I’ve been taking Niacin for 6 months now, 1500 mg a day. It has lowered my Lpa from 130 to 68 nnmol/L. Then I read this study today. Should I stop taking the Niacin?
Wow. That is very powerful.
I’ll take a look at the link you sent later.
Btw, have you measured to see if it helped raise your NAD+ levels?
It’s tough to know
-
on the one hand it’s a good team, published in a good journal, with quite high hazard ratios
-
on the other hand they are just talking about stable patients in general and not people with high Lp(a) (and your was really lowered a lot), the study was not a clinical trial but just an association study, etc
Below is the abstract from the paper (I could not access the whole paper).
Do you have the change in your levels of HDL (did it go up?) and Apo B (or LDL, do it/they go down)?
The mechanism by which they say that it increases risks seems to be connected to (vessel) inflammation - perhaps it could make sense to do some extra testing around that…!
Suggest you give your context, mention the new paper and ask Sam T via twitter - he is a world authority on Lp(a) and seems to respond to people’s questions quite often.
—-
Abstract
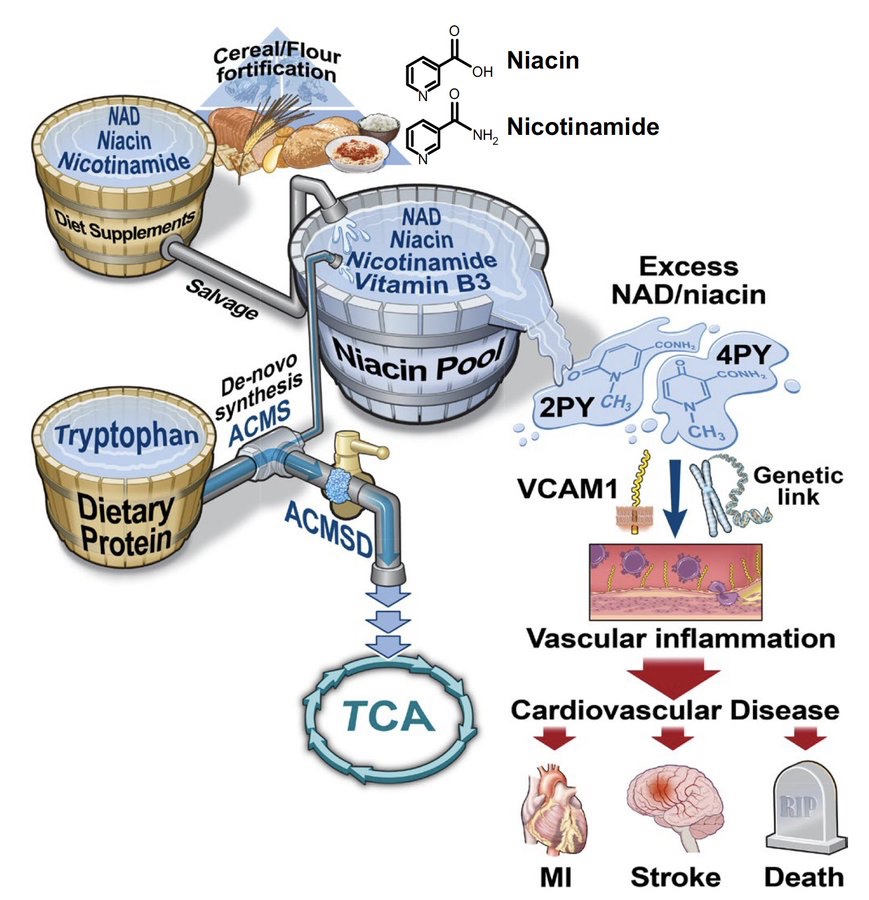
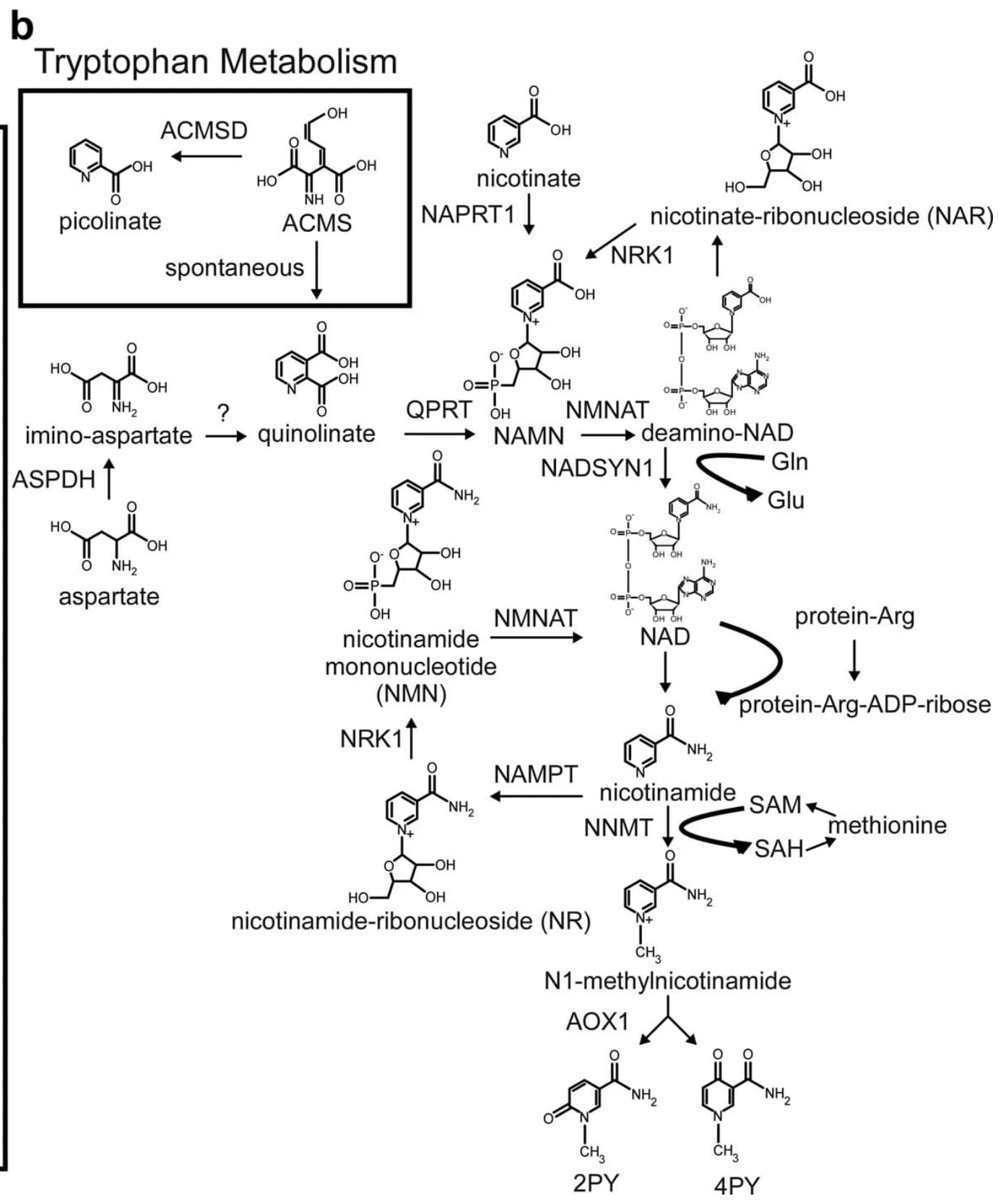
Despite intensive preventive cardiovascular disease (CVD) efforts, substantial residual CVD risk remains even for individuals receiving all guideline-recommended interventions. Niacin is an essential micronutrient fortified in food staples, but its role in CVD is not well understood. In this study, untargeted