Hi Alex!
Did you ever get a GlycoCheck scan? I saw a preventive cardiologist who wants me to buy this test from him. I’d be eager to hear your experience if you care to share.
I don’t see
studies on their website correlating their “Microvascular Health Score” with actual biomarkers of endothelial health.
There’s also the issue of inter- and intra-observer variability and reproducibility.
Still, I’m curious to give it a try. Should I?
Kindly,
Amy
I would love to try it but don’t know where to get it. A4M didn’t have it last year.
Very interesting videos and technology. Thanks for posting. Looks like an excellent measure of endothelial health.
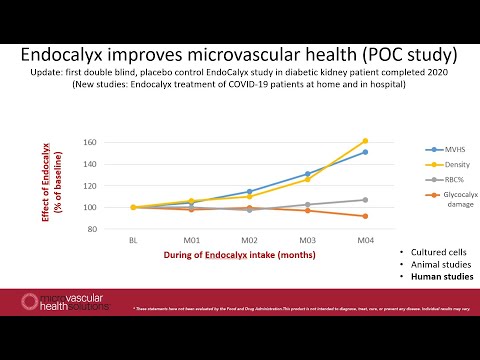
it’s an interesting area and I did have one person tell me it helped them out for their condition but it’s expensive stuff, and the research, supplements, and everything seems closely tied to one group so it’s hard to see it as something easy to trust. There are 9 pages of studies on their site, with only some being directly relevant to their products and I found one Effect of glycocalyx-targeted therapy on vascular function in older adults: a randomized controlled trial | Journal of Applied Physiology to go through (I don’t want to go through them all) It found the following: Our pilot study suggests that Endocalyx Pro supplementation is feasible in older adults but has no measurable effect on overall glycocalyx thickness and FMD. However, Endocalyx Pro may have select effects on capillary glycocalyx thickness and FMD normalized to shear rate among older adults, but further investigation is warranted.
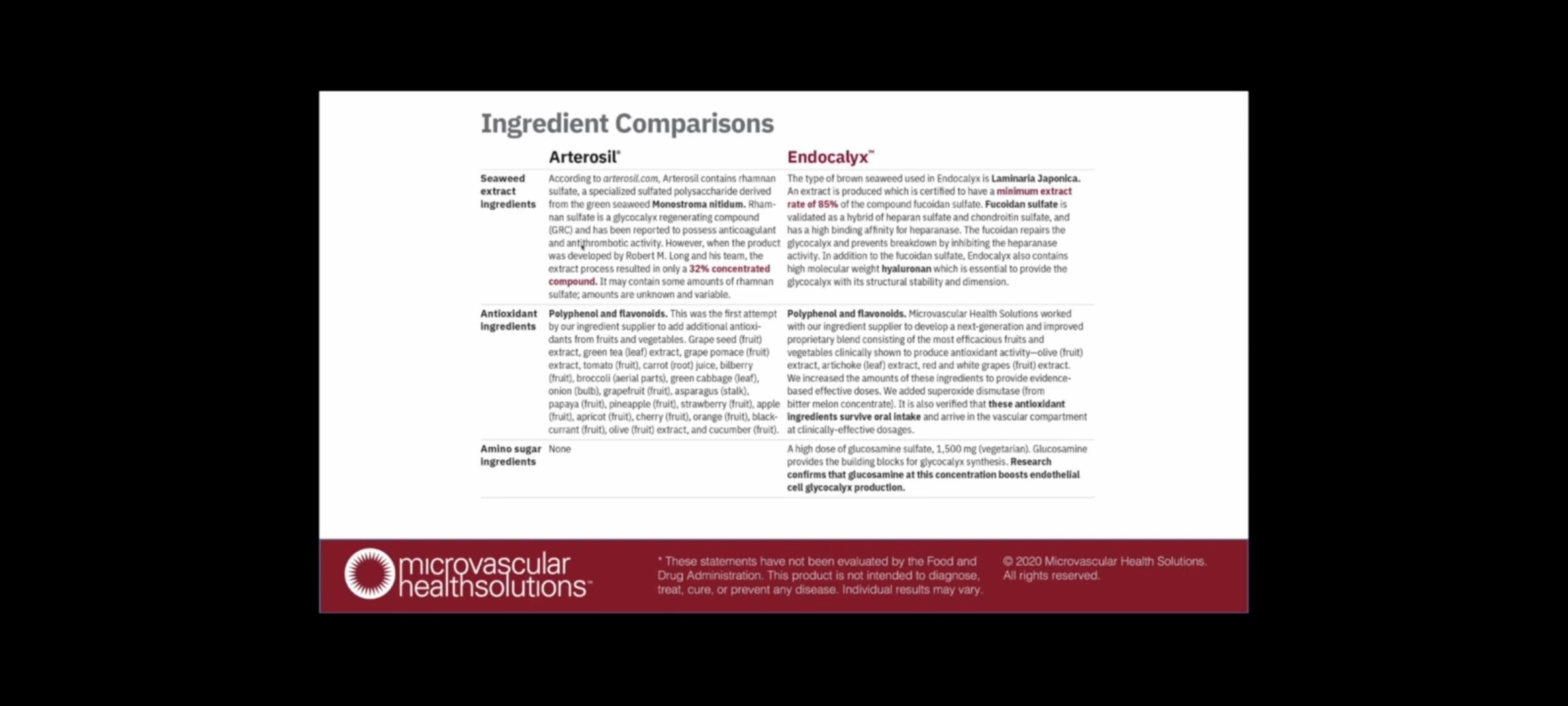
