Indian generic Nexlizet is about $0.50 per pill and 5 mg Rosuvastatin is about $0.10 per pill, which comes out to about $18 per month if both are taken daily. The best price I see on Indiamart for one unit of PCSK9i Repatha is about $130 per month, which is quite a bit more. Is there another place you see it for much less?
Because a high ApoB/LPa ratio is bad. Unfortunately, even though I have a very low LpoA, and a good ApoB reading.
“The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy – a review of the evidence”
You can only lower that by reducing your ApoB. I don’t think you can do much about your LpoA number.
This still means my ApoB/LPa ratio is bad and I need to reduce my ApoB further.
IMO: Disregard changing your LPa and concentrate on lowering ApoB.
“Elevated lipoprotein(a) levels represent a genetically determined risk factor for myocardial infarction”
That doesn’t mean that you can’t keep your other risk factors low. BMI, ApoB, triglycerides etc., low.
Absolute risk is not that much higher for higher readings of LpoA
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2006.01643.x
Ok. In short: Lp(a) and Apo B (or LDL) are seen as independent risks factors.
If your Apo B is high even if your Lp(a) is low you still are at risks and should work on getting Apo B down and especially aggressively if your CAC is high
Same. In the Uk. Was told I don’t qualify for a PCSK9i until I have a cardiac event
In short, if you have high Lp(a), best strategy IMO is to aggressively lower ApoB and all other controllable CVD risk factors in order to offset the increased risk from Lp(a). New meds are on the horizon specifically for Lp(a), but who knows how much they’ll cost and who will qualify for them. PCSK9i can help lower it 20 or 30%, which is better than nothing but I’m doubtful it’s enough to make a big real-world difference.
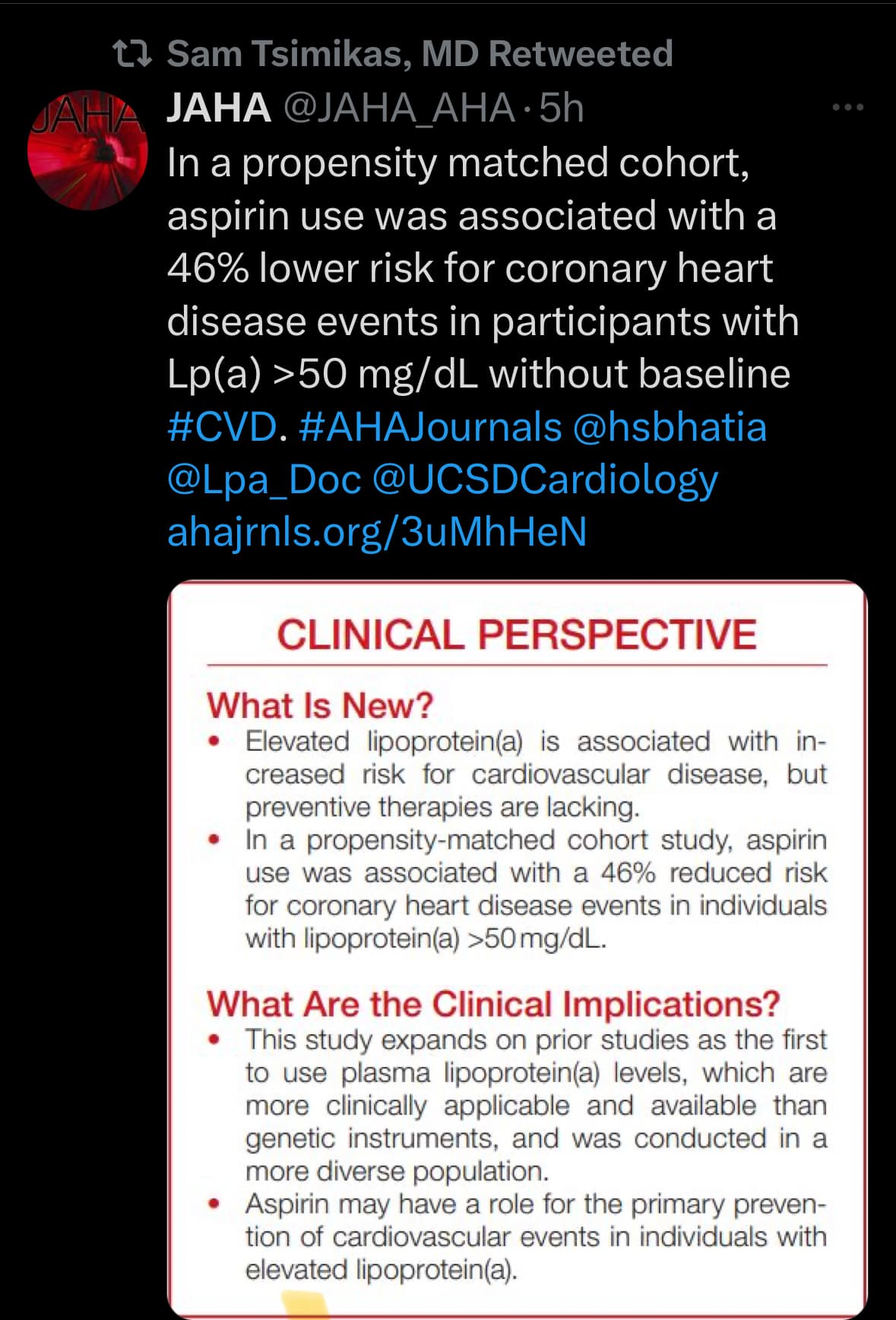
This might be worth considering for some of us.
Thank you for sharing this. This is great info for those of us with high LpA.
Also cross posting this and relevant to this thread:
Another study with same conclusion of aspirin being more helpful in higher Lp(a) patients
Some studies show Ezetimibe lowers Lp(a), (while other studies seems to have non significant (point estimates in right direction).
Does anyone have any experience of using Eze and leading Lp(a)?
A recent study supports the cholesterol absorption inhibitor ezetimibe’s ability to lower Lp(a), a finding that deserves further investigation as it has not been previously reported in multiple ezetimibe trials.
Do We Know When and How to Lower Lipoprotein(a)? - PubMed.
Overall pooled analysis suggested that ezetimibe 10 mg significantly reduced plasma Lp(a) concentrations in patients with primary hypercholesterolemia by - 7.06% (95% CI - 11.95 to - 2.18; p = 0.005) compared with placebo.
