rise in my BP caused by alcohol, if I have three or more units in the evening my night BP stays elevated. As these changes are quite low (within 5 points) and Aktiia detects them consistently I have no problems with its accuracy. But I guess it depends a lot on activating the optical sensor and probably in some people it is difficult to measure BP with optical sensor.
But can’t wait when Aktiia type of measuring will be available in Apple watch.
Interesting 2023 paper: Population-based discovery and Mendelian randomization analysis identify telmisartan as a candidate medicine for Alzheimer's disease in African Americans - PubMed
Telmisartan is associated with lower risk of Alzheimer’s disease (AD) in African Americans (AAs). Telmisartan is the only angiotensin II receptor blockers having PPAR-γ agonistic properties with beneficial anti-diabetic and renal function effects, which mitigate AD risk in AAs. Mendelian randomization (MR) analysis demonstrates the specificity of telmisartan’s protective mechanism to AAs.
The trial of telmisartan for AD prevention among AAs has just ended and we’re waiting for the results: Health Evaluation in African Americans Using RAS Therapy (HEART)
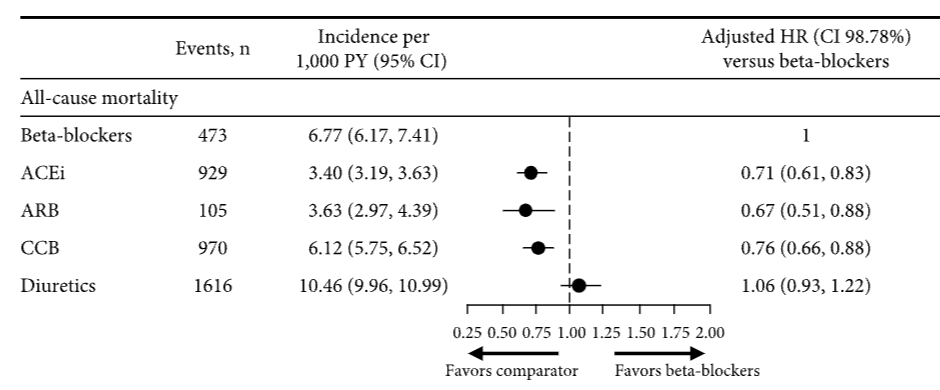
In the UK, once adjusted for baseline confounders such as angina, diabetes mellitus, and BP, the risk of all-cause mortality was lowest in patients treated with ARBs (then ACEi, then CCBs, then beta-blockers, then diuretics):
I’d like to find larger studies on all-cause mortality, with dihydropyridine calcium channel blockers (DCCBs like amlodipine) vs non-dihydropyridine calcium channel blockers and thiazide diuretics vs other diuretics. Can’t find anything…
I take lisinopril, an ACE-I. I don’t know what it does for my life expectancy, but it keeps a tight lid on my blood pressure, which usually hovers around 110/80.
Telmisartan really seems to be an outlier among ARBs with unique properties. In this paper just published in the American Journal of Hypertension: “BP control was similar in both groups; however, telmisartan users exhibited significantly lower visit-to-visit BP variability” (BPV). (Three-Year Cardiovascular Outcomes of Telmisartan in Patients with Hypertension: An Electronic Health Record–Based Cohort Study Get access Arrow)
The adjusted 3-year MACE rate was similar between telmisartan users (4.6%) and other ARB users (4.7%, log-rank p = 0.75), with comparable safety profiles, but as “BPV had a stronger association with dementia and cognitive impairment than mean BP levels” I would bet that telmisartan users will have lower rates of dementia and all-cause mortality years later (and that’s what most studies tend to find).
Other interesting properties of telmisartan vs other ARBs:
- “By leveraging the National Health Insurance Research Database, a Taiwanese study [78] found that the dementia risk was lower in telmisartan users compared with other ARB users (hazard ratio, 0.72; 95% CI, 0.53 to 0.97; p = 0.030). The authors attributed this to the greater effect of telmisartan on increasing PPAR-γ expression.” (Angiotensin Receptor Blockers and Cognition: a Scoping Review 2023)
- “Among seven ARBs (azilsartan, candesartan, irbesartan, losartan, olmesartan, telmisartan, and valsartan), telmisartan was the most effective ARB for the increase of adiponectin secretion” (Telmisartan is the most effective ARB to increase adiponectin via PPARα in adipocytes 2022)
- “Telmisartan can better improve IR compared with other ARBs.” (Telmisartan Improves Insulin Resistance: A Meta-Analysis 2018)
Also, for Covid: “Death by day 30 was reduced in the telmisartan-treated group (control 22.54%, 16/71; telmisartan 4.29%, 3/70 participants; p = 0.0023). Composite ICU, mechanical ventilation or death was reduced by telmisartan treatment at days 15 and 30. No adverse events were reported.” (Telmisartan for treatment of Covid-19 patients: An open multicenter randomized clinical trial 2021)
New paper on Covid: Discovery of inhibitors of the SARS-CoV-2 S protein through computational drug repurposing 2024
After the sieving process, a final list of 10 candidates was proposed, compounds which were subsequently purchased and tested ex-vivo . The results identified estradiol cypionate and telmisartan as inhibitors of SARS-CoV-2 entry into cells. Our findings demonstrate that the methodology presented here enables the discovery of inhibitors targeting viruses for which high-resolution structures are available.
