I visited pharmacies over here the past weeks, and it turned out Lmitrex in several European countries is only available per prescription. My GP agreed today to prescribe it, so I can finally give it a try once needed. Thanks for the recommendation.
Unfortunately my GP didn’t feel comfortable to prescribe Provigil for the fatigue. He didn’t feel comfortable with its potential side-effects/safety profile he said. (But on the other hand he also readily admitted that he didn’t really know what Provigil is normally prescribed for, and was using Google to find more info ![]() . I was too uninformed myself also).
. I was too uninformed myself also).
Sounds like his knowledge of provigil is limited.
I hope that the imitrex helps. Good chance that it will.
Indeed, you are right, and he mentioned that also. He mostly seemed worried that a side-effect of Provigil could be headaches, and on the other hand he was prescribing the Lmitrex against migraines. He said he thus wasn’t sure how one may interact with the other.
Thanks, happy to be able to try out the Lmitrex when needed.
Thanks so much, Mike: appreciate the Magnesium-recommendation. Sorry if I hadn’t been clear, but admittedly I only experience a headache on day 2-3 after dosing Rapamycin. So in that sense I certainly can’t complain ![]() . But since this headache seemed to be present for up to a day and quite unpleasant I wanted to do something about it.
. But since this headache seemed to be present for up to a day and quite unpleasant I wanted to do something about it.
I do take a Magnesium-supplement each day (albeit a low dose). But I had no idea Magnesium is sometimes also used as an acute treatment option for headaches, as discussed in the link you provided. Thanks, I may certainly want to give it a try also.
Indeed I complement the Rx meds I do take with quite a few natural/herbal alternatives (but try to avoid doing so those days I take Rapa). I think there is a place for both, albeit admittedly I’m somewhat concerned not just about CYP3a4 inhibition (and again after recently reading a post about piperines potential effect on Rapa serum levels), but also other potential interactions. Difficult to know if I may be doing my health a disservice ultimately. But that’s a topic for another thread of course ![]() .
.
After 5 weeks of stopping oral Rapamycin, I have recovered fully from the bacterial infection (which ended up not being too bad due to antibiotics!). I took a dose of 2 mg + GFJ + Metformin this morning + @AgeTron’s hair tonic. Hopefully there won’t be any more side effects!
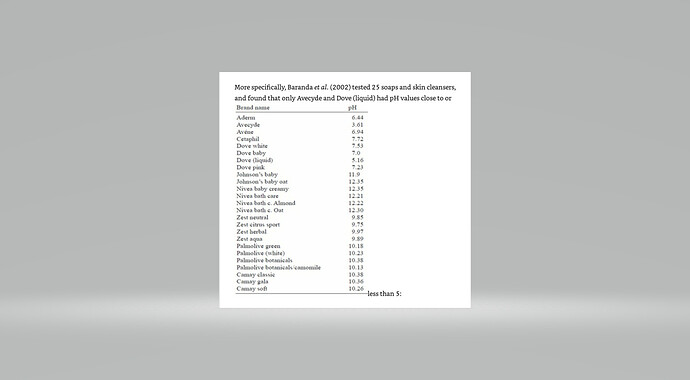
This comes from Michael Lustgarten’s free ebook. Microbial Burden. I hope the pic works:
Your skin maintains a ph of around 5.5 to stop bacterial infection. Soap has a ph of 9 usually, meaning it gives the bacteria like 6 hours of a loss of barrier function after every time you use soap. If you can read the chart above you will see there are only 2 soaps that work, Dove and a prescription soap that is unavailable here. I did buy the Dove and it cleans like crazy. This is what it looks like:
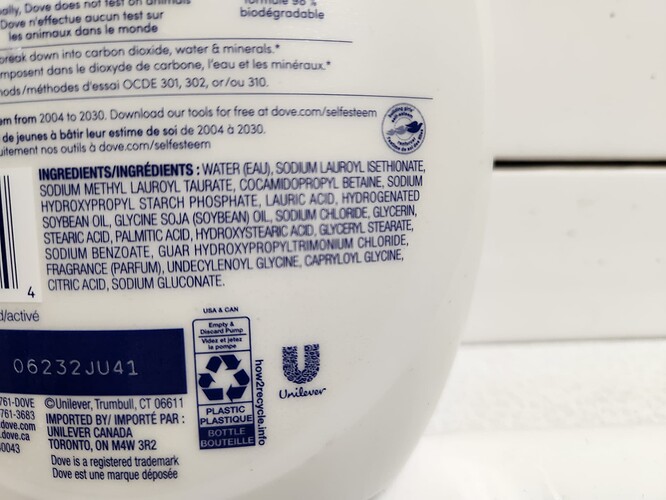
The label:
There was also a graph that he showed how Urea dramatically increases barrier function in the skin and 10% was the best rate. So I’ve been thinking about adding 10% urea to this liquid soap and trying that.