There is a product with similar claims called Arterisol by Calroy - can buy on Amazon or their website
Here is a comparisson of Endocalyx and Arterosil
Supplement I take for blood vessel support and glycocalyx maintenance.
Arterisol is recommended by Dr Twyman a cardiologist who I interviewed this year.
It contains
MonitumRS™ Green Seaweed Extract, Grape Skin And Seed Extract, Green Tea Extract, Grape Pomace Extract, Tomato, Carrot Juice, Bilberry, Broccoli, Green Cabbage, Onion, Garlic, Grapefruit, Asparagus, Papaya, Pineapple, Strawberry, Apple, Apricot, Cherry, Orange, Blackcurrant, Olive Extract, Cucumber
My doctor measured my glycocalyx function a couple of years ago using an EndoPat machine. It found my endothelial function score to be subnormal. He recommended Arterosil.
I have used Arterosil ever since and made impressive improvements in my endopat score, which is now normal.
However, because I use so many products, I can’t necessarily attribute the results entirely to arterosil.
Would be interesting to see a direct comparison between the GlycoCheck and the EndoPAT tests.
Here’s an article looking at different methods that include EndoPAT but not GlycoCheck:
New Noninvasive Methods to Evaluate Microvascular Structure and Function
https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.121.17954
canthe Glycocalyx recover from blood sugar and AGE damage (as long as you don’t get repeated days of it)
ChatGPT said:
Thought for 1m 0s
Short answer: usually, yes. The endothelial glycocalyx can bounce back after a single rough day of high glucose, but it’s slow and fragile. Repeated spikes stringed together are what really grind it down.