Therefore, we performed a systematic review and meta-analysis to assess this effect based on the available randomized controlled trials (RCTs).
Conclusions: Ezetimibe monotherapy (10 mg/day) showed a small (7.06%) but statistically significant reduction in the plasma levels of Lp(a) in patients with primary hypercholesterolemia. According to current literature, this magnitude of reduction seems to have no clinical relevance. However, further studies are warranted to clarify the mechanism mediating this effect of ezetimibe and to investigate its efficacy in combination with other drugs that have shown promise in lowering Lp(a) levels.
Effect of Ezetimibe Monotherapy on Plasma Lipoprotein(a) Concentrations in Patients with Primary Hypercholesterolemia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials - PubMed)%20compared%20with%20placebo.
Update:
Cross linking this - think it might be very relevant for anyone with non-optimal Lp(a) levels especially
Oxidized phospholipids in cardiovascular disease | Nature Reviews Cardiology
Abstract
Prolonged or excessive exposure to oxidized phospholipids (OxPLs) generates chronic inflammation. OxPLs are present in atherosclerotic lesions and can be detected in plasma on apolipoprotein B (apoB)-containing lipoproteins. When initially conceptualized, OxPL–apoB measurement in plasma was expected to reflect the concentration of minimally oxidized LDL, but, surprisingly, it correlated more strongly with plasma lipoprotein(a) (Lp(a)) levels. Indeed, experimental and clinical studies show that Lp(a) particles carry the largest fraction of OxPLs among apoB-containing lipoproteins. Plasma OxPL–apoB levels provide diagnostic information on the presence and extent of atherosclerosis and improve the prognostication of peripheral artery disease and first and recurrent myocardial infarction and stroke. The addition of OxPL–apoB measurements to traditional cardiovascular risk factors improves risk reclassification, particularly in patients in intermediate risk categories, for whom improving decision-making is most impactful. Moreover, plasma OxPL–apoB levels predict cardiovascular events with similar or greater accuracy than plasma Lp(a) levels, probably because this measurement reflects both the genetics of elevated Lp(a) levels and the generalized or localized oxidation that modifies apoB-containing lipoproteins and leads to inflammation. Plasma OxPL–apoB levels are reduced by Lp(a)-lowering therapy with antisense oligonucleotides and by lipoprotein apheresis, niacin therapy and bariatric surgery. In this Review, we discuss the role of role OxPLs in the pathophysiology of atherosclerosis and Lp(a) atherogenicity, and the use of OxPL–apoB measurement for improving prognosis, risk reclassification and therapeutic interventions.
