And another new paper related to these discussions (in pre-print):
“In contrast, our results showed that 20 mg/kg rapamycin administered pre- or post-MCAO decreased the volume of damage by 35–45%.”
20 mg/kg?! ![]() Even for mice that’s a lot, no?
Even for mice that’s a lot, no?
Yes, 20mg/kg is pretty high for rodents but I’ve seen studies of up to 100mg/kg (short term obviously). Kaeberlein/Bitto did the transient rapamycin lifespan study with 3 months at 8mg/kg (injection). Seemed to go well for the male mice, but a plateau for female mice.
Found the preprint of this paper - should have the details you seek:
Thanks. “intraperitonially with rapamycin (6 mg/Kg; #R-5000, LC laboratories) or vehicle (10% PEG400, 10% Tween 80 in water) on the day of the intrastriatal α-syn PFF injection and every two days thereafter following the intrastriatal α-syn PFF injection for 30 days.”
How does rapamycin absorption differs from intraperitonially VS orally?
No studies I’m aware of off the top of my head, in humans.
In mice - here is some data:
General: Why is it possible for mice to take high rapamycin doses daily?
Specific Equivalents: Concerns on improving Cmax and plasma halflife - #10 by RapAdmin
And see discussion in this paper: Transient rapamycin treatment can increase lifespan and healthspan in middle-aged mice - PMC
We initially used a treatment regimen consisting of intraperitoneal (i.p.) injections of 8 mg/kg rapamycin daily for 90 days. This dose was selected because we have previously found that it increases survival and alleviates disease phenotypes in short-lived mouse models of dilated cardiomyopathy, muscular dystrophy, and the severe mitochondrial disease Leigh Syndrome (Ramos et al., 2012; Johnson et al., 2013). Based on efficacy in the Leigh Syndrome mouse model and serum drug levels in wild type mice, we estimate that this treatment regimen is comparable to dietary delivery of eRapa at approximately 378 ppm (Johnson et al., 2015), or 27-fold higher levels than initially shown to extend lifespan in mice when continuous treatment is initiated at either 9 months or 20 months of age (Harrison et al., 2009; Miller et al., 2011)
I’ve done a bit of i.p dosing in the past. It’s a bit of a half-way route of drug administration (between oral and i.v)
Intraperitoneal injection bypasses first-pass metabolism from the gut, but is still subject to first-pass metabolism by the liver, since absorption is via visceral peritoneum which drains into the hepatic portal vein.
Thanks for your reply!
I get worried that the interactions might be too much.
I pulse the rapa 10mg weekly and pulse off the quercitin (and wish I knew whether to take the quercitin WITH the rapa or not). Besides ambroxol I take once-a-week exenatide, and B12 shots and until someone tells me otherwise that’s enough needles thank-you-very-much :o)
I do take a multi-B (with all the fancy forms like methylcobalamin) and lithium and meloxicam (an anti-inflammatory) and have read (I think Peter Attia?) that NR doesn’t cross the BBB very well.
I wonder about Nilotinib (is it similar in action to quercitin?) and I also wonder about an SGLT2 inhibitor. I haven’t gotten there yet. As I said, I would give a lot for advice. I’m kind of flying blind.
Why quercetin?
For NR in PD: “The investigators found that nicotinamide riboside treatment was well-tolerated and led to a significant increase of NAD+ levels and a reduction in inflammation markers, measured by brain imaging and blood samples.” But more research is needed.
This article is also good (although its findings need to be replicated in trials, it may give some “signal”): Parkinson Symptom Severity and Use of Nutraceuticals 2023
There’s a lot. But on rereading it, I’m thinking I really do want to start nilotinib…probably a bloody fortune.
I don’t know if Nilotinib is potentially helpful, but… Nilotinib is inexpensive (in many parts of the world… 120 rupees to the US$):
Thanks, I didn’t know. 50 mg/kg in rats: Quercetin administration abrogates the Parkinson’s disease (PD)-like motor and non-motor symptoms and attenuates the behavioral, neurochemical and biochemical deficits induced by rotenone toxicity in rats - MDS Abstracts
Unclear benefits per this poll though: Nutrients | Free Full-Text | Parkinson Symptom Severity and Use of Nutraceuticals
(but probably low risk as well, so good bet?)
I haven’t read everything yet, but: “Their re-examination points towards some results suggesting positive effects, but these findings will require further investigation. A parallel clinical trial of nilotinib (supported by Cure Parkinson’s and Van Andel Institute) did not find the same results and indicated that the drug was insufficiently accessing the brain. […] It is important to understand that these studies involve re-analysing data in a biased fashion – searching results for any interesting correlations or effects, and as such, these investigations should be considered as ‘hypothesis generating’ exercises. Researchers use these sorts of analyses to find new ideas for experiments that can then be tested, and further research will be required before isradipine or nilotinib can be re-examined in people with Parkinson’s.” ( Post-hoc analyses of the isradipine and nilotinib trial results - Cure Parkinson's ).