metabolomics analysis of fasting plasma from stable cardiac patients in a prospective discovery cohort (n = 1,162 total, n = 422 females) suggested that niacin metabolism was associated with incident major adverse cardiovascular events (MACE). Serum levels of the terminal metabolites of excess niacin, N1-methyl-2-pyridone-5-carboxamide (2PY) and N1-methyl-4-pyridone-3-carboxamide (4PY), were associated with increased 3-year MACE risk in two validation cohorts (US n = 2,331 total, n = 774 females; European n = 832 total, n = 249 females) (adjusted hazard ratio (HR) (95% confidence interval) for 2PY: 1.64 (1.10–2.42) and 2.02 (1.29–3.18), respectively; for 4PY: 1.89 (1.26–2.84) and 1.99 (1.26–3.14), respectively). Phenome-wide association analysis of the genetic variant rs10496731, which was significantly associated with both 2PY and 4PY levels, revealed an association of this variant with levels of soluble vascular adhesion molecule 1 (sVCAM-1). Further meta-analysis confirmed association of rs10496731 with sVCAM-1 (n = 106,000 total, n = 53,075 females, P = 3.6 × 10−18). Moreover, sVCAM-1 levels were significantly correlated with both 2PY and 4PY in a validation cohort (n = 974 total, n = 333 females) (2PY: rho = 0.13, P = 7.7 × 10−5; 4PY: rho = 0.18, P = 1.1 × 10−8). Lastly, treatment with physiological levels of 4PY, but not its structural isomer 2PY, induced expression of VCAM-1 and leukocyte adherence to vascular endothelium in mice. Collectively, these results indicate that the terminal breakdown products of excess niacin, 2PY and 4PY, are both associated with residual CVD risk. They also suggest an inflammation-dependent mechanism underlying the clinical association between 4PY and MACE.
