It’s a good question. At the moment I just get HsCRP and it’s very low (.03-.07). But I’m interested in the best testing. Especially for measuring the benefits of something like taking rapamycin which often doesn’t seem to show any changes in blood markers or even the latest epigenetic BioAge clocks. So I’m on the lookout for tests that would consistently show a benefit of weekly (or?) rapamycin or metformin or SLGT2 or tadalafil or any intervention that is done for longevity and might not show an immediate effect. Even something like reducing arterial plaque thickness (if possible) would be a slow process that might take years but it would improve circulation and therefor both healthspan and lifespan. And it’s measurable.
Inflammation besides being a hallmark of aging (Inflammaging) is also a marker of atherosclerosis so I believe that if your inflammation markers are very low, you aren’t actively building plaque. How effectively do the different inflammation markers measure endothelial inflammation? Lp-PLA2 seems to be a specific marker.
Lp-PLA2 is a 50-kDa, Ca2±independent enzyme associated with LDL. Small dense LDL particles are very atherogenic and readily undergo oxidative modification (117). The enzyme is a subtype of a growing family of A2 phospholipases and is secreted mainly by macrophages, monocytes, mast cells, and T lymphocytes. The enzyme has proinflammatory properties because it hydrolyzes oxidized phospholipids to lysophosphatidylcholine and free oxidized fatty acids and thus is the enzyme responsible for most of the increased lysophosphatidylcholine content of OxLDL particles. The atherogenic potential of OxLDL has been attributed to this high lysophosphatidylcholine content. Several prospective epidemiological studies have reported that Lp-PLA2 is a predictor of CAD (117), although controversy persists as to its independence from LDL cholesterol. The relationship of Lp-PLA2 to LDL cholesterol is also supported by several studies showing equivalent decreases in Lp-PLA2 and LDL cholesterol