Mouthwash can never replace mechanical cleaning and if you clean properly you do not need mouthwash
I’ve been chewing Spry gum which is sweetened with xylitol. I don’t like to chew, but it works muscles and is supposed to be good for you. Probably end up swallowing the pathogenic bacteria. So I start every day with a small piece of aged cheddar which is supposed to have enough spermidine to close all the loose junctions in the gut.
I would love for Arhu to weigh in on my post in the side-effects thread: Side Effects of Rapamycin (part 2) - #180 by CTStan
Peach kernel safflower is high in luteolin. I love fruit–it’s pretty much the only carb I eat–but try to always take some luteolin with it when I eat it.
I don’t know if this will make you feel better or not, but he’s fun to read anyway.
The article on statins is well done because it looks at the two factors that matter most. Absolute risk reduction and total mortality rates. In those most important factors statins mostly strike out. The sole exception being males under 65 with a history of heart attack. Most rapamycin users don’t fall into that category.
Blagosklonny posted a study today from 2013 which supports the notion that the metabolic effects of short term rapamycin are in direct contrast to the long term effects.
This was also seen in marmosets where lipid dysregulation was transient.
In this study we see in mice that the adverse insulin resistance at the beginning of treatment switches to the preferred insulin sensitivity over time. The same was seen with lipids.
Maybe patience is all that’s required after all.
Isn’t 20 weeks a long time for a mouse? If it dies in 100 weeks that’s 20% of its lifespan. I’m not sure I want to wait that long for things to normalize!
Fair point. I’m not certain that the translation from mice to humans actually works that way, but it might. The encouraging thing is that a similar transient metabolic effect was also seen in marmosets.
Also, according to the posted study, they make the claim that the “ metabolic switch “ from the unfavorable to the favorable occurs in renal transplant patients as well.
Perhaps I have been doing myself no favors by taking a washout period.
Do you think a steady dose and not doing periodic washout periods might be the better strategy to normalize our lab panels while on rapamycin?
It’s really hard to know and I debate this with myself frequently. I also don’t think that anyone really knows the answer to it.
So right now I’m straddling the fence, keeping my rapamycin dose reasonably low on a weekly basis while incorporating in flax and taurine to keep the lipids at bay.
As I’ve stated before, metformin messes with my exercise, so I’m seriously considering berberine for insulin sensitivity. I realize that it works via a similar AMPK mechanism but I’ll see how my stamina responds.
In the meantime, I do think that the metabolic effects will sort themselves out over the long run. I’m very skeptical that any drug could consistently give significant longevity while inducing long term metabolic dysfunction.
So I’m optimistic, but cautiously so.
Resveratrol reduces total cholesterol, triglycerides and LDL-C levels.
For those having cholesterol trouble, you may want to consider taking Resveratrol.
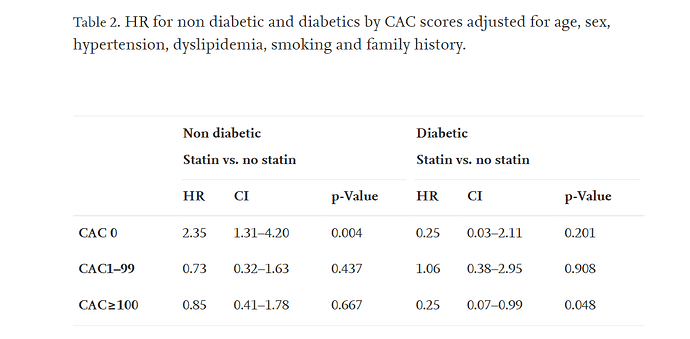
Statins did not reduce major cardiovascular events in non diabetics even in those with a baseline high atherosclerotic burden.
In those with CAC of zero, statins may actually increase risk.
I have read many studies similar to this and I am now going back to a lower dose, 5mg/week of rapamycin with EVOO. This time I will not be taking any “washout” periods.
This will give rapamycin a chance to revert lipids to normal.
I will have blood work done every two months to track lipid changes. My diet is pretty regular except for the holiday season when I will be eating out more and having dinners with friends and relatives. If my lipids stabilize, I will keep doing the 5 mg/weekly with EVOO, which translates roughly to 7.5 mg/week.
