This clip is from podcast # 235
Interesting discussion with Peter Atia with Layne Norton, Ph.D. especially the independent risk factor of LDL.
@ 5:44 Layne Norton: “We still have LDL denialists out there”, Peter Attia: “I think it is one of the most dangerous things I see actually.”
That’s an overly simplistic view and ignores the evidence of multiple studies as being essentially irrelevant.
Here’s a new 10 year study just published looking at lipids and CVD. It emphasizes the complex nature of this topic and it’s anything but settled and simple.
“ However, evidence supporting the causal link between TC, LDL and CVD remains controversial, and recent data reveals that CVD risk cannot be merely explained by TC and LDL levels, that LDL might even be Beneficial in terms of overall lifespan and that treatment with statins is of doubtful benefit in regard to primary CVD prevention.”
In this study HDL and Triglycerides were found to be the highest predictors, but it varied significantly by subtype.
The lipid/ CVD story is complicated and is still being written. Anyone suggesting otherwise is being overly simplistic.
Because they are lower in the evidence hiearchy. Don’t you use this heuristic too? Life is too short to be considering all the evidence, especially the weaker types (lower on the hierarchy).
Actually, for many people, life is too short for them to have an open mind and consider thoughtfully any study that conflicts with their pre- established viewpoint.
Life is complicated and paradoxical.
So finally we know why rapamycin moves some markers in the wrong direction, it’s because it’s actually doing its job and autophagy is kicking in
In essence one of the issues with markers. Sometimes you can only make progress by having the side effect of one or more markers going the wrong way. A strong argument for cycling really.
I think it tells us markers are just markers and we shouldn’t try and fix them but the underlying problem instead.
That is generally true - but there are some real problems with the classic evidence pyramid thinking.
I would emphasize that “lower-quality” evidence such as meticulously done N-of-1 crossover trials & Mendelian randomization can be very useful if carefully interpreted with a lot of contextual knowledge, while “high-quality” evidence can be useless or harmful.
Here’s an example:
Ivermectin in a meta-analysis was shown to be effective for COVID-19 treatment. This was later shown to be based on fraudulent data.
As for the case of LDL-P/apoB, my current opinion is LDL-P<1000 and LDL 70-90 (if not discordant) would be a reasonable treatment target for a lipidologist to consider, particularly if there are risk-enhancing factors, medication side effects are very carefully considered, and if it cannot be done through lifestyle alone.
Let’s say we compare LDL 55 vs LDL 70-90, assuming no discordance. What is the purported difference in absolute risk reduction on all-cause mortality over a few decades (let’s say 20-30 years) if your position happens to be correct? That should be more informative.
I suspect the difference would be clinically insignificant in a “healthy” individual with no risk factors (maybe a theoretical 1% or less absolute risk reduction) - while waiting for more information over the next 20 years is probably a better option.
That being said, many people will have varying opinions on this. My general rule is to cut my confidence level in half after a lot of research on any purported benefit (expert opinions alone can and very often are incorrect) - unless there are very, very good reasons and I fully understand the subject at hand. We can size a position based on confidence level of the benefits vs harms accordingly.
In randomized controlled trials, lowering from 70 mg/dl median LDL-c show a reduction in events, both in statins and PCSK9, with no observed adverse effects. With a relative risk reduction equal to when the starting LDL-c was twice as high.
Because LDL-C–lowering therapies tend to produce the same relative percentage lowering of LDL-C regardless of starting levels, the absolute lowering of LDL-C and therefore the relative and absolute risk reductions will mathematically be a function of the baseline LDL-C. For example, in patients starting with an LDL-C level of 2.6 mmol/L (100 mg/dL), a 60% decrease in LDL-C (what a PCSK9 inhibitor typically achieves) should lower LDL-C by 1.6 mmol/L (60 mg/dL), reduce the relative risk of major vascular events by 31%, and, assuming a 5-year major vascular event rate of 25% in a secondary prevention population, yield an absolute risk reduction of 7.8%. If the same patients started with an LDL-C level of 1.8 mmol/L (70 mg/dL), LDL-C should be lowered by 1.1 mmol/L (42 mg/dL) and the relative risk of major vascular events by 23%, which would yield an absolute risk reduction of 5.8%.