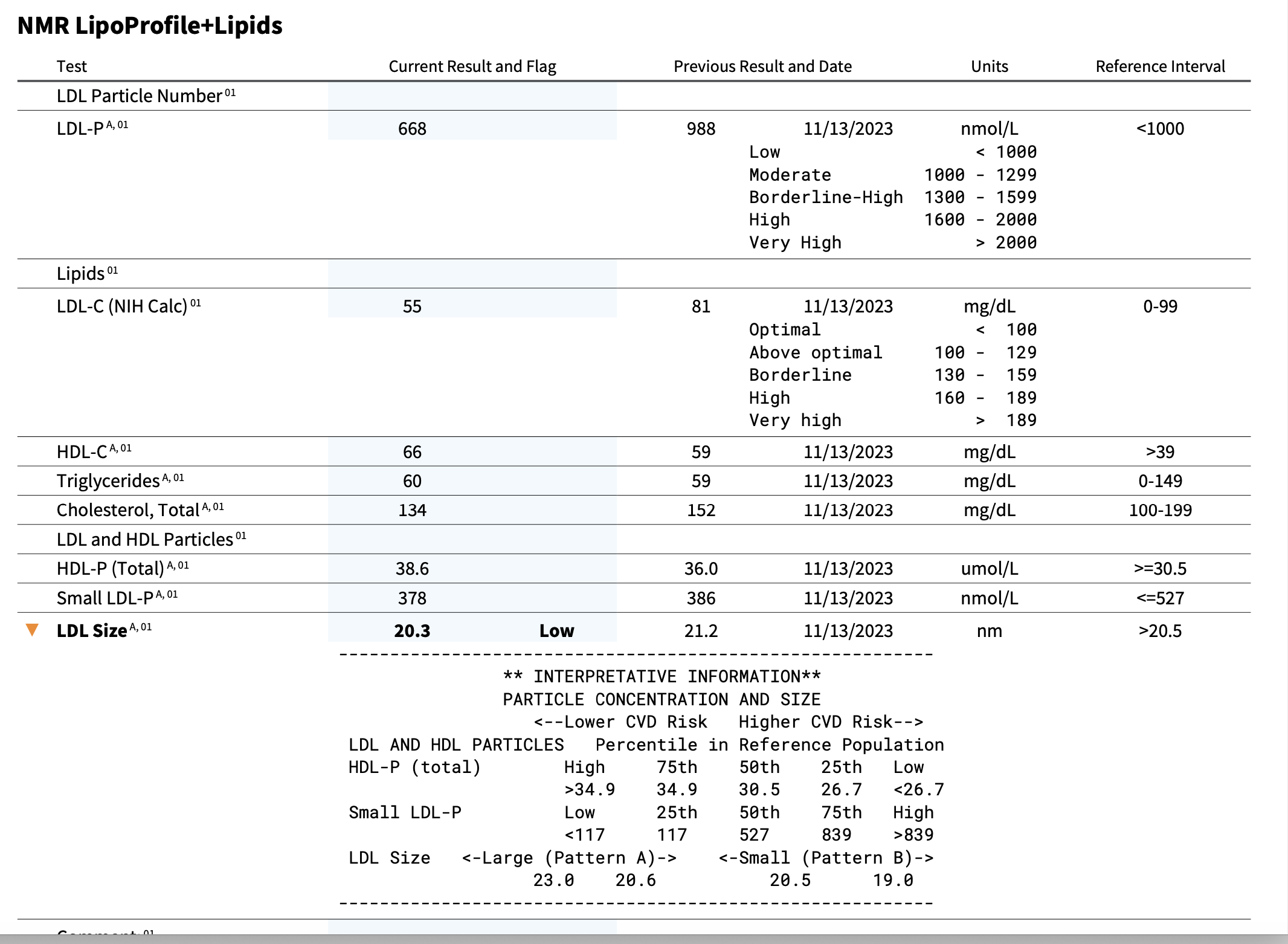
Thanks for the replies. Interesting enough I have an appointment with Dr. T in about ten day when I’m visiting San Diego. I’ve had the appointment in the books for 6 months so it’s timely. Here is a screen shot of my lipids. My CRP was less than 1. I will follow up after having the discussion with Dr. Tsimikas. Any further insights would be appreciated. Note; regarding Lipids. I’m not on a statin but I’m on Nexletol.
It doesn’t sound good…
A terminal metabolite of niacin promotes vascular inflammation and contributes to cardiovascular disease risk
Despite intensive preventive cardiovascular disease (CVD) efforts, substantial residual CVD risk remains even for individuals receiving all guideline-recommended interventions. Niacin is an essential micronutrient fortified in food staples, but its role in CVD is not well understood. In this study, untargeted metabolomics analysis of fasting plasma from stable cardiac patients in a prospective discovery cohort (n = 1,162 total, n = 422 females) suggested that niacin metabolism was associated with incident major adverse cardiovascular events (MACE).
Paywalled Paper:
I have not. Should NAD plus levels not be raised? Please advise.
Niacin is used to treat hyperlipidemia especially as an adjunct therapy to statins if LDL isn’t getting low enough. Side effects can include high uric acid, increase risk of gout and insulin resistance, cause hyperglycemia and cause flushing / pruritis:
I would say no it does not induce heart disease and it would require good evidence to convince me at least of that. That paper is not a clinical trial or mendelian randomization study and it seems that niacin is used or at least have been used a lot in clinical practice.
I might actually try this to get my apoB maybe down a bit and HDL up. The Poor Man’s CETP inhibitor.
Thank you for the reply. This is very helpful.
Telmisartan is good at reducing vascular inflammation ![]()
Niacin was commonly recommended for coronary heart disease prevention until about 10 years ago when that began to change.
https://pubmed.ncbi.nlm.nih.gov/28927896/
I’m currently taking Telmisartan so that is good news.! Thanks
A priori I would expect this to be a bigger potential issue for NR and NMN, as my understanding is they’re mostly converted to NAM prior to uptake, and NAM is closer to 2PY and 4PY than niacin/nicotinate.
I would say no it does not induce heart disease and it would require good evidence to convince me at least of that. That paper is not a clinical trial or mendelian randomization study and it seems that niacin is used or at least have been used a lot in clinical practice.
It is a longstanding paradox that niacin doesn’t reduce CVD risk commensurate to its reduction in LDL. But yeah would be nice to see MR or RCT. They do provide some mechanistic evidence centered around increased recruitment of immune cells to vascular endothelium.