levels in response to several different classes of lipid-lowering agents (118). Further, in contrast to the situation for CRP, the levels of which are reduced by statin therapy in a manner independent of the effects on LDL cholesterol, there is little evidence that statins lower Lp-PLA2 levels once LDL cholesterol level reduction is accounted for.
https://jnm.snmjournals.org/content/48/11/1800#sec-22
What I’m most interested in is the different mechanisms of the inflammation markers. Il-6 and HsCRP seem to correlate closely, but I’d be interested in when they diverge.
From google AI:
When inflammation is triggered, IL-6 is released into the bloodstream by neutrophils, macrophages, and other cells at the site of damage or infection.
IL-6 stimulates the liver to produce CRP and other acute phase proteins, which are then released into the bloodstream.
As IL-6 levels rise, so do CRP levels. In severe infections or burns, CRP levels can increase from less than 1 μg/mL to up to 1000 μg/mL.
IL-6 and CRP are both markers of systemic vascular inflammation. They have been independently associated with cardiovascular events and mortality in both healthy men and women.
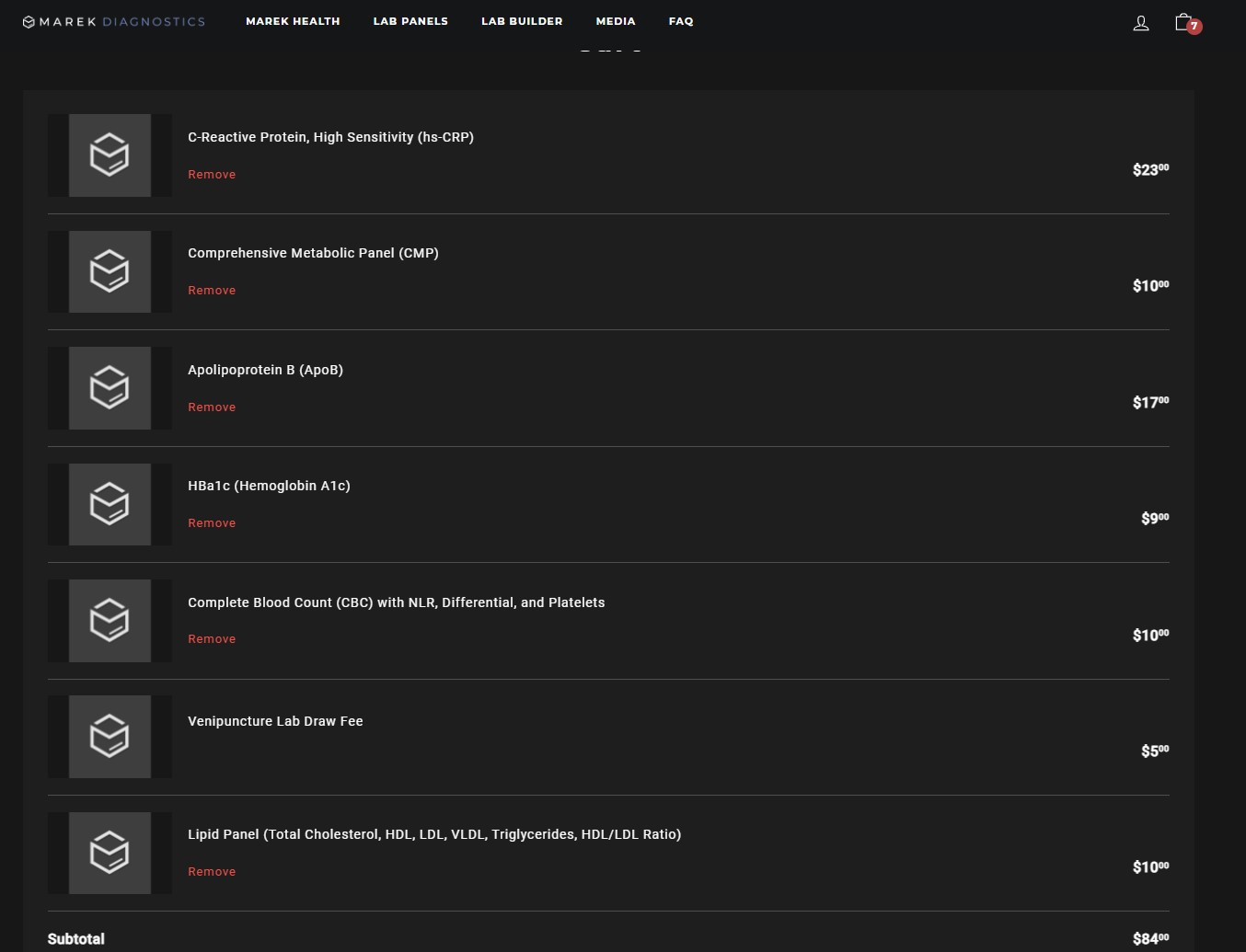
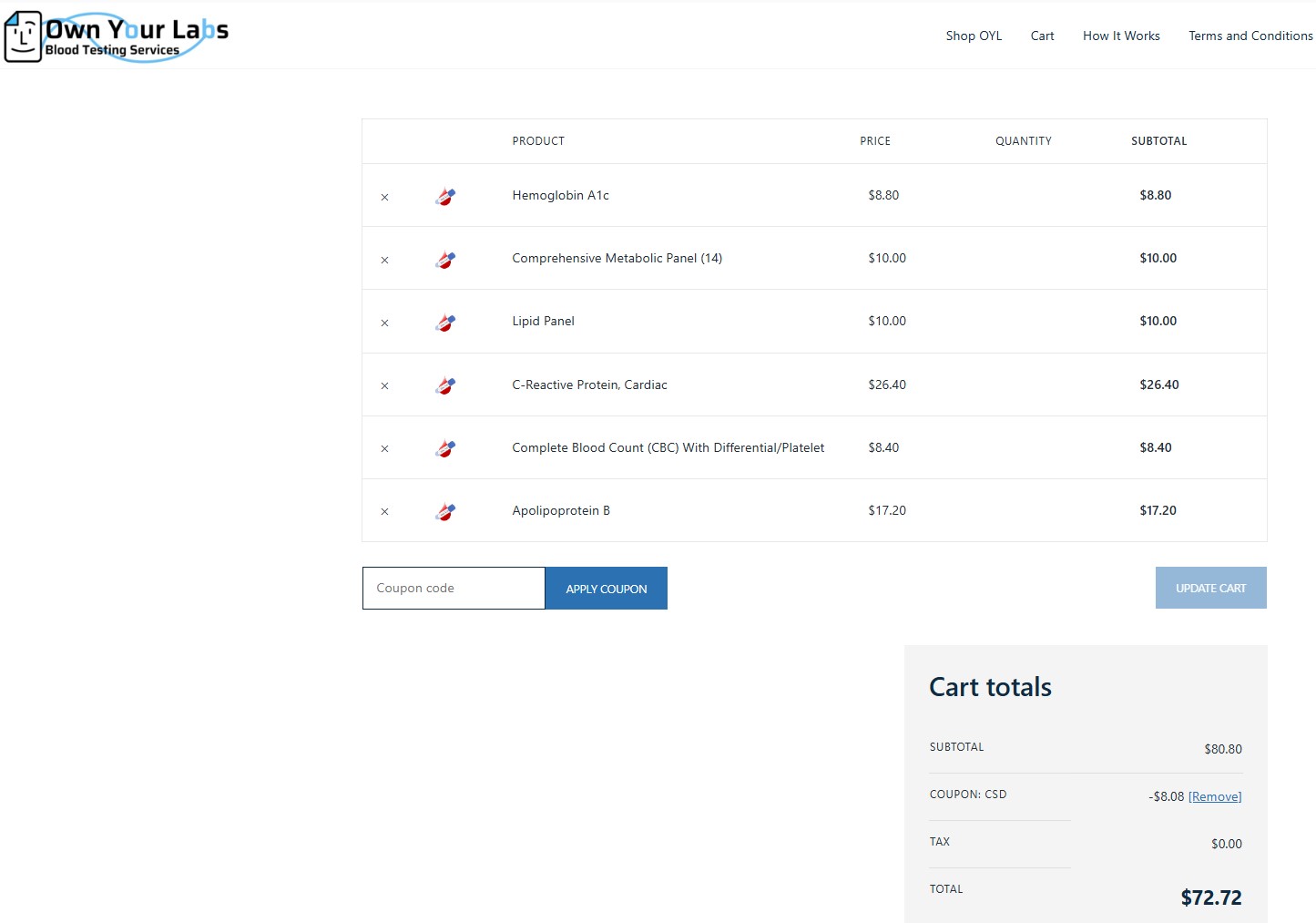
GlycA also is connected to atherosclerosis. Here from Marek Dianostics -(price is reasonable)
Enhanced Lipid Panel (Lipid Panel, ApoB, GlycA, DRI)
Price Regular price $50
GlycAis a novel composite marker of inflammation that reflects enzymatic glycosylation, the process by which sugar attaches to proteins. GlycA reflects the serum concentration and glycosylation state of five major acute-phase inflammatory proteins (a1‐acid glycoprotein, haptoglobin, a1‐antitrypsin, a1‐antichymotrypsin, and transferrin).
The big question is what are these other markers telling you that HsCRP isn’t? and how is it actionable? Certainly a direct head to head comparison of all these markers would be useful. I’ll continue to investigate - Like when would IL-6 tell you more than HsCRP?