This is an old (2001) paper, but probably just as true today as when it was first published:
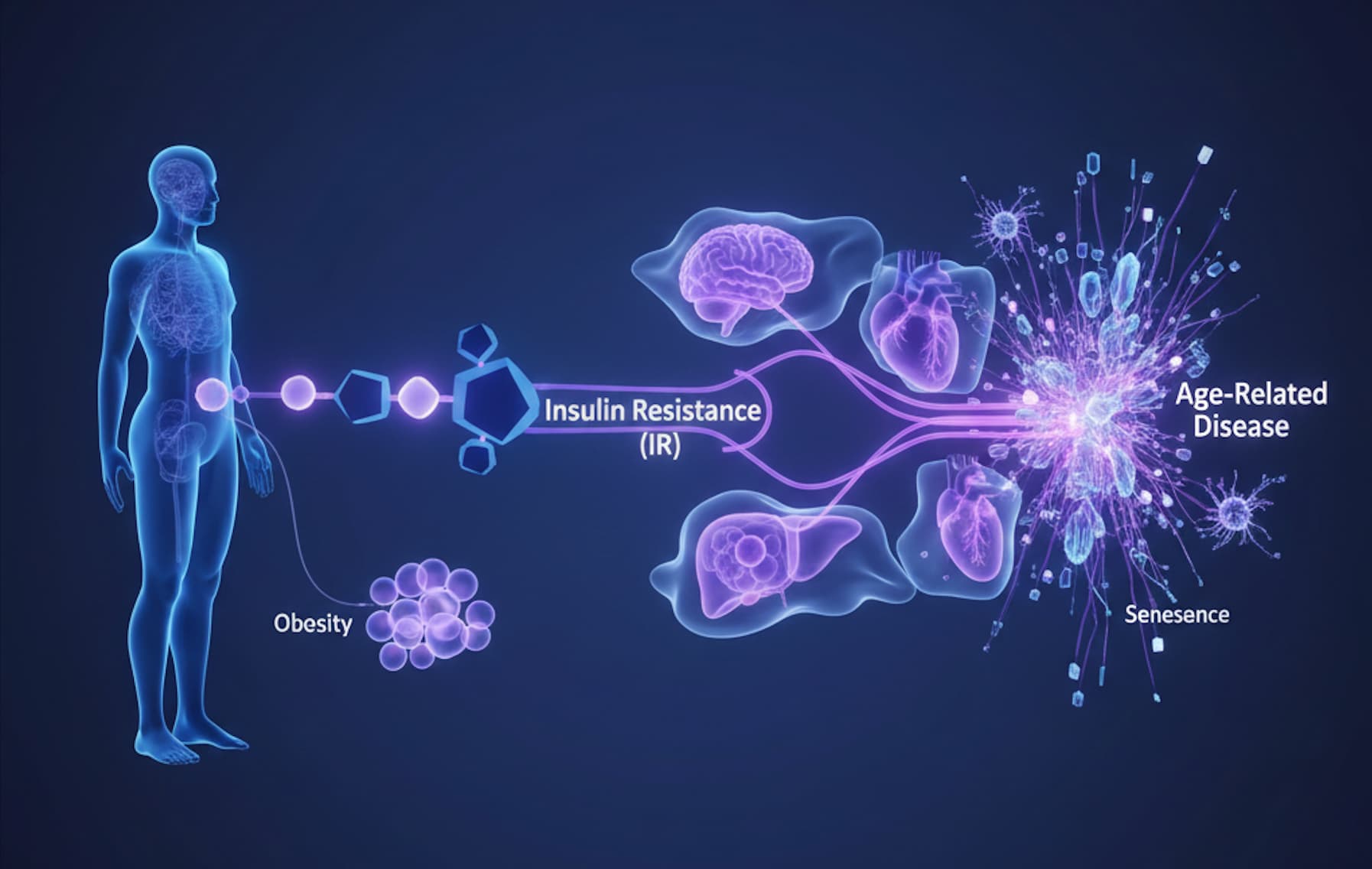
In a landmark prospective study that challenges the “obesity paradox,” researchers at Stanford University have demonstrated that insulin resistance (IR) is not merely a comorbidity of obesity but an independent, primary driver of age-related disease in healthy, non-obese individuals. The findings are stark: over a 6-year period, zero clinical events (stroke, cancer, hypertension, or heart disease) occurred in the most insulin-sensitive third of the population.