What’s the relationship between quercetin and nilotinib/dasatinib btw?
If you’re already taking lithium, then you may need to change your dosage if you start an SGLT2i (see: Starting empagliflozin or dapagliflozin in patients on lithium? Monitor lithium levels )
What’s your current lithium dose? This trial suggests 30-45mg/day, “slowly titrated in each patient up to the maximum tolerated dosage in this range”: CTG Labs - NCBI
Regarding Nilotinib, I guess we’ll soon get the results of this trial, which may help you to make a decision: CTG Labs - NCBI
Also: have you checked your blood pressure? (see thread: Optimal Blood Pressure we Should Target? Systolic Under 110 or 100? ) I wonder whether lowering mean BP AND BP variability can decrease PD risk (for instance with an ARB/sartan or a dihydropyridine calcium channel blockers like isradipine).
Quercitin and nilotinib (plus like a million other things I guess) are senolytics, and somewhere I read about “synergistic cytotoxicity” which maybe was meant to be good but sounded a bit scary to me. I’m a little protective of my brain cells. But really, I don’t know. These articles quickly soar over my head.
I DO take lithium, although my doctor for some reason is terrified of it (actually, he is convinced it causes tremor) so I only take 5mg a day. I wouldn’t mind titrating up–think I’ll look up signs of maxing out. Thx!
Yes, I eagerly follow all the trials, particularly the repurposed drug trials. Wish results came faster!
Parkies tend to run low blood pressure, and I am no exception, generally running like 110/65 or so. Maybe it’s one bright spot in an otherwise grim landscape :o)
Your doctor is right, but as far as I can determine it’s only at prescribed therapeutic levels.
Does your doctor know that the doses of lithium we are taking in the form of lithium orotate are much much lower than commonly prescribed?
I have been taking lithium orotate for over two decades at doses from 5 - 15 mg of elemental lithium.
As I reported previously, I had started to develop what I believed were age-related "essential tremors. I did not associate the tremors with the lithium supplement. But, who knows?
A few weeks after I started rapamycin my tremors went away and I have been free of them since. I was not aware that lithium was a probable cause as I developed tremors when I was about 78 yrs. old.
“The available evidence suggests higher lithium doses and plasma levels are associated with an increased risk of developing lithium tremor, implying a dose-response relationship”
“Tremor was related to higher doses, to higher concentrations, and to higher gradients of lithium in plasma”
“Lithium tremor revisited: pathophysiology and treatment”
https://sci-hub.se/10.1111/acps.12171
I take 1 mg of lithium orotate daily. It seems to be a good microdose. Lithium is also synergistic with Rapamycin. Supposedly it cancels Rapa’s lipid effects. Maybe I need to dose higher?
http://www.pnas.org/doi/10.1073/pnas.1913212116
However, the study is done in flies, which is never 100% translatable. So, here’s hoping.
Yes it’s frustrating how slow trial results come out. You can often get them faster by contacting the authors. For instance the results of this trial are not yet out ( Risk Reduction for Alzheimer's Disease - Full Text View - ClinicalTrials.gov ) but the author told me that it failed: 2y of intensive BP control with losartan and amlodipine + physical exercise did not improve cognitive performance.
Yes I’m aware of the hypotension risk in PD but I’d still look at BP, especially continuously over a day or week (for instance with a device like Aktiia) because:
- Hypertension in mid-life may be a risk factor for PD later in life: Hypertension and Diagnosis of Parkinson’s Disease: A Meta-Analysis of Cohort Studies - PMC
- Some antihypertensive drugs are considered as potential repurposed treatments for PD (namely CCBs like isradipine and ARBs like candesartan/telmisartan)
- Blood pressure variability (BPV, aka the variations during the day and week) seem to matter more than the mean for neurological diseases. Maybe you spend a lot of time during the day in hypotension and/or hypertension and don’t know it. And it seems that CBBs and ARBs can “smooth” the BP (without reducing it too much at low doses). See: Blood pressure variability: methodological aspects, clinical relevance and practical indications for management - a European Society of Hypertension position paper 2023
- Knowledge is power.
