would taking baby aspirin help clotting as a daily regimen in addition to statin?
For the premium members of Peter Attia, there is now a 14 minute article on statins:
Atherosclerotic cardiovascular disease (ASCVD) is one of the few chronic diseases for which we have a clear, causative factor that can be targeted therapeutically to reduce long-term risk. The strength of evidence from genetic, randomized, and observational data all points in the same direction: ASCVD is caused by circulating, cholesterol-carrying, apolipoprotein B (apoB)-containing lipoprotein particles, which above certain threshold concentrations have the ability to leave plasma, pass through the arterial endothelial lining and enter the underlying intima layer, where atherogenesis occurs. Reducing apoB particle numbers can thus drastically slow disease progression. Of the various pharmacological treatments now available for reducing circulating apoB particles, one of the earliest classes of drugs to be developed remains one of the most effective (and affordable) options – statins.
$19 / monthly.
This is a super long thread.
A couple of questions, as I am currently just starting Rapamycin.
-
I have slightly high LDL and am currently in the process of trying out regimens to reduce it. Should I first do this before starting rapa, in order not to falsify the results? One step after the other?
-
What is the consensus now: Is the dylipidemia an issue now or not? Should I also try to get LDL back down to ideal levels with heightened LDL due to Rapa? Or do we more or less ignore it because it is due to rapa?
-
How to manage LDL over time? If Rapa dysregulates lipids, how do I measure them and get proper feedback for blood tests? Do I stop rapa for a few weeks before blood tests? For how long?
Controlling your lipids is more important than using rapamycin.
Now, yes.
Yes, always.
No, it doesn’t matter where it’s form.
With pharmaceutical drugs and lifestyle. A low saturated fat diet, and high in mono- and polyunsaturated fat. Statins, PCSK9 inhibitors, Ezetimibe, etc.
You should measure ApoB. If you cannot measure that, you can do LDL or non-HDL-c.
That doesn’t matter as you want to know your lipids on the drug too if you’re going to take it.
If I need to get it to ideal levels either way, why try to do that now before starting Rapamycin only to then adjust the measures again after dyslipidemia due to Rapa?
Indeed - I rather meant: How to handle it if its additionally increased due to Rapa. But that question is superfluous if I need to get LDL down to ideal levels regardless of additional increases due to Rapa or baseline without rapa.
Indeed. Its on my list for the next test. So far only LDL and Lp(a). In this instance I first tried “soft” interventions like Psyllum husk and reduced fat intake, red rice, after which I might try statins with the doc.
Thanks a lot. So in my book there is not need to stop Rapa and first sort out LDL/ApoB, instead I can continue Rapa and sort it out nonetheless asap.
Mind you, I’m in my thirties, low Lp(a) and the LDL is 160 w/o intervention or rapa. My doc says its nothing to worry about, but if I read the literature it seems there is no reason not to lower it nonetheless. But I indeed need an ApoB test, too. Step by step.
Imo why not start rapa+rosuva+zetia all at once then check your lipids a couple months later? If LDL-C is above 70 (50), maybe increase your statin dose, if it’s below 70 (50) you don’t need to change anything. The only other value I’d look out for is HbA1c as both rapamycin and statins can increase your blood sugar.
The consensus is, I think, we don’t know whether rapamycin-driven lipid disregulation is a significant issue, but given that (in my view) the preponderance of data suggests that lipid dis regulation is not a good thing, so getting that under control is important.
the increase in lipids doesn’t seem to happen to everyone, or even a majority of people, but it seems dose dependent (the higher the dose, the more frequent the dosing, the more likely it is).
I’ve always had high cholesterol, no matter what my diet. It went higher by about 20% with rapamycin, and I’m working to get my APOB number down to where I want it. I’m managing both rapamycin and lipids together and trying to work out a combination of approaches that works for me.
I had low LDL (86) before Rapamycin and higher LDL (122) after Rapamycin. I do take a fairly high dose each week (9 mg equivalent). I am trying a very high once-per-month protocol to see how that goes. I’ll report my numbers in early 2024.
I’d use a statin and ezetimibe in your case (Maybe try Rosuvastatin + Zetia). Statins didn’t work for me, but maybe they will for you?
