We know that VO2Max levels are a key driver of healthy longevity.
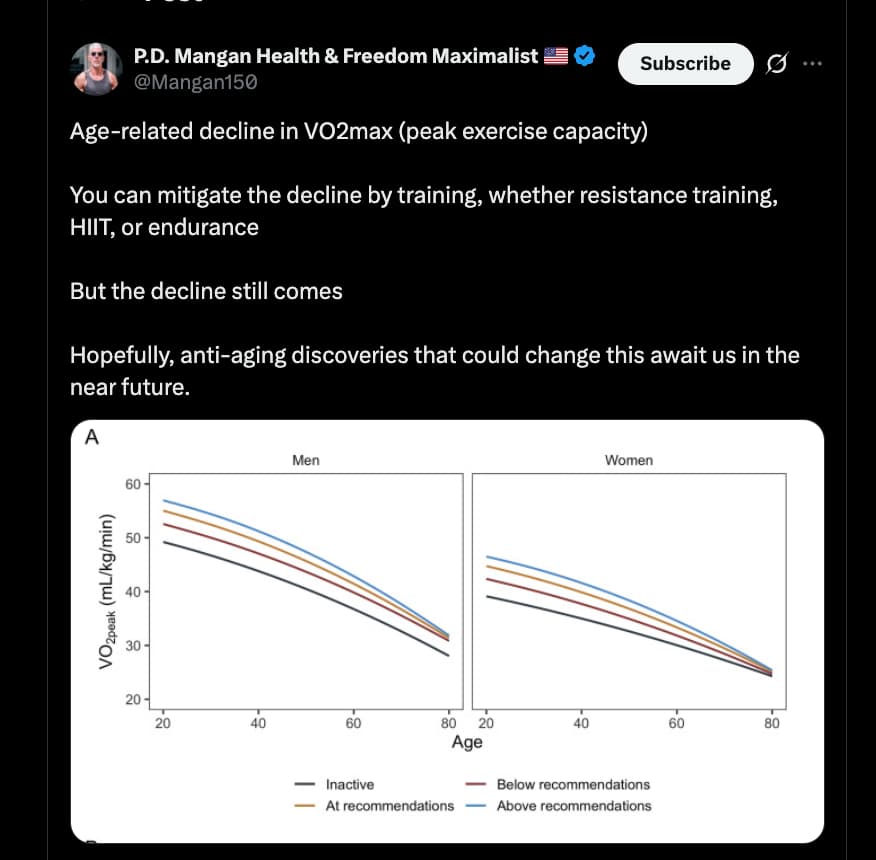
So this graph from the main VO2Max thread got me thinking… what, if anything, is showing benefits at slowing or stalling this decline, other than exercise?
Below are some very interesting results from my CGPT queries. Rapamycin looks to be one of the best potential compounds, and I suspect that the new paper coming out from Brad Stanfield will further confirm this… and more human clinical trials need to be done.
Rapamycin / mTOR inhibition
- In old low-capacity runner rats, rapamycin increased grip strength and attenuated age-related decline in maximal running distance vs controls.
- A 2025 mouse study using PoWeR training showed rapamycin did not blunt improvements in maximal exercise capacity from training, though frequent dosing impaired glucose tolerance.
My Prompt:
I want you to look more at the actual reasons why vo2max in humans decrease with age. Given current theories on this topic, What are the possible exogenous compounds that could reasonably be identified, or have been hypothesized, might plausibly maintain human vo2max levels during aging? I am less interested in clinical validation done to date, and more of a mechanistic look, and a list of compounds that are good bets to test going forward.
CGPT5.1 Response:
Alright, here’s the blunt version: if we only care about mechanisms and expected VO₂max effect size (not legality, not health trade-offs, not clinical proof), the “big rocks” are obvious: things that increase hemoglobin, turn muscle into a fat-burning engine, or radically upgrade mitochondrial quality.
Below is a stack-ranked list based on expected effect size on VO₂max in aging humans , assuming:
- Person is already doing reasonable endurance training.
- Effect size = magnitude of VO₂max improvement / slowing of decline vs same-age, similarly trained control.
- This is conceptual, not a dosing guide or medical advice.
Tier 0 (Context): Training & Altitude
Just to anchor:
- Endurance training can roughly halve the age-related decline vs sedentary.
- Living/training at altitude (natural HIF/EPO stimulus) can add another ~5–15% VO₂max vs the same person at sea level (with optimized protocols).