If taking Rapa reduces your ability to keep bacteria from entering your body through the skin then it may be important to pay attention to this. I’ve not had a rash but I only take 4 mg with GFJ every 12 days now.
Thanks for that. Actually I do use Dove exclusively as my cleaning soap. It comes in a variety of scents and the whole family likes it. ![]()
Dove in solid form looks to be a ph in the low 7’s. The only form of Dove that is ph 5.16 is the bottle pictured of liquid soap labelled for sensitive skin, hypoallergenic and says microbiome under that. I got it at Wal Mart.
I ordered the Urea. In the skin it turns on the CAMP gene which makes LL-37, an antimicrobial peptide. I’m guessing the AMP in CAMP stand for anti microbial peptide. Using Urea triples the amount of LL-37. It quaduples the amount of beta defensin-2, which is another antimicrobial peptide.
So washing with a basic soap (and that would be all soap since it is made with Lye and fat), gives the bacteria free reign of your skin to set up shop for about 6 hours. It wipes out your defense. Using the liquid Dove cancels that out so that it is as if you didn’t even wash. Using Urea triples one AMP and quadruples the other.
I never wash my face with soap. No need to, it just removes too much natural oil. I just rinse with water and use a facecloth. My skin is very good for my age. Really quite good for any age minus a few wrinkles.
I used to be the same regarding washing my face. I didn’t think it mattered. After a chat with my dermatologist, she said try a face wash and moisturizer. It has made a huge difference. I use the Dove liquid soap to wash and then I apply a simple Physiogel moisturizer. My skin looks a lot better! And if you look younger, you feel younger.
Crazy, my dermatologist told me I would be better off not using any soap on my face. And, I am happy with that and the results.
Of course, women who use make-up might need soap.
Of course we’ve had soap for a little over 2000 years, so it must be ok. But before that there were people looking almost exactly like us for 250,000 years. So it must be ok to go without too.
I would like to go the other way. I get tired of washing my body manually every night, but it is necessary because of my job (and the way I do it). I need to be clean so the bed doesn’t get dirty. They have washers for clothes, dishes,cars…there should be a baby bidet, this is a grudge from my youth and 5 kids. I want to just step into a cabinet and maybe a seal around the face, hit a button and relax and enjoy the show. Why has this not been done? You’re an engineer, this could be your lasting contribution to mankind.
There are times I have to use soap on my face, but rarely. I just shower without putting soap on my face.
Unfortunately, I was an electronics design engineer, so I don’t know anymore than the average man about plumbing.
They have full-body showers where many shower jets are placed around the booth and they effectively spray your body with water. Lots of people have them. Most people only have the top-down shower because it’s cheap, effective, and environmentally friendly. But mostly cheap.