@johano in my case my LDL-C (and TC) on rapamycin (6mg/week) improved, it dropped approximately 15% in course of 6 months.
I believe there is much more you can do for your health with lifestyle interventions that are proven to extend healthspan and lifespan and will undoubtedly improve your metabolic health as well. Loosing additional weight, keeping your belly fat to minimum, your BMI in check, practicing moderate dietary (caloric) restriction (I personally do around 10%), avoid saturated fats, restrict meat consumption, eating high fiber diet, avoiding sugar, dietary omega 3 sources, daily exercise, no smoking, limiting alcohol intake, taking care of stress, psychological wellbeing etc.
I don’t believe any pill (rapamycin included) could be a replacement for healthy habits. And for your ASCVD health it is crucial that you address your metabolic health before age of 50. Cumulative burden up to middle age is far the most predictive of ASCVD.
It is crucial that you try to keep your LDL-C in the 50-70 mg/dl (or better apoB in that range), your blood pressure below 120/80, your fasting glucose below 85 mg/dl and CRP below 0,7 mg/L if you want to live long.
There isn’t any evidence to the contrary, that it isn’t a significant issue, with the same standard of evidence behind lipid disregulation. There will never be such evidence either for a long time, and it isn’t hidden somewhere to be found right now. What we have is the best we will ever get for a long time and based on current information means that it is not good at all. At the same time I’m not going to make people believe in it, they can look at the evidence themselves. If they’re going to believe animal model studies will be applicable to them, or speculate based on mechanisms, without understanding the limitations of that and how it compares to clinical trials and genetic studies, that is on them and their lack of knowledge, education, about science in general. Often it is the case that they have this knowledge, yet choose to see past it because of ideological reasons, or motivated reasoning.
There is no consensus on LDL-C which is a weakly correlated indicator and is not even measured but estimated. (see below)
This means that on average more LDL-C is bad but that does not mean it is bad for any particular individual. If you want to know if you are at risk get an NMR lipid panel and you will have a much better assessment. There are some people who have an extremely high LDL-C but a low CVD risk and obviously others who have a very high risk.
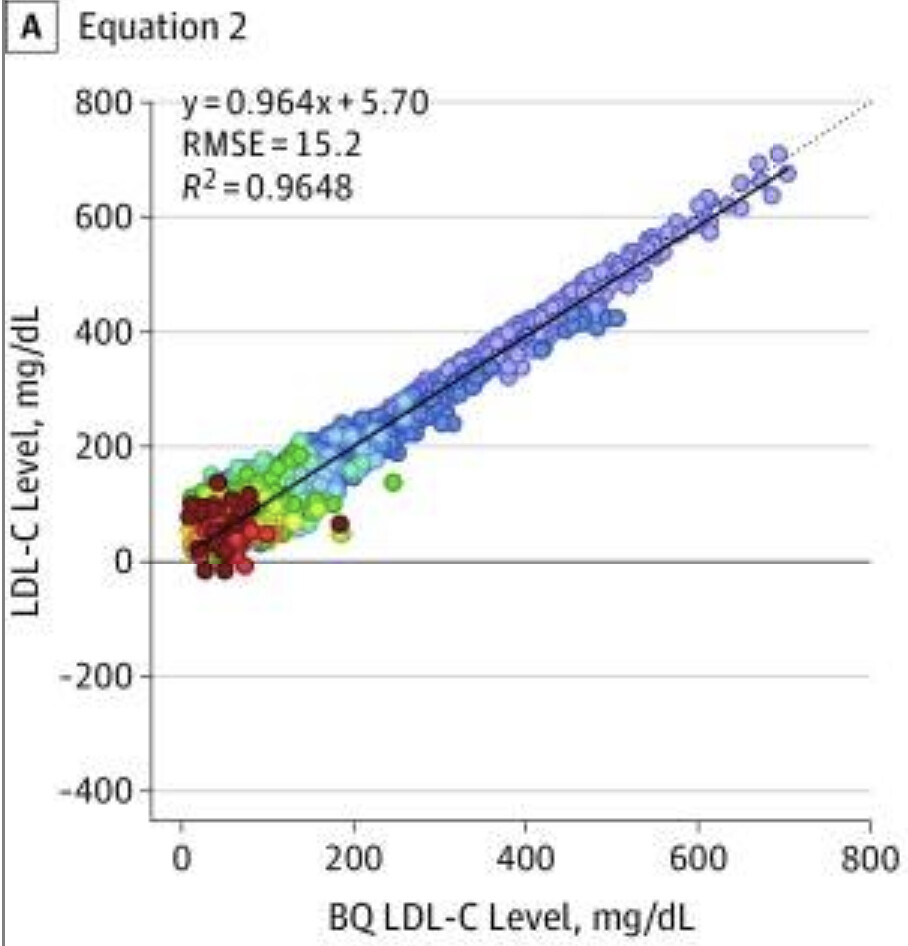
To go back to the LDL-C estimation which is what you get with a non NMR lipid panel here is the latest NIH equation used by the standard lipid panels:
LDL-C = TC/0.948 – HDL-C/0.971 – (TG/8.56 + [TG x NonHDL-C]/2140 – TG2/16100) – 9.44
Basically they measure TG, HDL and the NonHDL and use them to get an estimation of the LDL-C.