Key points
- Phosphocholine-containing oxidized phospholipids (OxPLs) induce chronic inflammation, including in atherosclerotic lesions, and can be detected in plasma on apolipoprotein B-100 (apoB-100)-containing lipoproteins.
- A method has been developed to quantify OxPLs on a normalized amount of apoB-100 (OxPL–apoB), so that the measurement is independent of plasma apoB-100 and LDL cholesterol levels.
- Lipoprotein(a) (Lp(a)) particles carry the largest fraction of OxPLs among apoB-containing lipoproteins; the OxPLs are bound covalently to apolipoprotein(a) and are free in the lipid phase of the associated LDL-like particle.
- Plasma OxPL–apoB levels predict the presence and extent of anatomical atherosclerotic cardiovascular disease, and elevated levels are associated with disease in multiple arterial beds; measurement of OxPL–apoB improves prognostication of peripheral artery disease, as well as incident and recurrent myocardial infarction and stroke, and improves risk reclassification, particularly in patients in intermediate risk categories, for whom improving decision-making is most impactful.
- Plasma OxPL–apoB levels are reduced by treatment with antisense oligonucleotides aimed at reducing Lp(a) production and by lipoprotein apheresis, niacin therapy and bariatric surgery.
- Plasma OxPL–apoB levels predict cardiovascular events with a potency similar to or greater than that of plasma Lp(a) levels, probably because OxPL–apoB levels reflect the levels of the most atherogenic and pro-inflammatory Lp(a) and apoB-100-containing particles.
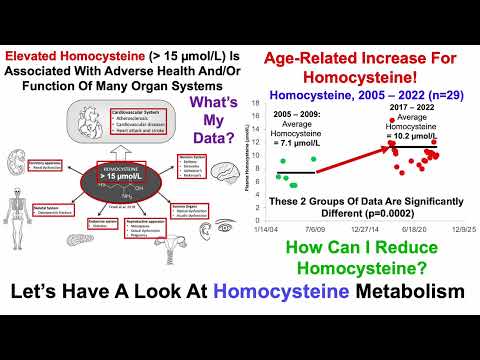
I lowered my LP(a) with 43% in 3 months by using 400mg bezafibrate, but it also increased my homocysteine levels.
Thx. Do you know if his glycine experiment ended up workin?
Did that 6 months ago, by daily glycine / creatine / TMG and methyl folate I got a 30% reduction, so I continued using these. Then 3 months ago, I did a 3 month bezafibrate test and now I was back where I started.
Did you get it through a doctor or IndiaMart or another source? I don’t see it on IndiaMart. My Lp(a) is at 100…
Found that from the vid below. Dr. Bosworth discusses the blogpost in the vid. But I prefer reading than listening.
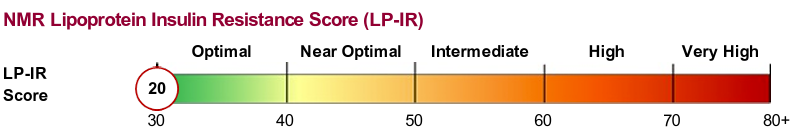
| Risk Factor, | Age of Onset < 55 Years | Age of Onset 65 – 75 Years |
|---|---|---|
| per SD Increment | Adjusted Hazard Ratio | Adjusted Hazard Ratio |
| Insulin Resistance, LPIR Score | 6.4 | 2.09 |
| Systolic Blood Pressure | 2.24 | 1.48 |
| Triglycerides | 2.14 | 1.61 |
| Apolipoprotein B (ApoB) | 1.89 | 1.52 |
| C-Reactive Protein (CRP) | 1.76 | 1.62 |
| Non-HDL Cholesterol | 1.67 | 1.41 |
| Body Mass Index (BMI) | 1.47 | 1.33 |
| LDL Cholesterol | 1.38 | 1.24 |
| Hemoglobin A1c | 1.38 | 1.24 |
| Lipoprotein(a) | 1.22 | 1.11 |
I am merely sharing what I found. I am not an advocate of the theory. I do not want to get into an argument with posters who have their pet theories about CVD risk.