I interpret recent articles to suggest that there is a u-shaped dosage curve with the sweet spot being roughly 5 - 10 mg/weekly for humans
Yeah, I think we’re on the same page.
You think that the EVOO makes the 5 mg the equivalent of 7.5 mg’s? That much of an impact?
I do believe that I read that a fatty meal enhances the absorption of rapamycin by about 30% - 50%. I take rapamycin with a shot of EVOO along with a high-fat meal. Maybe I am wrong, I just want to be somewhere between 5 and 8mg
Some pretty strong arguments here for checking ox- LDL over merely LDL levels. LDL seems to be less and less relevant as a stand alone marker.
Isn’t this contradicting a rather substantial body of evidence showing utility of statins for primary prevention both in DM and non-DM patients with sufficient risk factors (including subclinical CAD)? I do wonder if this study was simply underpowered to detect reduction in events over 5 years in the CAC <100 groups. There simply aren’t a lot of events happening in a patient population with extremely mild coronary disease… and that is evidenced by the unimpressive CIs and p-values.
From the abstract, even the positive findings look like borderline trash:
For DM patients, baseline statin therapy significantly reduced MACE for patients with CAC ≥100 (HR: 0.24; 95 % CI 0.07–0.87; p = 0.03) and SIS≥3 (HR: 0.23; 95 % CI 0.06–0.83; p = 0.024) compared to those not on statin therapy
This one study with barely-significant findings indicating that statins may not be that useful is not going to stand a chance against the meta-analyses showing very clearly that statins do their job well. If you have a CAC of 0, yes, maybe you should consider not going on a statin, but I don’t think that’s a controversial opinion.
Edit:
Managed to get access to the full paper. I’m sorry, but this is just screaming “underpowered” to me.
It’s interesting to me that they even acknowledge in the following quote that diabetes itself – a massive risk factor for CVD – essentially takes more than 5 years to become statistically detectable in its ability to cause events:
“Valenti et al[10] examined the long term prognostic value of CAC in a single center study in patients with diabetes, and found that for first 5 years CAC- 0 was associated with similar mortality risk in those with and without diabetes. However, beyond 5 years mortality risk was higher in patients with diabetes. In Walter Reed cohort of 928 individuals with diabetes, statin therapy was not associated with significant reduction in ASCVD events in patients with CAC-0, however those with CAC > 0 had significantly lesser events over 9-year follow-up.[10]”
If diabetes has a hard time making itself known within 5 years in terms of contributing to events, then it’s unsurprising that treating a group of barely-diseased patients with a statin for 5 years isn’t going to lead to an impressive reduction in events unless you’re ready to have an MI at the drop of a hat. Atherosclerosis prevention is a marathon, not a 5k. If you’re going to make the claims this paper is trying to make, you need way more patients (and events) if you’re going to change how we think about statins.
The argument is whether an increase in LDL from rapamycin warrants an aggressive intervention with medications such as a statin drug. This would assume that LDL would override any protective mechanism that may occur with rapamycin.
I’m arguing that the evidence doesn’t support such an intervention and that the benefit/ risk ratio doesn’t work.
The evidence from statins related to their cholesterol lowering effects isn’t clear because of the pleiotropic nature of statins. They’re anti inflammatory as well as anti thrombotic.
Agreed that aggressive intervention is probably unwarranted, although a low-intensity statin (pravastatin 20mg, or even 10mg/d) still seems like a reasonable idea given that most people in this community are interested in living long enough such that atherosclerotic disease is nearly inevitable. The mendelian randomization studies – as well as subsequent research showing cumulative apo-B/LDL exposure as an important risk factor – suggest to me that optimizing lifetime exposure is probably a good idea.
Hydrophilic statins like pravastatin have also not been shown to contribute to diabetes risk, nor are they associated with adverse cognitive findings. While I completely agree with you that throwing 80mg of atorvastatin at someone on rapa is unwarranted, low-risk, low-dose treatment with something like pravastatin 20mg +/- ezetimibe is a fine decision for someone trying to optimize long-term risk of cardiovascular disease.