great post on Telmisartan. I was very curious because Peter Diamandis is using it and he has been at this for a long time.
Yes given its safety profile (same as placebo), its high BP lowering efficacy, its half life (it’s the longest acting ARB) and its other unique properties (insulin sensitivity, PPARa, etc.), it’s a no brainer that telmisartan is the best among all antihypertensives acting on the RAS (so ARBs and ACEIs). See also: Why Telmisartan Is Best For Blood Pressure - Life Extension
As I said in the other topic, I don’t know if there’s such a clear winner for CCBs (it’s dihydropyridines for sure but among them is it amlodipine? Probably because of its uniquely long half life) and diuretics (it’s probably thiazides and thiazide-likes, but which one? My bet is on indapamide slow release that seems to have a long half life and less association with insulin resistance and dyslipidemia).
Angiotensin Receptor Blockers Do Not Reduce Risk of Myocardial Infarction, Cardiovascular Death, or Total Mortality: Further Evidence for the ARB-MI Paradox
https://www.ahajournals.org/doi/full/10.1161/circulationaha.117.026112
Individual trials of angiotensin II receptor blockers (ARBs) and systematic meta-analyses have repeatedly demonstrated the ARB class to significantly reduce systemic blood pressure, stroke, and the subsequent development of heart failure and diabetes mellitus.1 However, no individual trial or meta-analysis has observed an impact of ARB treatment on the incidence of myocardial infarction (MI), cardiovascular mortality, or all-cause mortality (Table). All-cause mortality is the most comprehensive summary indicator of cardiovascular benefit of treatment2 and, consequently, it is surprising that ARBs have no impact given the other clinical benefits we have just acknowledged.
A systematic review/meta-analysis conducted by Bangalore et al3 demonstrated that in 20 trials of ARB versus placebo (n=66 282) and 21 trials of ARB versus active comparator (n=39 738), ARB in no individual trial improved all-cause mortality. Furthermore, when the trials were analyzed in combination, the impact of ARB on mortality was precisely zero compared with placebo (odds ratio, 1.01; 95% confidence limit, 0.96–1.06) and virtually zero compared with an active comparator (odds ratio, 0.99; 95% confidence limit, 0.95–1.03). Placebo-controlled trials are the most rigorous method of assessing treatment efficacy (as well as harm), and, consequently, it is concerning that other meta-analyses of ARBs versus placebo-controlled trials have also reported a lack of mortality reduction in patients with high risk (Savarese),4 those with diabetes mellitus (Cheng),5 and patients with hypertension (Thomopoulos et al),6 as well as no reduction in MI or cardiovascular mortality (Table).
Thomopoulos et al6 also reported the impact of different drug classes compared with placebo in the treatment of systemic hypertension. Indapamide, calcium channel blockers, and angiotensin-converting enzyme inhibitors (ACEIs) all statistically significantly reduced mortality, whereas 4 other drug classes reduced mortality but not to a degree that was of statistical significance. ARB was the only drug class that failed to reduce death compared with placebo, despite representing the largest group of patients studied (n=65 256) and despite an average blood pressure reduction of 3.7/2.0 mm Hg. Because stroke was reduced by ARBs, cardiovascular and all-cause mortality must have been driven by an excess risk of fatal MI and sudden death. ACEIs but not ARBs reduced coronary heart disease (including nonfatal MI) and cardiovascular death (including fatal MI6), despite both being inhibitors of the renin-angiotensin-aldosterone system.