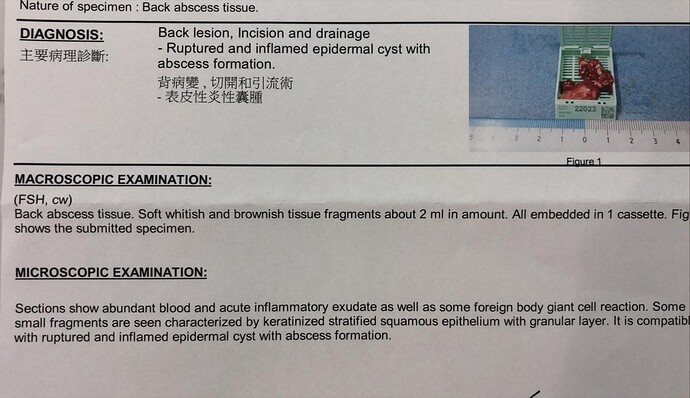
Did your doctor (dermatologist?) ever actually tell you that your epidermoid cyst was “infected”? Did he or she obtain a culture from the cyst contents and send it to a lab? Epidermoid cysts often rupture under the skin, becoming severely inflamed and painful due to inflammation, but are almost always a sterile inflammation that doesn’t require antibiotics, just incision/drainage for short-term relief and eventually excision if the cyst persists or recurs (which it usually does). Non-dermatology providers sometimes assume they’re infected because they “look” infected, and prescribe antibiotics unnecessarily. This is important because if this was just a typical ruptured epidermoid cyst and not an infection, then any connection to rapamycin would seem very unlikely.
The diagnosis was an infected sebaceous cyst. I could have had it excised and drained as I have had done twice in the past with other cysta. This time I went with antibiotics and it worked. The past two times it happened they excised it, drained it and then sent the sample to the lab that prescribed a treatment of antibiotics. It took a lot longer and was very painful. I much prefer antibiotics without excision.
This is a fairly common occurrence for me and happens about once every two years. I don’t blame the Rapamycin for it, but I felt I needed to stop it until I recovered.
And you are sure they sent the sample for a culture? If so, what baterium was it?
This was the previous one that they removed. Fairly deep hole. It took over a week to recover and I had to go to the clinic daily for wound cleaning and dressing. Trust me, antibiotics was much better. This is the lab report. If you know of ANY way to prevent these from forming, PLEASE let me know. This has been a curse on me ever since I turned 43. This was the last one before I started taking Rapamycin or any other supplements.
The wound became infected a few days after the removal and I had to take antibiotics and they added silver to the wound to kill the bacteria.
Interesting! Too bad they didn’t get a culture to see what kind of bacteria was the culprit. If your nose is colonized with MRSA, for instance, it can cause recurrent infections/abscesses, and you can get your nose treated with topical mupirocin to knock out the colonized bacteria. Might want to ask your dermatologist if he or she can do a quick nasal culture to rule this out since this has been a recurrent problem for you.
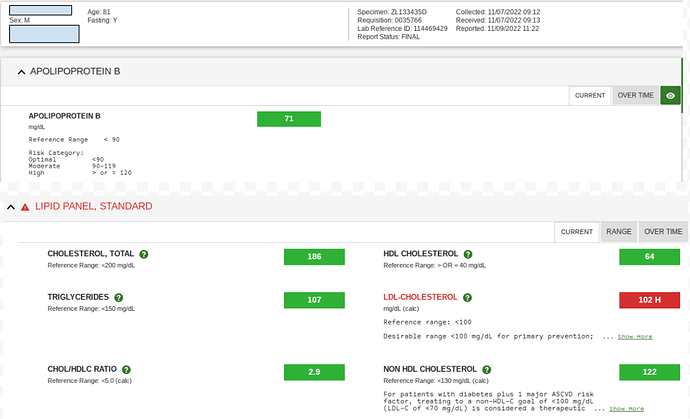
Finally honing in on what I feel to be my personal optimal rapamycin dosage. That being the amount I can take without adversely affecting my blood panels and epigenetic aging clocks.
These are my latest lab results. This is the first time I have had the APOLIPOPROTEIN B test included. I am quite happy with the results. I have been ramping down to my current 5mg rapamycin weekly with EVOO. I think I will continue this as a maintenance dose. Previously I have taken much higher doses with some negative side effects.