Everything below sits on top of that.
Tier 1 – Mechanistically Massive Levers (10–20%+ VO₂max Potential)
These are the “nuclear options” mechanistically. Not endorsing, just ranking.
1. Exogenous EPO / HIF-Prolyl Hydroxylase Inhibitors (e.g., roxadustat)
Mechanism: ↑ EPO → ↑ RBC mass → ↑ hemoglobin → ↑ arterial O₂ content → higher peak O₂ delivery.
- This is the most direct way to force VO₂max up: more oxygen-carrying capacity.
- In athletes, illicit EPO use ≈ +5–15% VO₂max, sometimes higher.
- In aging, where Hb often drifts lower, the relative impact could be big.
Effect-size rank: #1 – biggest single lever on raw VO₂max.
Longevity lens: high risk (thrombosis, hypertension, cancer signaling concerns).
2. PPAR-δ Agonists (e.g., GW501516 class)
Mechanism:
- Reprograms muscle toward type I oxidative fibers.
- ↑ Fatty acid oxidation, ↑ mitochondrial genes, ↑ endurance.
- Turns skeletal muscle into a chronic “trained” phenotype.
- In rodent models, this class is insanely powerful for endurance and work capacity even without training.
- Mechanistically, it hits both oxygen utilization and substrate efficiency, which are huge for VO₂max.
Effect-size rank: #2 – enormous mechanistic upside.
Longevity lens: abandoned due to carcinogenicity in animals. Huge red flag.
3. AICAR (Potent AMPK Agonist)
Mechanism:
- Mimics cellular energetic stress → activates AMPK → ↑ PGC-1α → ↑ mitochondrial biogenesis and oxidative capacity.
- In animals, chronically administered AICAR improves endurance dramatically.
- It basically forces a high-oxidative phenotype in muscle even with modest training.
Effect-size rank: #3 – very large mechanistic impact on mitochondrial density and utilization.
Longevity lens: not realistically usable long term; side-effect profile, practicality.
4. Myostatin Inhibitors / Follistatin Approaches
Mechanism:
- Inhibit myostatin → large increases in muscle mass and often strength.
- Bigger muscle + same or better capillarization and mitochondrial density ⇒ higher peak work output capacity, raising VO₂max.
- This is more indirect: VO₂max goes up because you can produce more power at max effort, not because of hemoglobin or mitochondria alone.
Effect-size rank: #4 – potentially large VO₂max bump if training is aligned.
Longevity lens: unknown long-term effects; theoretical increased O₂ demand + cardiac load.
Tier 2 – Strong but More Nuanced Levers (5–10% VO₂max Impact OR Significant Slope Change)
These have good mechanistic depth and are more plausible in a “serious but not insane” longevity stack.
5. Rapamycin / Rapalogs (Intermittent, low–moderate dose)
Mechanism:
- ↓ mTORC1 → ↑ autophagy and mitophagy (esp. with fasting/exercise).
- Long term: preserves mitochondrial quality, reduces inflammaging, maintains muscle fiber function.
This is likely less about acute VO₂max boost and more about slowing the age-related decline of mitochondrial function and cardiac/vascular aging.
- Realistically: could mean a 60- or 70-year-old looks more like a typical 50- or 60-year-old in max O₂ utilization capacity, if paired with training.
Effect-size rank:
- Acute: modest.
- Long-term trajectory: very high for preserving VO₂max vs normal aging.Call it #5 overall.
6. Urolithin A (Mitophagy Enhancer)
Mechanism:
- Activates mitophagy (PINK1–Parkin pathway) → clears defective mitochondria → healthier mitochondrial pool.
- Human data already shows improvements in muscle endurance and mitochondrial gene expression.
Again, preservation of function > acute doping effect. This is about keeping muscle oxidative capacity “younger” per decade.
Effect-size rank: #6 – strong mechanistic candidate for slowing VO₂max decline with age.
7. Beet/Nitrate Supplementation (Dietary Nitrates, Potassium Nitrate, etc.)
Mechanism:
- ↑ NO bioavailability → vasodilation, improved muscle perfusion, ↓ O₂ cost of submax work.
- In both young and older adults, nitrates typically yield ~2–5% VO₂max and performance bumps.
Effect-size rank: #7 – modest absolute VO₂max boost, but highly reliable and very mechanistic.