Read or ignore. The prerogative is yours.
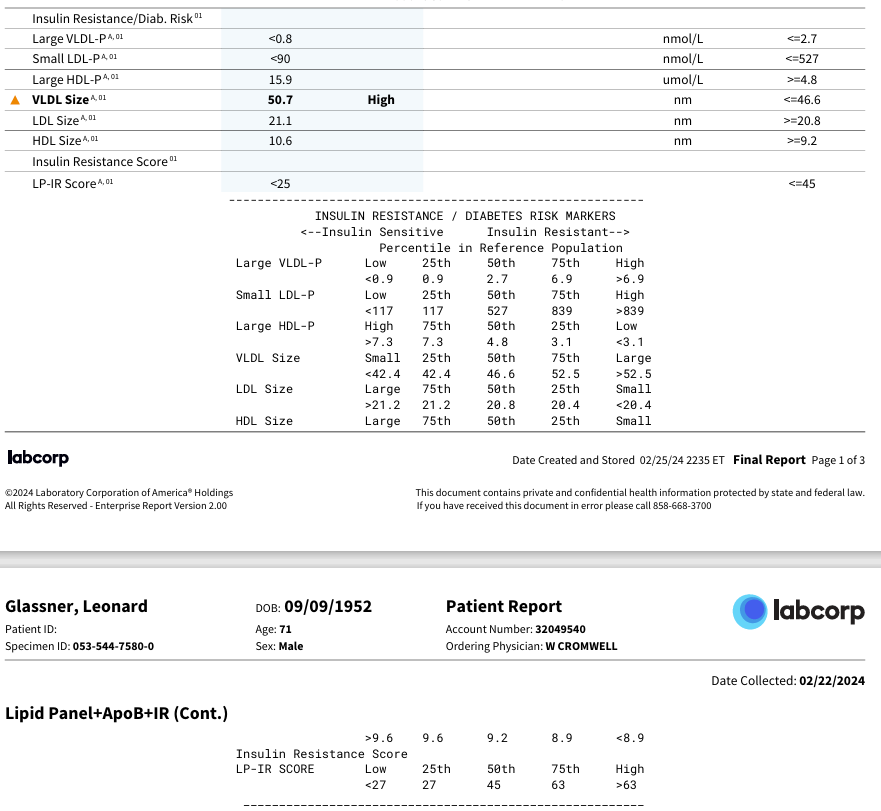
LP-IR
Results from my labcorp test a few weeks ago:
Seems pretty encouraging.
(Note that the one thing flagged ‘high’ means it was above the 50th percentile, not outside the range.)
And yet - I have CVD. Have had since at least 2016, likely started years before.
I did start a statin four months before this test, but per the Dr. Forey:
‘Importantly, the LPIR Score remains relevant even among individuals prescribed statin therapy.8 Specifically, statins have a relatively small effect on the lipoprotein parameters that are heavily weighted in the LP-IR algorithm.5’
I get everything from a pharmacy in Belgium / Europe where I live. Now I am testing daily 145 mg fenofibrate nanoparticles to see what this drug gives after 3 months on LP(a) and homocysteine.
I do think there is some degree of arbitrariness in who gets the PCSK9i and who is denied. I was told at first to take the statin but pushed back because the statin can raise Lp(a). Then I had a CAC done and it came back 0.91 – very low but not zero, so some evidence of CVD (bit of calcium on the LAD). I requested – dare I say – entreated – my cardiologist once more and this time I was able to get the PCSK9i. The process is frustrating. Might add- – Pelacarsen is being trialed right in my university medical complex. It is sitting in cupboards right where I am being seen. But it will be years before I might be able to get it. Tom Dayspring seems to indicate at least five years or so, by the time it completes trial, gets through FDA, and then only for “nightmare cases” (his words) and finally to those who are high risk but not off the charts.