This study dismantles the assumption that a normal BMI guarantees metabolic health. By using the gold-standard “Insulin Suppression Test” (IST) rather than simple fasting glucose, the authors stratified 208 healthy volunteers into tertiles of insulin resistance. While the most resistant group suffered a barrage of age-related pathologies (28 events), the insulin-sensitive group remained completely disease-free. This implies that hyperinsulinemia is a “silent” accelerator of aging that operates beneath the radar of standard physical exams, driving pathology years before hyperglycemia (diabetes) is diagnosed. For the longevity biohacker, this paper provides the definitive metric for healthspan: Insulin Sensitivity.
Source:
- Paper: Insulin Resistance as a Predictor of Age-Related Diseases
- Date: 01 August 2001
- Stanford University, USA – The Journal of Clinical Endocrinology & Metabolism
- Impact Score: 5. Evaluated against a typical high-end range of 0–10+ for specialty medicine, this is a High impact journal.
Related Reading: Post-meal blood sugar spikes linked to increased Alzheimer's risk
Part 2: The Biohacker Analysis
Study Design Specifications
- Type: Prospective Cohort Study (Level C).
-
Subjects: 208 healthy, non-obese (BMI < 30 kg/m²) human volunteers.
- Note: Excluding obese individuals isolates IR as a variable independent of adiposity.
- Methodology: Gold-Standard Insulin Suppression Test (IST). Subjects infused with somatostatin, insulin, and glucose to measure Steady-State Plasma Glucose (SSPG).
- Follow-Up: 4–11 years (Mean: 6.3 ± 0.2 years).
Healthspan Analysis (The “Human Lifespan” Proxy)
- Translational Gap: This is a human clinical study, not a murine lifespan experiment. Therefore, we measure “Event-Free Survival” rather than maximum lifespan.
-
The “Zero-Event” Anomaly:
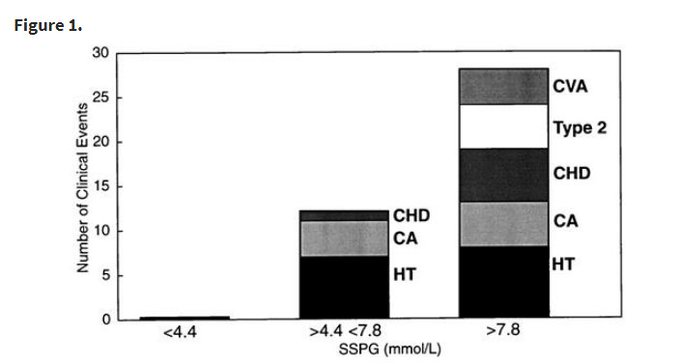
- Insulin Sensitive Tertile (SSPG < 4.4 mmol/L): 0 clinical events. (100% Healthspan maintenance over duration).
- Insulin Resistant Tertile (SSPG > 7.8 mmol/L): 28 clinical events (inc. Hypertension, Cancer, Stroke, CHD).
- Risk Ratio: The risk difference is effectively infinite between the top and bottom tertiles during the observation window.
Mechanistic Deep Dive
- The Hyperinsulinemia Toxicity Thesis: The study suggests that compensatory hyperinsulinemia (the body pumping out excess insulin to overcome resistance) is the primary driver of pathology, not just high glucose.
- Oncology (IGF-1 Axis): The study observed 9 cancer cases, all in the insulin-resistant tertiles. High circulating insulin upregulates IGF-1 bioactivity and activates PI3K/Akt/mTOR pathways, promoting cellular proliferation and inhibiting apoptosis (a pro-tumorigenic state) Insulin Resistance and Cancer (2025).
- Vascular Erosion: Insulin resistance abrogates NO-mediated vasodilation, leading to stiff, hypertensive arteries. The “Resistant” group had significantly higher blood pressure despite starting with normal vitals.
Critical Limitations
- Sample Size: n=208 is relatively small for a prospective cohort.
- Duration: ~6 years is insufficient to measure “Lifespan” extension, only mid-term “Healthspan.”
- Causality: As an observational study, it proves prediction, not causation. However, the dose-response relationship (Tertile 1 vs 2 vs 3) strongly implies a biological gradient.