Great for “functional VO₂max” (what you can do in the real world).
8. PDE-5 Inhibitors (Tadalafil, Sildenafil)
Mechanism:
- Inhibit cGMP breakdown → prolonged NO signaling → better vasodilation.
- ↓ Pulmonary pressures, improved muscle perfusion; may reduce arterial stiffness with chronic use.
- VO₂max effect likely small–moderate alone, but could synergize with nitrates and training.
Effect-size rank: #8 – small acute effect, potentially meaningful chronically via better hemodynamics.
9. Telmisartan (ARB + Partial PPAR-γ/PPAR-δ Activity)
Mechanism:
- ↓ BP + arterial stiffness (ARB).
- Mild PPAR-δ agonism → small shift toward more oxidative muscle phenotype and improved insulin sensitivity.
- Likely a chronic slope modifier: less hemodynamic damage, better vascular compliance, better substrate use → VO₂max decline slowed.
Effect-size rank: #9 – moderate, mostly via long-term vascular and metabolic effects.
10. NAD+ Boosters (NR, NMN, etc.)
Mechanism:
- ↑ NAD+ → ↑ SIRT1/SIRT3 → ↑ PGC-1α → mitochondrial biogenesis and improved mitochondrial function.
- Strength of effect likely highly context dependent (age, baseline NAD+, training, diet).
Effect-size rank:
- Acute: mild.
- Chronic trajectory: #10 – modest but plausible preservation effect on VO₂max via mitochondrial maintenance.
Tier 3 – Moderate but Plausible (1–5% Direct or Indirect Effects)
These are more “fine-tuners” than core drivers.
11. Mitochondria-targeted Antioxidants (MitoQ, SkQ1, etc.)
Mechanism:
- Localized ROS scavenging at the ETC → protect complexes, maintain efficiency, reduce oxidative mtDNA damage.
- Likely not huge VO₂max boosters on their own, but could preserve quality of respiration over time.
Effect-size rank: #11 – small–moderate, supportive.
12. Epicatechin (Cocoa-derived)
Mechanism:
- ↑ NO, ↑ capillary density in muscle (preclinical), possible SIRT1 activation.
- Potential improvements in microvascular function.
Effect-size rank: #12 – small acute effect, modest chronic help for microcirculation.
13. Citrulline (Better NO Precursor Than Arginine)
Mechanism:
- Sustained arginine → NO production → vasodilation and perfusion.
- Likely < nitrates effect but similar axis.
Effect-size rank: #13 – modest; useful adjunct to NO-axis strategy.
14. Creatine
Mechanism:
- ↑ Phosphocreatine buffer → better high-intensity work → allows higher training loads.
- The VO₂max benefit is indirect: greater training gives better central and peripheral adaptations.
Effect-size rank: #14 – indirect but real via increased training capacity.
15. CoQ10 / Idebenone
Mechanism:
- Electron carrier / ETC support.
- Likely only meaningful in deficiency, statin users, or mitochondrial disease.
Effect-size rank: #15 – low except in specific subgroups.
16. L-Carnitine / Acetyl-L-Carnitine
Mechanism:
- Facilitates fatty acid transport into mitochondria → better fat oxidation at submax exercise.
- Some endurance benefit; VO₂max effect is typically small.
Effect-size rank: #16 – minor, mostly metabolic efficiency at submax loads.
How I’d Distill This for a Serious, Longevity-Minded Experimenter
If you strip out the “insane but effective” options (EPO, GW, AICAR, hardcore myostatin inhibition) and focus on plausible long-term VO₂max preservation, the mechanistic priority list looks more like:
- Rapamycin / intermittent mTOR inhibition – slow multi-system aging of the O₂ transport/utilization chain.
- Urolithin A – maintain mitochondrial quality in skeletal and cardiac muscle.
- Nitrates (dietary or controlled salt forms) – acute boost + chronic endothelial health.
- PDE-5 inhibitor (low-dose, extended) – vascular function, NO axis, pulmonary pressures.
- Telmisartan (if hypertensive / borderline) – long-term vascular remodeling and mild PPAR-δ help.
- NAD+ booster – mitochondrial biogenesis support (especially in older ages).
- Mitochondria-targeted antioxidants – protect ETC and mitochondrial integrity.
- Epicatechin / citrulline – extra NO/capillary tuning.
- Creatine – raises ceiling for training output.