ACEIs suppress angiotensin II, thereby preventing pathological effects, but they also prevent the breakdown of bradykinin, thereby inducing additional cardioprotective effects. This profile is distinct from the one achieved by use of an ARB that induces selective antagonism of the AT1 angiotensin II receptor, inhibiting a negative feedback loop and consequently increasing angiotensin II levels by 200% to 300%. This may lead to MI as a result of stimulation of the AT2 receptors, which are markedly upregulated and active in atheromatous plaques.1 ACEIs in meta-analyses of placebo-controlled trials conducted in parallel to the ARB meta-analyses discussed above (Thomopoulos et al,6 Savarese,4 Cheng,5 Bangalore et al3) demonstrated a robust 9% to 11% risk reduction in all-cause mortality, 10% to 17% risk reduction in cardiovascular mortality, and 17% to 19% risk reduction in MI (all P<0.05; Table). The divergent effects of ACEI and ARB on both all-cause and cardiovascular mortality are despite their comparator arms having similar risks of both (7.8% versus 9%, 4.7% versus 5.2%, respectively).3
These observations are consistent with an earlier meta-analysis1 that reported that ARBs versus all comparators (11 trials, n=55 050) did not reduce mortality (odds ratio, 1.01; 95% confidence interval, 0.96–1.06, P=0.8) and the risk of MI actually increased 8% (odds ratio, 1.08; 95% confidence interval, 1.01–1.16; P=0.03), with that increase qualitatively apparent in 9 of the trials and statistically significant in 2. This article also included a parallel meta-analysis of ACEI trials. ACEIs versus all comparators (39 trials, n=150 943) reduced the relative risk of total mortality 9% (P<0.0001) and MI by 14% (P<0.0001). The divergent effects in the parallel ACEI and ARB meta-analyses on MI and death were marked, despite their comparator arms having similar cardiovascular risks; rates of global death, MI, and stroke (cerebrovascular accident) were essentially no different (13% versus 14%, 5.8% versus 6.3%, and 4.2% versus 4.4%, respectively). In addition, blood pressure lowering comparable to the risk reduction in stroke, a blood pressure–dependent phenomenon, was also similar.
Divergent cardiovascular effects of ACEIs and ARBs were also confirmed in a meta-regression analysis (n=146 838) by the BPLTTC (Blood Pressure Lowering Treatment Trialists’ Collaboration), as well as being independent of blood pressure lowering.1 For any given blood pressure reduction, ACEIs also reduce the risk of coronary heart disease by an additional 9% (P=0.002), independently of the effects of blood pressure lowering. In contrast, ARBs had no blood pressure–independent effects on coronary heart disease; rather, there was a small, nonsignificant increase in the risk of harm of 7% (–7%: 95% confidence interval, 7 to –24; P=NS), a phenomenon we have called the ARB MI paradox. Specifically, it is paradoxical that no net benefits are observed with ARBs. Furthermore, and most important, for any given blood pressure reduction, ACEIs reduced the risk of MI and death an additional 15% (P=0.002) above that of an ARB.
Head-to-head trials of ARB versus ACEI are of interest, but there is a paucity of data. In the ONTARGET trial (Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial),2 the largest ACEI versus ARB controlled trial reported to date (n=17 118), the ARB telmisartan was not statistically equivalent to the ACEI ramipril for a combined cardiovascular end point. The US Food and Drug Administration approved telmisartan as a second-line therapy for those high-risk patients who are ACEI intolerant (New Drug Application 20–850). This decision was influenced by a lack of superiority of telmisartan compared with placebo in the parallel TRANSCEND trial (Telmisartan Randomized Assessment Study in ACE Intolerant Subjects With Cardiovascular Disease), consistent also with the HOPE-3 trial (Heart Outcomes Prevention Evaluation-3) conducted in patients at intermediate risk (n=12 705; follow-up, 5.6 years)4 in whom candesartan combined with hydrochlorothiazide failed to reduce a combination of cardiovascular events despite a robust reduction in blood pressure of 6.0/3.0 mm Hg.
Angiotensin Receptor Blockers May Increase Risk of Myocardial Infarction
https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.105.594986
Candesartan failed the ITP.
Interesting with your conclusions here. It is exactly what I’ve concluded. I tell my patients it is best to hit multiple pathways at low-moderate dose, as pushing the dose of any drug yields very little added benefit and often results in side effects.
I generally start with Telmisartan, and don’t push beyond 40 mg, then add Amlodipine 2.5 mg and max at 5 mg, then add indapamide 1.25 mg … The indapamide doesn’t get maximal effects until at least 45 days.
I recently had someone who for 40 years has had uncontrolled hypertension and interestingly it was the indapamide at the end that took them down to a sensible range. I goal for SBP of 115 mmHg - which is naturally a big ask of the drugs when someone is running 180-190 mmHg long term.
In this individual, it wasn’t until week 4 of indapamide that we finally got the movement needed, as much as the first 2 drugs helped a bit.
I prefer this diuretic, as in low dose it rarely affects electrolytes.