Still, searching for that sweet spot. I have been doing 1 mg/day for 7 days and 7 days off.
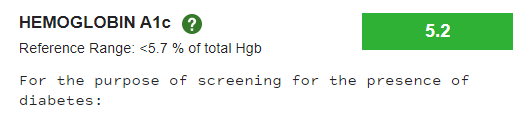
I am still having trouble keeping my glucose below the high normal range.
Currently, I am taking 500 mg of metformin with rapamycin, a 50 mg acarbose tablets
before dinner. Also, I just added Linagliptin 5mg tablets four days ago morning and evening. “Linagliptin helps to control blood sugar levels by increasing substances in the body that make the pancreas release more insulin.” It is also sometimes combined with metformin in a single pill. So, far I have seen zero effect. Maybe it is still too soon to tell or I need to increase the dose. I have tried Jardiance Empagliflozin, also to no noticeable effect. Perhaps it is just because I am old.
The only insulin-sensitizing drugs that I can find have serious side effects and most of them have been banned in some countries.
So, my next plan is to reduce my rapamycin intake to 1 mg/day for 5 days then 9 days off.
I prefer to try this rather than increase my anti-diabetic drug intake.
As I have commented before: I don’t believe it is okay to have markers outside of the normal range even if you are taking rapamycin. Specifically, I believe that blood glucose should not be above normal. Glycation, from my readings, appears to be one of the most important things to reduce to prolong life span"
"Glycation, a deleterious form of post-translational modification of macromolecules has been linked to diseases such as diabetes, cataract, Alzheimer’s, dialysis related amyloidosis (DRA), atherosclerosis and Parkinson’s as well as physiological aging
“Hyperglycemia increases the glycation process, and is especially apparent in insulin independent tissues such as red blood cells, peripheral nerve tissue cells, endothelial cells, eye lens cells, and kidney cells”
“There is evidence to indicate that controlling hyperglycemia by antidiabetic biguanides prolongs life span in experimental animals. Caloric restriction, which appears to prolong life span by bringing about mild hypoglycemia and increased insulin sensitivity further strengthens the idea that glucose via glycation is the primary damaging molecule.”