Everything else is either:
- Mechanistically powerful but too dirty/dangerous (EPO/HIF-PH, GW501516, AICAR).
- Or too small relative to the big structural levers (CoQ10, carnitine, generic antioxidants).
My Prompt:
What are possible exogenous compounds that have been hypothesized or tested to help maintain human vo2max levels during aging?
CGPT5.1 Response:
Short version:
There is no pill that reliably preserves VO₂max with aging in otherwise healthy humans. A few agents nudge peak VO₂ or endurance in specific settings, but effect sizes are small and often disease-specific. Below is a map of what’s actually been tested or seriously hypothesized.
1. Human data where VO₂max / peak VO₂ was actually measured
1.1 Inorganic nitrate (beetroot juice, nitrate salts)
Mechanism
- Dietary nitrate → nitrite → nitric oxide
- ↓ O₂ cost of submax work, improved muscle blood flow and vasodilation, which can translate into slightly higher VO₂max / peak VO₂.
Evidence
- A 2025 meta-analysis of beetroot juice in healthy adults found a small but statistically significant increase in VO₂max (SMD ~0.16; 95% CI 0.01–0.31). Authors explicitly describe the effect as negligible in magnitude.
- In older adults with controlled hypertension/HFpEF, supervised aerobic training plus high-nitrate beetroot juice improved peak VO₂ and submaximal endurance, though the main driver was the training; nitrate mainly improved BP and submax exercise tolerance.
Takeaway:
Nitrate donors are the only over-the-counter thing with halfway decent human VO₂max data, but we’re talking low-single-digit % changes, not “preserve your 30-year-old VO₂max at 70”.
1.2 ACE inhibitors (Perindopril)
Mechanism
- ↓ afterload, improved endothelial function and muscle perfusion; ACE inhibitors also have some data in sarcopenia and physical function.
Evidence (older / diseased populations)
- In functionally impaired older adults without overt HF, perindopril improved exercise capacity—mainly 6-minute walk distance—with an effect size similar to ~6 months of exercise training in that population.
- Trials in older patients with LV dysfunction or HF show better 6-min walk distance and symptoms; 6-min walk is moderately correlated with peak VO₂, but VO₂max was not always directly measured.
- A later RCT in sarcopenic older adults found no added benefit of perindopril on walking distance beyond exercise training.
Takeaway:
In frail / HF populations, ACE inhibitors can improve functional capacity and likely peak VO₂ somewhat, but this is heart-failure pharmacology, not a general VO₂max-preservation strategy for healthy aging.
1.3 SGLT2 inhibitors (empagliflozin, dapagliflozin, etc.)
Mechanism
- Osmotic diuresis, ↓ preload/afterload, improved myocardial energetics; huge benefits on HF outcomes.
Evidence
- A 2024 meta-analysis of 17 HF trials found SGLT2i improved symptoms and quality of life, and some studies showed better 6-min walk distance; but changes in peak VO₂ on CPET were small or absent overall.
Takeaway:
SGLT2i are excellent HF drugs with survival benefit; not convincingly VO₂max-enhancing for otherwise stable older adults.
1.4 Mitochondria-targeted antioxidant MitoQ
This one is instructive because it’s a negative result.
Evidence
- A 2023 trial in physically inactive females: a single acute dose of MitoQ reduced VO₂max versus placebo, apparently by impairing ventilatory responses to exercise.
- A 2024 meta-analysis (8 studies, n≈188) concluded MitoQ reduces exercise-induced oxidative damage but does not improve endurance performance (SMD for performance −0.50; 95% CI −1.39 to 0.40).
Takeaway:
Killing mtROS isn’t a free lunch: acute high-dose MitoQ can actually worsen VO₂max. Not a VO₂max preservation strategy.
1.5 Erythropoiesis-stimulating agents (EPO and analogues)
- In both patients and doped athletes, increasing hemoglobin clearly raises VO₂max by ↑ O₂-carrying capacity. This is textbook physiology.
- But: thrombosis, hypertension, stroke, cancer progression signals; and in sport it’s banned.
Takeaway:
Yes, EPO works on VO₂max, but the risk/ethics profile makes it irrelevant for legitimate aging interventions outside specific anemia indications.
2. Human data: “fitness-adjacent” compounds with weak or indirect VO₂max evidence
These come up in longevity circles a lot, but VO₂max data are thin.
2.1 NAD⁺ precursors (NR, NMN)
Mechanism
- Boost NAD⁺ → support mitochondrial function, sirtuins, etc.