That’s quite a change in LDL and Tryglicerides --What was your RAPA dose and frequency?
I started a 5 mg/weekly with GFJ and EVOO then titrated up to 20 mg-biweekly then went down again to 10 mg/weekly with just the EVOO. High doses gave me diarrhea which is the main reason I am now at 10 mg/weekly with EVOO. I am still a little concerned with my lipids because I have a BMI of ~22.5 and eat a quasi-Mediterranean diet.
Thank you – was asking because all my lipid were pretty good (Triglycerides 56/ HDL 68 / LDL 116) before starting RAPA except my doctor wanted my LDL even lower and was trying to force compliance with a Statin (which I’m resisting)
@tongMD my LDL is obviously way above the 70 mg/dL you cite as a starting point for further reduction - but my HDL and Triglycerides are good . . . would you be worried if you were me and go on Statin with the possible sidde effects?
Note your meta analysis is NOT in healthy individuals with low risk and no risk factors in the first place. Context is super important.
I am not your doctor and I haven’t even seen you. Please don’t ask me whether you should go on a statin or not.
I’m certainly not going to be providing anything beyond general information and my nonexpert interpretation of the literature that should never be relied upon to make any sort of treatment decisions.
As mentioned, consider requesting a referral for a lipidologist.
I will mention there isn’t any human data to guide healthy individuals for long-term statin use (ie risk of tendinopathy), nor is HDL really a resolved issue. There is such a gross oversimplification on the immunological function of lipoproteins overall. AFAIK, Attia probably hasn’t mentioned it much at all. I don’t think he’s ever gone over statins, MMP, cartilage, and collagen. Or immunology much.
There is some evidence to even suggest some subtypes of HDL are atherogenic. We really don’t know as much as Attia claims.
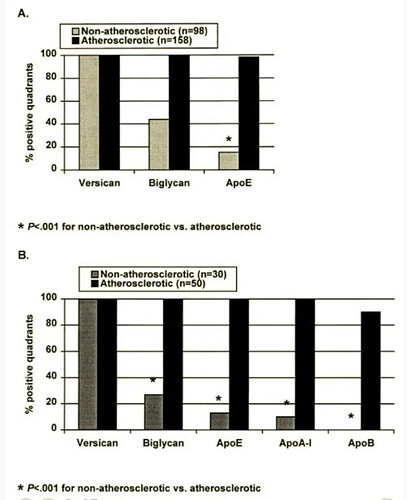
We can see here biglycan which is a proteoglycan that attracts apoB and apoE is in 100% of lesions - but apoE is present in almost 100% of lesions, apoA1 in 100%, and apoB, the supposed initiator, according to Attia, is only present in 90%. If you understand the basics of lipidology and assume Attia’s non-expert hypothesis was flawless, it should be 100% apoB - not 90%.
Now this does not mean anyone should stop a statin if they are indicated for one by their doctor or that apoB is irrelevant. I mentioned the weekly dosing with increased “hepatoselectivity” as an option to reduce risk of myopathy (or potential cognitive risks by avoiding specific statins that may significantly cross BBB) in those where it is indicated by their doctor to talk with their doctor about the benefits vs risks in statin switching - particularly those with risk enhancing factors for atherosclerosis.
It just means the mechanism isn’t as clear as purported and there’s a lot of real gaps. It’s easy to sell a vastly simplified story - “do something” in healthy people and pay me 6 figures per patient as VIP medicine, which has documented risks of its own. If there isn’t a big risk we are reducing - why trade one potential small benefit for several potential risks? There are other options that can be tried first. And even then Attia seems to have been off statins himself - I wonder why since he doesn’t appear to have explained it despite his “faith” in statins. Now if there was better evidence in the context I’m looking for or I’m indicated for it - I’d seriously consider taking a statin. I’m not claiming statins are super harmful drugs either - they’re relatively “safe” overall assuming perfect conditions and usage.
