I mean that you have to stay on the med forever or the weight invariably returns as do the associated co- morbidities.
Piloting a Remission Strategy in Type 2 Diabetes: Results of a Randomized Controlled Trial
- personalized exercise routines
- strict diets
- glucose-controlling drugs
Four months after the intervention, 40 percent of the subjects were able to stop taking their medications and remained in partial or complete remission.
Tangentially related:
How’s insurance coverage for privately-insured patients? Is step therapy still usually required, or just BMI>30 = good to go? Any issues with supply/availability of the drug itself?
Insurance is difficult and usually not covered. They still claim that weight loss is cosmetic!
You have to start dosing low and titrate up . Takes a couple months to really kick in.
Cost at pharmacies is about $1500 per month.
One thing that I noticed right away with rapamycin was a 10% drop in my neutrophils. This is probably ,at least in part ,due to its anti inflammatory effects. A low neutrophil count has been found to be cardiovascular protective in several studies.
It’s never easy. No matter what the subject I can find opposing “expert/study” opinions
“As stated in our paper, it is important to understand that our results are based on observational analyses. Thus, they say nothing about the causal role of LDL cholesterol in the development of cardiovascular diseases or mortality, and our results cannot be used to assess the potential effect of LDL cholesterol lowering therapies.”
https://www.bmj.com/content/371/bmj.m4266/rr-4
"
Gil Carvalho MD PhD
@NutritionMadeS3
·9h
this means lowering cholesterol itself is not the problem. the problem is cholesterol dropping spontaneously, in the absence of drug treatment or lifestyle change (i.e. due to underlying progressive disease)
“landmark analysis: the longer we hold LDL-cholesterol down the stronger the benefit”
Interesting thread here:
https://twitter.com/NutritionMadeS3
Here’s what’s confusing. Let’s say you have a group of people with a normal LDL range and they get cancer. The disease “ eats up “ their LDL and it spontaneously drops to some very low level. This group would now have a high mortality rate from the cancer and the lipid was just an unrelated association. But now we should see increasing mortality rates as the LDL’s increase, but that’s not what we saw in the Japanese study.
For each incremental increase in LDL we see Lower mortality rates . This should not be happening if LDL is giving them heart attacks and strokes. I mean are we actually to say that the highest LDL group just doesn’t have any illnesses pushing down their values?
Well it’s hard to pinpoint because after I got the first results and was put on a low dose statin I also changed my diet and supplementation protocol but I would say the Crestor got it down about 50% to where I am now but I will say that the LDL going down to 30 was after I was on Rapa for almost a year with no other real changes in my protocols so not scientific but an interesting N=1.
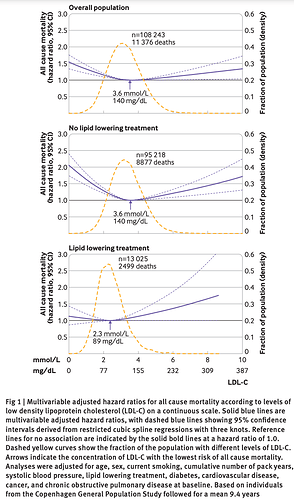
In the general population, there is generally a U-shaped curve to LDL and mortality, the Danish study re-posted here.
If you look at the x axis, or LDL-C, it captures very high LDL-C values (200 mg/dL++)
In the Japanese study, one of the major limitations:
“The threshold for the high LDL-C group may have been too low to evaluate the U-shaped relationship between LDL-C levels and all-cause mortality”
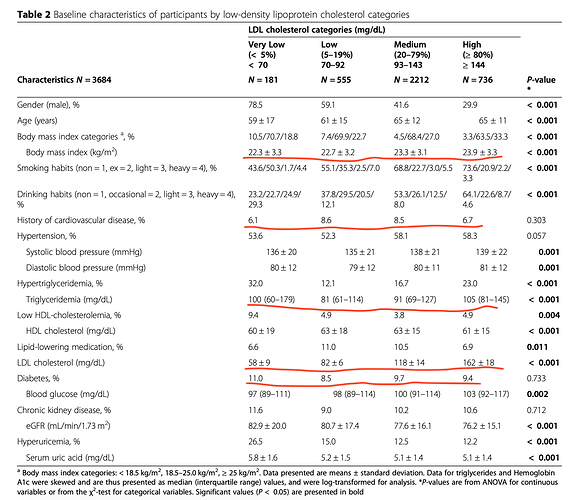
If you look at Table 2, herein, the average LDL of the “high” quartile was 162 +/- 18. That’s not much above 140 in the above Danish study.
Also, the “high” LDL-C Japan study cohort dosen’t seem too unhealthy, if history of CVD, BMI, diabetes, TG and TG/HDL are proxies for CVD (which they are). The high quartile LDL-C group absolute values for these parameters are relatively good.
As for explanations for higher LDL-C and lower all cause mortality (from the Japanese study).
“Ravnskov et al. [27] reviewed nine cohort studies involving more than 140,000 individuals. The review showed that the occurrence of cancer was inversely associated with cholesterol levels measured 10–30 years earlier, and the association remained when cancer cases that appeared during the first 4 years were excluded. Moreover, the lowering of lipids in rodents have led to cancer in previous experiments [25]. In addition, exotoxins produced by Gram-positive bacteria are absorbed by LDL-C [31]. Thus, higher LDL-C levels have been associated with reduced infection-related mortality and other nonCVD mortality, which explains the inverse relationship with all-cause mortality [28].”
So the going explanation for higher mortality in the very low LDL group is that they have some serious illness driving down the LDL. But you would expect weight loss in that group but instead they’re at a very healthy 22.3 BMI. Normal.
I’ve seen before some studies showing that LDL protects against pathogens.
It’s confusing but it’s never just cardiovascular mortality that’s important, it’s total mortality.
One very significant issue with all medical studies is the use of relative rather than absolute risk in their results and conclusions.
Here’s a look at absolute risk reduction using statins for lipid reduction on cardiovascular outcomes and the risk reduction is modest at best.
“The studies were all partially or wholly funded by the pharmaceutical industry.”
This is one of the main reasons to question many studies.
Yeah. That’s for sure
Peter Attia gave a good rebuttal to this analysis. One of the main points is that the average study duration was short (4.4 years) for a disease that accumulates over a lifetime (starting in the teens). It takes a long time to reverse it, such that the effects of statins are much stronger over longer periods of time.
Seems like he rather casually dismisses the work of multiple researchers from 4 separate countries evaluating 21 studies and published in 2 major peer reviewed medical journals.
His reasoning is also based on published research and explains why the meta-analyses can be “true” but also interpreted incorrectly. The time factor and the Mendelian randomization studies are especially convincing IMO. This framework also leaves plenty of room for non-statin methods of lowering ApoB and for inflammation as a causal factor and a legitimate target in CVD.
I think it’s fair to say that we agree that chronic inflammation is an important underlying cause of most, if not all, age- related diseases.
Where we seem to disagree is the importance of lipids in the management of primary prevention of cardiovascular disease. You view them as an independent risk worthy of drug intervention whereas I see them more in the context of other risk factors and therefore not necessarily requiring meds.
We may both be right depending on the situation.
Perhaps of interest on this topic:
And more evidence for an HDL sweet spot.
Amazing how we’ve been studying lipids for over 40 years yet we continue to be surprised. For many years we preached the higher the better with HDL. Nothing in science is ground in stone, it’s only good until the next study.