Here’s the useful version:
- Recovery window. After an acute hit, animal data show the layer can rebuild itself in roughly 5–7 days if the insult doesn’t keep repeating. That’s not instant, but it’s not permanent doom either. PubMed Central+1
- What damages it fast. Even one hyperglycemic clamp in healthy humans causes measurable shedding and endothelial dysfunction. That’s been shown directly. PubMed+1
- AGEs are the sticky part. AGEs and RAGE signaling push chronic inflammation and enzymatic “shaving” of the glycocalyx. That damage is more stubborn and accumulates if high-glucose days repeat. BioMed Central
What helps it recover (and stay recovered):
- Avoid repeat spikes for about a week. Give the layer space to regrow; that 5–7 day window is your ballpark. PubMed Central
- Keep oxidative stress down. Antioxidant support can blunt hyperglycemia-induced injury in experiments; vitamin C/N-acetylcysteine have signals here, but think “adjunct,” not miracle. MDPI+1
- Exercise and flow. Healthy shear stress is a pro-glycocalyx signal; it’s part of how vessels maintain NO signaling and barrier function. Semantic Scholar
- Medication effects. In people with diabetes, SGLT2 inhibitors show vascular benefits and appear to help preserve the glycocalyx. Sulodexide (a heparan/dermatan sulfate mix, not approved everywhere) has evidence for promoting glycocalyx reconstruction. Discuss either with a clinician; they’re not over-the-counter toys. SpringerLink+3PubMed Central+3Physiology Journals+3
- Diet basics. Fewer post-meal glucose spikes and lower dietary AGE load help the environment the glycocalyx lives in; Mediterranean-style patterns and omega-3s are reasonable bets. MDPI
- Watch the sodium. High-salt patterns have been linked to worse microcirculation and glycocalyx properties. Physiology Journals
Bottom line: one bad day won’t wreck your glycocalyx forever, but a run of bad days will. If you avoid back-to-back spikes, the layer can rebuild over days; if you don’t, AGEs and inflammatory signaling make the damage more persistent and harder to reverse. You don’t need perfection, just stop giving your endothelium serial cliff dives. If you’re dealing with diabetes or frequent spikes, loop in your clinician about SGLT2i or other strategies while you dial in post-meal control. PubMed+2PubMed Central+2
You said:
can the glycocalyx absorb damage that would otherwise damage the endothelial cells (and more irreversible forms of it)
ChatGPT said:
Thought for 41s
Short answer: yes, but only up to a point. The endothelial glycocalyx is basically the vessel wall’s sacrificial shag rug. It takes the first hit so the actual endothelial cells don’t have to. If the hits are mild and not constant, you lose some rug fibers, then grow them back. Keep stomping on it, and you rip through to the floorboards.
What “absorbing damage” looks like in real biology:
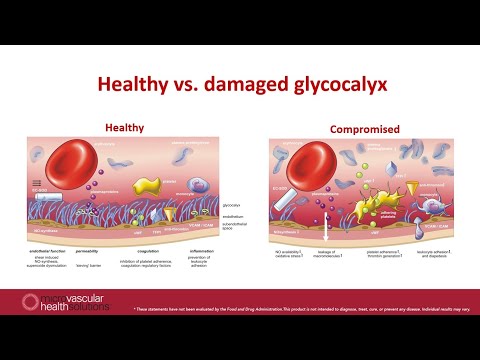
- Physical and chemical buffering. The glycocalyx blunts shear stress, screens the membrane, and limits charged gunk from sticking to the cell surface. Strip it away and leukocyte/platelet sticking and permeability shoot up. That protective “front line” role is well described. PubMed Central+2PubMed Central+2
- Antioxidant docking. Extracellular superoxide dismutase (EC-SOD) parks on heparan-sulfate in the glycocalyx, putting antioxidant activity right at the interface. Lose the GAGs and you lose that shield. AHA Journals+3AHA Journals+3PubMed+3
- Sacrificial shedding. Under hyperglycemia, sepsis, ischemia-reperfusion and similar insults, enzymes shave off syndecans, heparan sulfate and hyaluronan. That shedding can occur before overt endothelial injury, acting as a buffer. When shedding is limited or reversed, downstream endothelial damage is reduced. BioMed Central+2Frontiers+2
- When the buffer fails. If the aggression is intense or repeated, you progress from “shaved glycocalyx” to junctional disruption, impaired NO signaling, and true endothelial injury or death. Clinical and animal data show markers of deeper cell damage (like soluble thrombomodulin) rise once you’re past the glycocalyx’s buffer capacity. BioMed Central
Evidence that protecting or rebuilding the rug helps:
- Mechanistic reviews: The glycocalyx functions as a permeability barrier and mechanotransducer that preserves endothelial integrity. PubMed Central+1
- Intervention data: Rebuilding the glycocalyx with agents like sulodexide restores barrier function, reduces inflammatory signaling, and improves microvascular outcomes in models of hyperglycemia, sepsis, and retinal endothelium. That’s consistent with the idea that the glycocalyx takes the hit so cells don’t. Nature+3PubMed Central+3PubMed Central+3
Bottom line: the glycocalyx can indeed soak up a lot of the damage that would otherwise land on the endothelial cells, and it can regrow after limited hits. But it isn’t adamantium. Space out the insults and it shields you; stack them, and you burn through to more irreversible endothelial injury. Frontiers+1
You said:
can glycocalyx help maintain membrane barrier integrity from microplastics
ChatGPT said:
Thought for 1m 0s
Short answer: yes, when it’s healthy the endothelial glycocalyx is the velvet rope that keeps plastic riffraff off the cell membrane. But if exposure is heavy or repeated, that rope gets shredded and the bouncers go on break.