Seems to me that many people can potentially lower LDL from say 100-130 to 70-90 with say 12-15g 100% psyllium husk from food (especially if you have low soluble fiber intake), 5 grams of 100% cocoa bits from food, and/or “perfect” lifestyle factors alone - if you’re aiming for some target. If you’re not discordant - there probably isn’t significant potential benefit in absolute risk reduction from a target of 70-90 through daily combined statins/ezetimibe to say a target 55 in “healthy” people (55 may be a more reasonable target in certain high risk patients with history) with no risk factors. When Attia claims statins are so-called “compound interest” as an investment, that doesn’t take into account other systemic risks. If his position turns out to be true - why not take the route of “compound interest” with the lowest potential risks?
I’m not sure if risk is the most important thing for the healthy, but prevention, preventing ascvd from developing in the first place. Most people (90%+) have a positive CAC at between age 70-90. I think that a very low LDL over a long time might prevent CAC from turning positive at that age. If an LDL is healthy at 30-40 mg/dl we don’t know, but it is for neonatals, and in short term studies, and it does lower risk in those who are unhealthy and at high risk without any observed side effects. So you’ll have to consider this being an ‘ascvd mechanism’. And of course studies are done on those who are unhealthy or at high risk, because without any events you can’t find an effect. I don’t know if you can use mendelian randomization to study very low ldl levels.
On the surface, a target LDL level of less than 70 mg/dl may appear markedly low, but its cogency can be supported by a physiological rationale that we are born with an LDL level of 30–40 mg/dl, and, at that time, the development of the brain is at its peak. The safety of low LDL level has been supported by Ray et al. They reported that the reduction of LDL levels to as low as that of a neonate is safe as well as beneficial in reducing the risk of angina, MI, or cerebrovascular disorder and total mortality [19]. These might be the levels to which humans are inherently adapted, and the levels ventured to be achieved [14]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5937425/
How relevant is this to your situation? How many people age 70-90 had no risk factors and “perfect” lifestyle factors in the first place when say 30-50s? Long time second-hand smoke exposure counts as a risk factor. They probably did not have “perfect” lifestyle factors.
“An important accomplishment of the second half of the 20th century has been the reduction of smoking prevalence among persons aged greater than or equal to 18 years from 42.4% in 1965 to 24.7% in 1997”
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4843a2.htm
The Japanese have a >50% CAC score of 0 in age 65-75 (as far as I could find to compare US vs Japan data) for those with zero main risk factors (smoking, diabetes, hypertension, dyslipidemia) - not even detailed risk stratification using newest in depth criteria. That’s without adjusting for “perfect” lifestyle factors - which I suspect will put that number in much higher proportion for CAC = 0.
Neonatal physiology is very different. For example, heart rate of 140, RR 45, and BP 75/45 is “normal” for neonates. That would warrant a trip to the ER for an adult.
I don’t think staying at 70 - 90 mg/dl will be enough to prevent ASCVD since there is a decrease in risk for those who are unhealthy and who are at high risk when lowering even from that. Meaning it is a factor to consider because there is a causal mechanism. I don’t think you can mitigate this with other factors since it is such a strong factor when all other factors are excluded - in genetic studies and rcts.
Do you understand why the other risk factors matter in calculating risk? Let’s assume your hypothesis is correct - what is the absolute risk reduction in healthy people?
As an example, let’s generously assume everything you assert is absolutely correct with no flaws, if you have a 30-year risk of <10% of ASCVD risk at LDL 100-130, what is the difference in absolute risk reduction for lowering LDL to 40-55 vs LDL 70-90? (You can calculate this with Framingham data)
An intervention reducing risk from 30% to 25% is very different than say 5% to 4%. And that’s generously assuming that the effect would be the same if one has say T2D & HTN - which it probably isn’t.
Meanwhile, we can wait for more data to better refine our approach or newly approved treatments that might even reverse atherosclerosis (or similar) in 30 years. This could very well decrease all-cause mortality far more as a better bet.
You’re ignoring several of the most important considerations.
- Benefit / risk always must be considered.
- Primary prevention differs from secondary.
- The presence of other risk factors
- Absolute vs relative risk.
- Total mortality risks.