- It may be useful to detect and manage orthostatic hypotension: Smartwatch May Help Parkinson’s Patients Manage Blood Pressure Drops
Regarding telmisartan/candesartan, see as well: The Endotoxin Hypothesis of Parkinson’s Disease 2023:
If LPS contributes to PD, then a number of possible therapeutic strategies could be considered for further evaluation in clinical trials as outlined below. However, if LPS is elevated in only a subset of PD, patient stratification would be essential for targeting the most appropriate patients. Monitoring of blood LPS levels in such trials would provide important validation of the mechanistic principle, alongside clinical efficacy measures. […] (4) Blocking LPS receptors. Candesartan, an existing drug licensed for the treatment of hypertension, has been shown to reduce TLR4 expression and activity, is expected to cross the BBB, and has a good safety profile, making it an attractive candidate for repurposing in Parkinson’s disease.
Does anyone know how to test for serum LPS?
I’m also curious:
- Are there things that you tried but stopped because they did not seem to work or had bad side effects?
- Among all your interventions, if you had to keep only one, which one would it be?
- Have you considered selegiline/deprenyl at a low dose? (it may protect the BBB from LPS, see: Anyone taking Selegiline / Deprenyl For Longevity? - #55 by Vulcan )
Also, what about your LDL levels and have you considered statins? @Joseph_Lavelle wrote recently:
ldl picks up the LPS which is then cleared from the body when the ldl is picked up by the liver. Statins make the liver produce more ldl receptors to remove ldl from the bloodstream. This is why ldl measurements decrease and how the lps gets taken out. So, statins help with removal of lps, according to Krause.
I don’t know if the above is correct but the use of cholesterol-lowering drugs is associated with decreased risk for PD:
- News in Context: Cholesterol Medication and Parkinson’s 2022: “In the meantime, if you need a cholesterol medication, it may be worth discussing whether a statin might be beneficial, particularly if you live with Parkinson’s or with a risk for the disease, such as having a family member with PD, carrying a genetic link, or acting out your dreams.” (MJ Fox Foundation)
- Statins may reduce the risk of Parkinson’s-like symptoms in older adults 2022
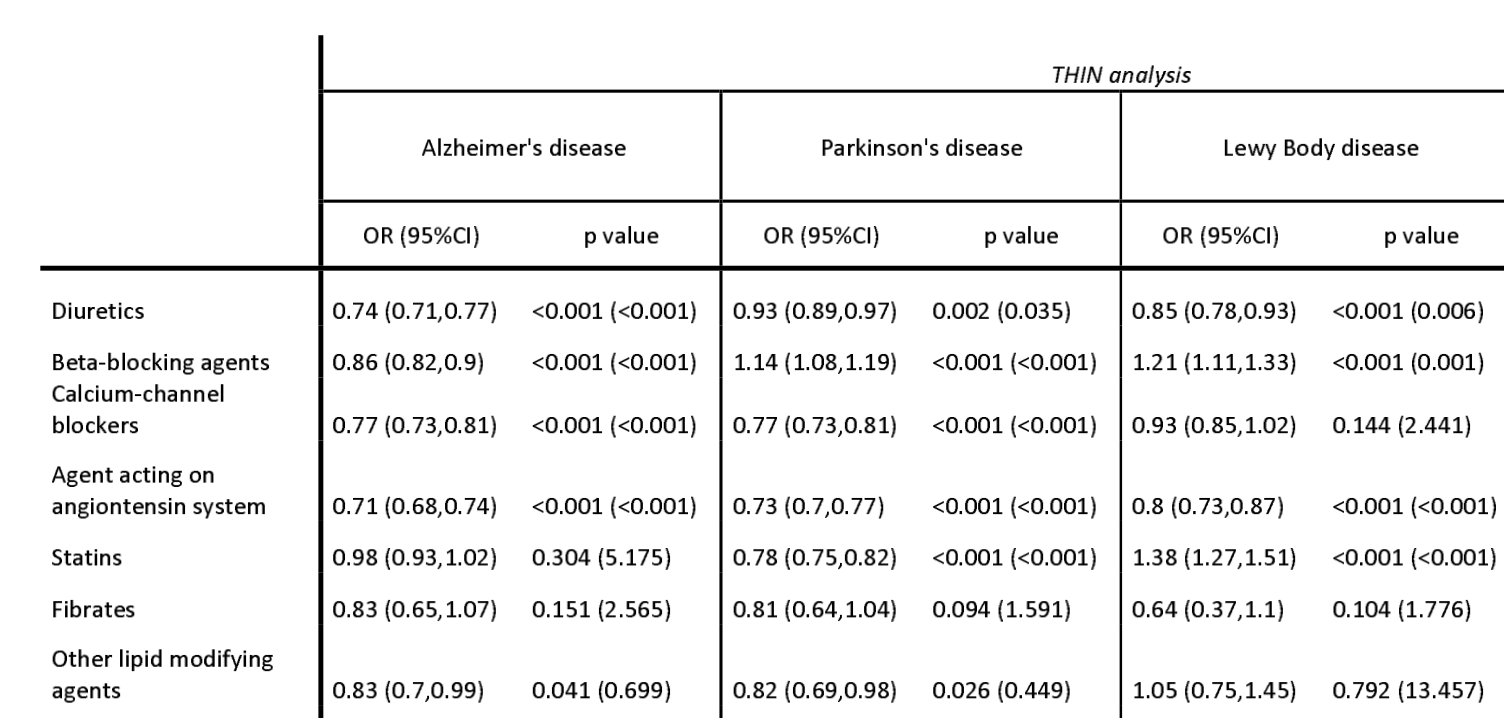
- Association of cardiovascular disease management drugs with Lewy body dementia: a case–control study 2023
- A Comparison Between Early Presentation of Dementia with Lewy Bodies, Alzheimer’s Disease, and Parkinson’s Disease: Evidence from Routine Primary Care and UK Biobank Data 2023
There was one successful clinical trial of lovastatin: A Double-Blind, Randomized, Controlled Trial of Lovastatin in Early-Stage Parkinson’s Disease 2021
Lovastatin 80 mg/day or placebo with 1:1 randomization was administered for 48 weeks. […] Lovastatin treatment in patients with early-stage PD was associated with a trend of less motor symptom worsening and was well tolerated.