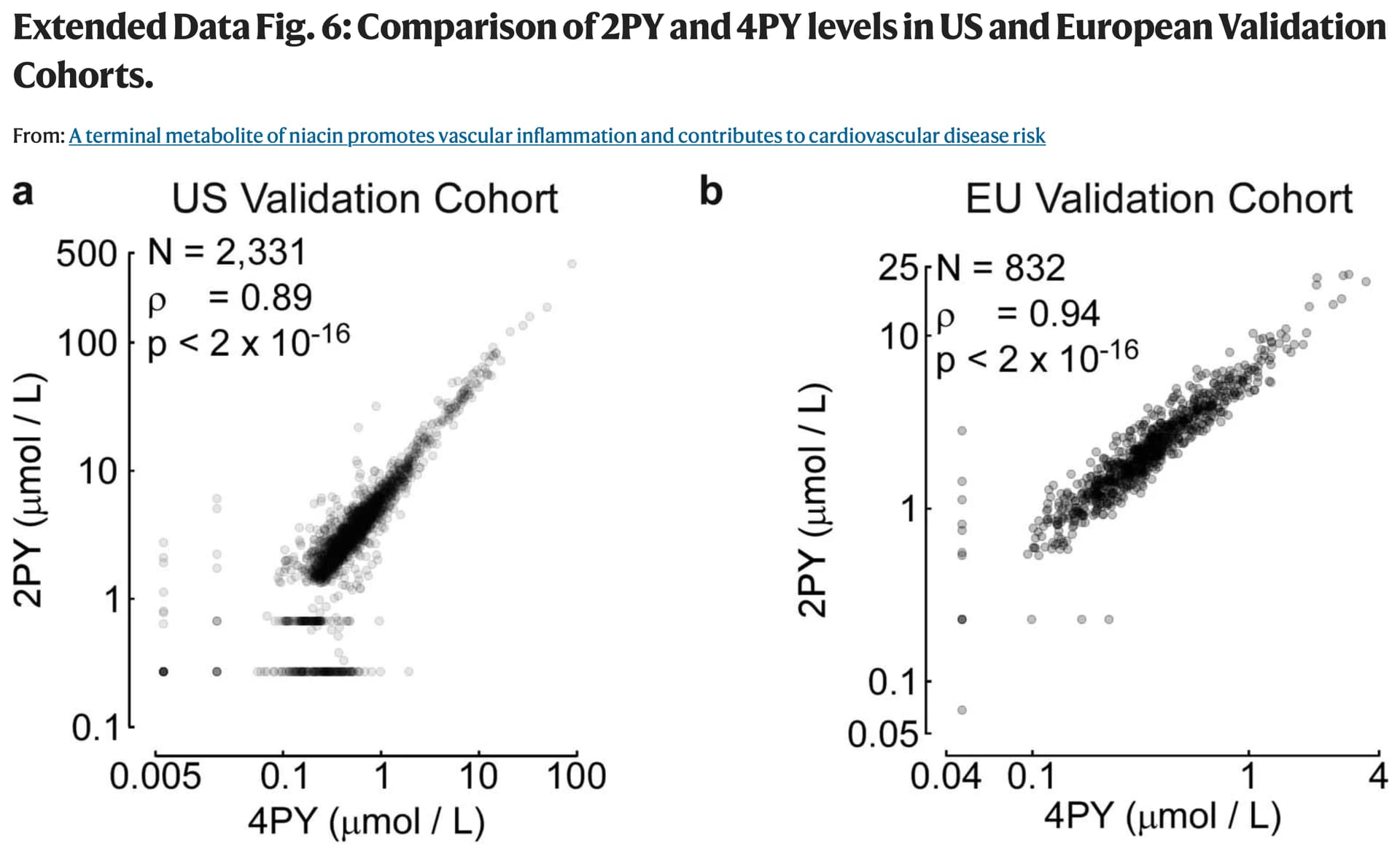
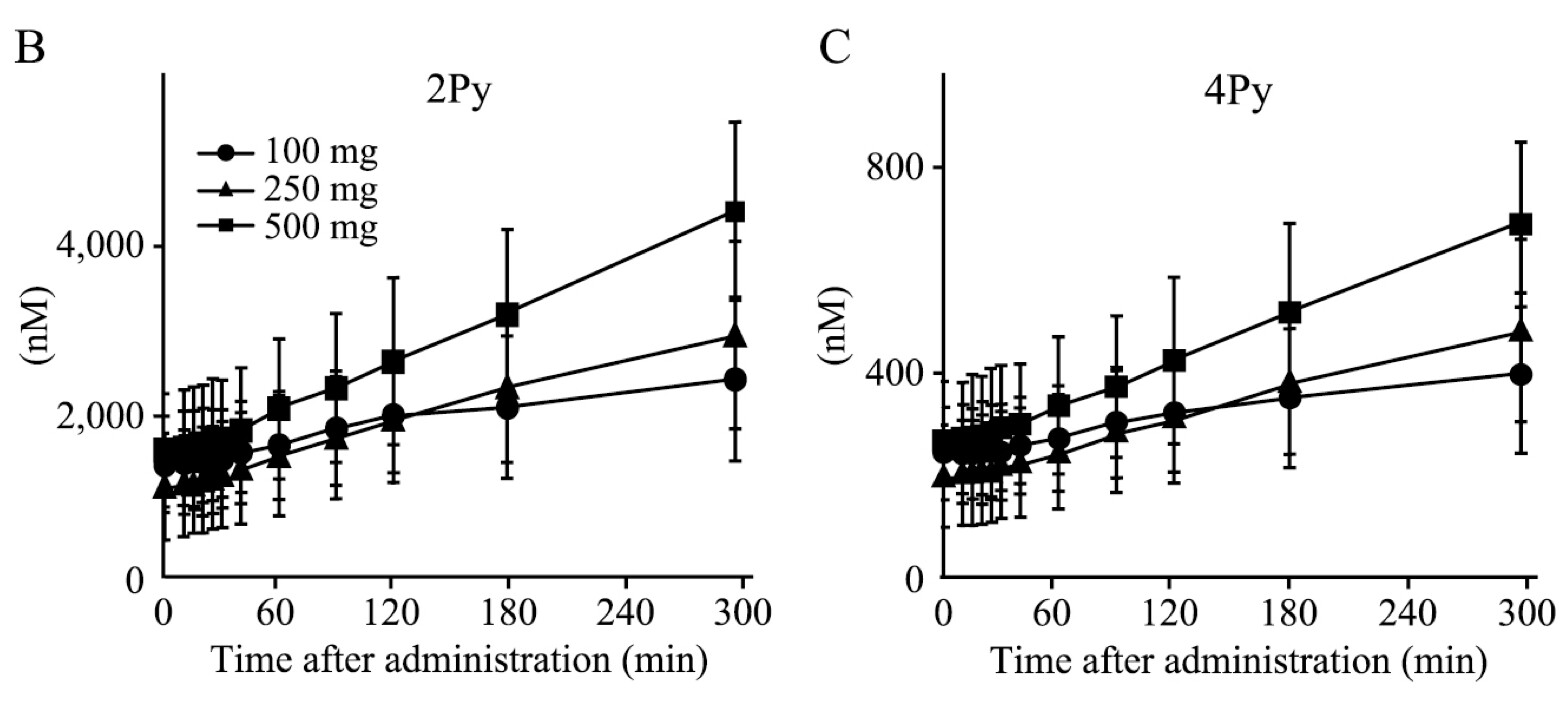
Below is serum levels from the recent study, you can see that 4PY levels at the lower end are around 0.1 uM, whereas 2PY levels are around 1uM at the lower end.
Also plasma levels of 2PY and 4PY following NMN administration in 10 healthy Japanese men.
Interestingly, Niacin and Nicotinamide/Niacinamide don’t have the same effect on lipids.