Evidence
- NR RCTs in middle-aged/older adults show:
- ↑ NAD⁺ metabolites and improved vascular function (↓ SBP, arterial stiffness)
- No robust, reproducible gains in VO₂max; most trials don’t even measure it, or report null for exercise capacity.
- A 2025 pilot trial is testing NR + exercise in hypertensive older adults, focusing on BP and muscle, not VO₂max as primary.
Takeaway:
NAD⁺ precursors are plausibly cardio-protective , but not yet shown to maintain VO₂max with aging.
2.2 Melatonin
Mechanism
- Antioxidant, circadian alignment, possible mitochondrial effects.
Evidence
- Acute melatonin before maximal running: ↓ oxidative stress markers, no improvement in performance in trained athletes.
- Animal work shows melatonin can improve exercise tolerance, PGC-1α signaling and substrate handling in rodents, but that’s far from “preserves VO₂max in aging humans”.
Takeaway:
Good for sleep, maybe recovery; not a validated VO₂max agent.
2.3 CoQ10 and related mitochondrial supplements
- Small HF trials report modest increases in peak VO₂ and exercise time with CoQ10, but data are disease-specific and heterogeneous; essentially no robust trials in healthy older adults linking CoQ10 → preserved VO₂max with age.
2.4 “Classic” ergogenic aids (caffeine, beta-alanine, sodium bicarbonate, creatine)
- Clear benefits on performance, time to exhaustion, power output in specific protocols.
- Effect on measured VO₂max is generally minimal; they mainly alter perception of effort, buffer H⁺, or support phosphocreatine—not the O₂ transport chain per se.
- There’s no longitudinal human data showing they slow the age-related decline in VO₂max.
3. Animal / speculative “exercise mimetics” and geroprotectors
These are mechanistically interesting but not ready for “VO₂max preservation” claims in humans .
3.1 Rapamycin / mTOR inhibition
- In old low-capacity runner rats, rapamycin increased grip strength and attenuated age-related decline in maximal running distance vs controls.
- A 2025 mouse study using PoWeR training showed rapamycin did not blunt improvements in maximal exercise capacity from training, though frequent dosing impaired glucose tolerance.
Human reality:
We have no human VO₂max data. At best, rapa might preserve some physical function via geroprotective mechanisms, but anything about human VO₂max is extrapolation.
3.2 PPARδ agonists (GW501516 / “Cardarine” etc.)
- In mice, GW501516 plus training produced huge increases in endurance—running distance ↑ 30–70%, with a shift toward oxidative muscle fibers and enhanced FAO.
But:
- Tumorigenicity signals in animals → development stopped; WADA-banned; sold in gray-market bodybuilding circles with zero safety data.
Takeaway:
Powerful proof-of-concept exercise mimetic in rodents , but not a clinically acceptable VO₂max drug .
3.3 AMPK agonists (AICAR) and combinations
- AICAR and AICAR+PPARδ agonists in mice increase endurance and oxidative muscle phenotype.
- Again: no human aging/VO₂max preservation data, and drug-development largely stalled due to safety/abuse concerns.
3.4 Melatonin, again (rodent endurance)
- Rodent endurance studies show melatonin can increase time to exhaustion and enhance exercise-induced PGC-1α and glycogen sparing.
- Translational gap remains large.
4. So what actually matters for maintaining VO₂max with aging?
Putting the literature together:
- Training dwarfs drugs.
- Decades of data show that staying in the top VO₂max quartiles for age is associated with massive mortality risk reductions; drugs so far move VO₂max by at most a few percent in narrow groups, whereas well-designed training can double VO₂max from deconditioned baselines.
- Nitrate supplementation is the only halfway solid, legal, OTC candidate with direct VO₂max data.
- Expect small gains and maybe some help offsetting age-related declines in oxygen cost/vascular function, not miracle preservation.
- Cardiovascular drugs (ACEi, SGLT2i, etc.) help mainly by preventing disease progression.
- They may indirectly preserve VO₂max by preventing HF, ischemia, and vascular stiffness, but not by raising VO₂max above what your training and genetics would otherwise support.
- High-dose mitochondrial antioxidants around maximal exercise are not obviously helpful and may be harmful to VO₂max.
- The MitoQ data are a good cautionary tale: blunt ROS too much at the wrong time and you can acutely reduce VO₂max.