And one failed of simvastatin: Evaluation of Simvastatin as a Disease-Modifying Treatment for Patients With Parkinson Disease: A Randomized Clinical Trial 2022
1-month phase of simvastatin, 40 mg daily, followed by 23 months of simvastatin, 80 mg daily, before a 2-month washout period […] In this randomized clinical trial, simvastatin was futile as a disease-modifying therapy in patients with PD of moderate severity, providing no evidence to support proceeding to a phase 3 trial.
So maybe statins are only symptomatic and not DMT.
There’s an ongoing study to see if statins can prevent Levodopa Induced Dyskinesia: Preventing Levodopa Induced Dyskinesia in Parkinson’s Disease With HMG-CoA Reductase Inhibitors (STAT-PD)
Sorry for the 3rd post in a row but wow… I’ve just checked the supplemental material of the just published Association of cardiovascular disease management drugs with Lewy body dementia: a case–control study and table S5 shows that the 4th best-performing drug to prevent Lewy body dementia is… the immunosuppressant Tacrolimus! With a 1y OR of 0.46 [0.32-0.59]. Tacrolimus is not in their 3y model, but the 9th most performing in the 3y model is another immunosuppressant currently tested in the ITP: Methotrexate. This is surprisingly not mentioned in the paper itself.
I know, lithium causes tremors, but I think you’re right–more at the doses used to treat bipolar disorder, which is grams a day. The dose makes the poison, eh?
The problem is, my doctor thinks I’m nuts (you’re taking rapamycin!? That’s a dangerous cancer drug! You’re using exenatide!? It has side effects! ) so I have trouble getting him to listen to anything.
You know, having Parkinson’s has side effects. Growing old has side effects. We choose which ones WE want to risk.
Ooof. You ask hard questions.
Let’s see–I did try the whole NAC NMN thing, and I’m ashamed to say part of the reason I leapt on the Peter-Attia-It-Doesn’t-Cross-The-BBB-anyway conclusion was because I didn’t like the pills: they were big and smelled terrible.
Metformin. Also read along the way there wasn’t a lot of point. Also read some stuff about metformin vs. exercise…and I exercise like a crazy person.
Mannitol. There were some iffy, non-placebo controlled positive-ish results that I ultimately decided I didn’t buy.
Tryptophan–because I listened to a far-out theory by Dr. Jonathan Sackner-Bernstein and I’ll try anything. In a nutshell, he believes PD is lack of dopamine transport, not lack of dopamine. Since dopamine is toxic (thus killing their overstuffed neurons) he thinks the fix is to block synthesis. Ha. I felt awful pretty quickly.
Just FYI: Venglustat. I was in the Sanofi/Genzyme study, NOT on placebo, for nearly the full three years, before the study was stopped.
I take Azilect, which was all the neuroprotective rage when I was diagnosed. I know it’s kind of fallen out of favor. I’ve debated switching to seligiline.
Here’s what I think in general though: any treatment for the cause of PD (as opposed to the symptoms) isn’t gonna make you feel miraculously better. It’s going to keep neurons from dying, or maybe nurture baby ones, and I’m not convinced that’ll be detectable on a day-to-day basis.
If something makes you feel different overnight, to me it screams placebo.
I am musing on what I wouldn’t give up. I didn’t even MENTION my keto diet, or hot tub/cold pool, or exercise, or non-negotiable sleep routine. You see?
BTW I’ve had PD for 10 years.