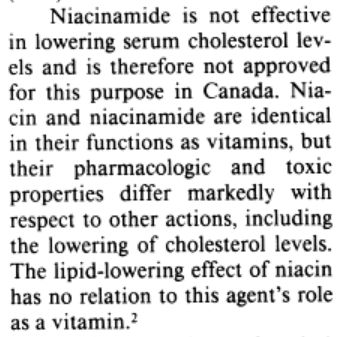
from here:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1336277/?page=1
@Isutiger
Supplemental niacin can have a host of side effects, including:
Severe skin flushing combined with dizziness
Rapid heartbeat
Itching
Nausea and vomiting
Abdominal pain
Diarrhea
Gout
Liver damage
Diabetes
P henome-wide association analysis of the genetic variant rs10496731, which was significantly associated with both 2PY and 4PY levels, revealed an association of this variant with levels of soluble vascular adhesion molecule 1 (sVCAM-1). Further meta-analysis confirmed association of rs10496731 with sVCAM-1 (n = 106,000 total, n = 53,075 females, P = 3.6 × 10−18). Moreover, sVCAM-1 levels were significantly correlated with both 2PY and 4PY in a validation cohort (n = 974 total, n = 333 females) (2PY: rho = 0.13, P = 7.7 × 10−5; 4PY: rho = 0.18, P = 1.1 × 10−8). Lastly, treatment with physiological levels of 4PY, but not its structural isomer 2PY, induced expression of VCAM-1 and leukocyte adherence to vascular endothelium in mice.
So they point to an association of 4PY to sVCAM-1. Is that the factor related to CVD?
The study below was a clinical study done in 2000, and arrived at the opposite conclusion.
OBJECTIVES
The purpose of this study was to evaluate whether soluble vascular cell adhesion molecule-1 (sVCAM-1) is a marker for increased cardiovascular risk.
BACKGROUND
Soluble forms of cellular adhesion molecules (CAMs) may be useful markers of endothelial activation and local or systemic inflammation. Recent studies indicate that plasma concentration of soluble intercellular adhesion molecule-1 (sICAM-1) is elevated many years before a first myocardial infarction (MI) occurs. However, only a few prospective studies have evaluated whether sVCAM-1 is also a marker for increased cardiovascular risk.
METHODS
Baseline plasma samples were obtained prospectively from 14,916 healthy participants in the Physicians’ Health Study. In a nested, case-control study design, the plasma concentration of sVCAM-1 was measured in 474 men with confirmed MI during the nine-year follow-up period, and in an equal number of control subjects who remained free of reported cardiovascular disease and who were matched for age, smoking status and length of follow-up.
CONCLUSIONS
In contrast to previous data on sICAM-1, we found no evidence of an association between sVCAM-1 levels and the risk of future MI in a large cohort of apparently healthy men. These data suggest important pathophysiologic differences between sVCAM-1 and sICAM-1 in the genesis of atherothrombosis.
It is sICAM that is the cardiovascular risk, not sVCAM.
The authors of the old study are all MDs. One of them is a Fellow of the American College of Cardiology.
Paul M Ridker MD,FACC
None of the authors in the new study has an MD affixed after their name. I clicked on each and every name in the new article.
MDs are trained as clinicians, not researchers. They have to get extra training to have any idea what they are doing or talking about when it comes to research. PhDs are first and foremost researchers, and are trained from the ground up as such. That’s not to say there aren’t some world-class MD researchers (there are), but I don’t think it’s useful at all to distinguish good vs bad studies on this criterion.
They’re both markers of inflammation related to CVD risk.
Sorry. Forgot to post the link.
https://www.sciencedirect.com/science/article/pii/S0735109700007427
They’re both markers of inflammation related to CVD risk.
The second study acknowledged that, as I quoted above, and re-quote here. That is why they conducted the study.
Recent studies indicate that plasma concentration of soluble intercellular adhesion molecule-1 (sICAM-1) is elevated many years before a first myocardial infarction (MI) occurs. However, only a few prospective studies have evaluated whether sVCAM-1 is also a marker for increased cardiovascular risk.
Their conclusion is that we found no evidence of an association between sVCAM-1 levels and the risk of future MI
One may agree or disagree with the second study’s conclusion. I am merely sharing the study I found. It is the members’ prerogative to read or ignore the post.
Your study presents a qualified conclusion. There must be elevated sVCAM-1 in diabetic patients.
In conclusion, levels of sVCAM-1 are independently associated with the risk of cardiovascular mortality in type 2 diabetic subjects and therefore might be useful for identifying subjects at increased cardiovascular risk.