I do find it pretty amusing that the indicator the most used for the treatment decisions is the only one not measured.
Let’s see how well it works:
From A New Equation for Calculation of Low-Density Lipoprotein Cholesterol in Patients With Normolipidemia and/or Hypertriglyceridemia
As you can see, the higher the LDL the better the approximation which is why you get a R^2 of 0.96 which is a very nice correlation.
Now, as most people here are probably not much higher than 200, only look at the 0-200 portion of that graph and clearly the correlation is much lower and the data points distribution is very scattered. There are even points which are negative! Others are overestimated by 100+.
BTW those estimations are derived from a population who is mainly unhealthy on average which makes it even less likely to fit the people in that forum.
Obviously taking any medication with side effects based on that simple LDL estimation does not look optimal to me. If you are in the +100 category you are going to be told to take statins while you should not and inversely if you are in the -100 category you will think you are fine while you might not.
That’s why I highly encourage people interested in their lipids to take an NMR lipid panel.
This low carb conference just ended and they have different science:
Low carb diets cause High LDL, but it isn’t bad for you.
LDL-C can be calculated or measured directly.
In my lipid panels I took and could find in it is always indicated as “direct LDL-C” which is not calculated but measured.
I’m curious about the cholesterol “defense against pathogens” argument mentioned by Diamond in the low carb video. Does anyone know where that argument comes from? I’ve heard it before from the low carb crowd. I am generally biased against the arm waving low carb stuff since I used to be swayed by it some years ago but I don’t want to miss something useful if it is real.
Lustgarten has references to studies in his book. I got the ebook free, read it about 4 times, then lost it. I’m not great at the tech stuff. Think I’ll buy a paper copy.
Seems like it cleans up the LPS, which are the broken up pieces of the bacteria left over after the LL37 kills them. The LL37 just hangs out in your bloodstream like sandburs in the pasture. It increases with increasing vitamin D. This lowers your microbial burden, but LPS is the cause of T2D, so it needs to be removed.
LL37 is an AMP (anti microbial peptide). It has a Lysine and Leucine on the end and is 37 amino acids long.
Thanks. Here is some background info on LPS which is also called Endotoxin. The primary route into the body is thought to be inflection and leaky gut. These documents do not reference any mechanism of cholesterol removing LPS. I’ll keep looking.
https://www.sciencedirect.com/topics/chemistry/endotoxin#:~:text=Endotoxins%2C%20also%20called%20LPS%2C%20are,cell%20lysis)%20%5B231%5D.
They have “different science,” all right ![]() .
.
One PhD psychologist (and Dave Feldman, Ravnskov (sp?), and other fringe characters) vs. the European Atherosclerosis Society, American Heart Association, and American College of Cardiology.
I’m guessing this is a leap to mechanistic conclusions from the evidence that APOE4 (which was the original primate APOE and raises circulating LDL-C) seems to be protective against some pathogens and the fact that LDL-C falls during sepsis to the conclusion that LDL-C itself is protective when just walking around.
That’s a huge leap of logic. During sepsis one tends to lie on their bed a lot instead of sitting at their disk, so is sitting good for your immune system? ![]()