Here’s the non-cute version:
- Barrier first, cells second. An intact glycocalyx is a charge- and size-selective filter that reduces particle contact and uptake. Degrade it and endothelial uptake of nanoparticles jumps several-fold. That’s been shown directly. PubMed Central+1
- Micro/nanoplastics don’t play nice. PET and polystyrene particles can trigger glycocalyx loss via ER-stress and ROS, then push permeability and inflammation up. Once the glycocalyx is shaved, the membrane and junctions get the full blast. BioRxiv+2PubMed Central+2
Net: a robust glycocalyx does help maintain membrane barrier integrity against microplastics, mainly by electrostatic screening and spacing the particles away from the lipid bilayer. But microplastics, especially the nano crowd, can damage the glycocalyx itself; after that, the barrier effect collapses and the cells start losing tightness and composure like a budget umbrella in a wind tunnel. PubMed Central+2BioRxiv+2
If you want the practical takeaway without the lecture: protect the glycocalyx or everything downstream pays the bill. Keep it intact and it buys you time; let it erode and microplastics get much closer, much faster. PubMed Central
You said:
"We believe delving into the PHB-HBP axis as a ‘Saboteur Factory’ of initial cellular hardware failure could reveal how glucose overload drives aberrant prohibitin O-GlcNAcylation and epigenetic reprogramming, ultimately leading to glycocalyx collapse and systemic metabolic dysfunction. " explain
ChatGPT said:
Thought for 37s
Here’s the translation from sci-poetry to biology, with fewer capes and more enzymes:
What the sentence is claiming
“PHB-HBP axis = Saboteur Factory” means:
- HBP (hexosamine biosynthetic pathway) is the glucose side-route that turns a slice of incoming sugar into UDP-GlcNAc, the donor used for O-GlcNAcylation (a reversible “sugar tag” slapped onto proteins inside the cell).
- PHB (prohibitin 1/2) are scaffold proteins that stabilize mitochondrial membranes, help assemble respiratory complexes, and moonlight in the nucleus as co-regulators.
- When glucose is high, HBP flux rises, O-GlcNAcylation spreads, and if PHB gets aberrantly O-GlcNAcylated, its mitochondrial and nuclear jobs go sideways. That screws with energy, redox, and gene programs.
- Those shifts push endothelial cells toward glycocalyx loss and leaky, inflamed vessels, which then feeds into systemic metabolic dysfunction.
The step-by-step chain
- Glucose overload → more HBP flux.
GFAT pulls glucose and glutamine into UDP-GlcNAc. When this pool swells, lots of proteins get extra O-GlcNAc tags.- PHB gets mis-tagged.
Prohibitin’s O-GlcNAcylation can alter its interactions with mitochondrial proteases and respiratory complexes. Translation: wobblier mitochondria, more electron leak, more ROS, and less clean ATP per glucose molecule.- Mito-nuclear crosstalk flips.
PHB also works with transcription machinery. When its post-translational marks change, you get epigenetic reprogramming: O-GlcNAc also modifies histones, DNMT1, TETs, and TFs like Sp1 and NF-κB. Net effect is a gene-expression tilt toward inflammation, ER stress, and sheddase activity.- Endothelial phenotype shifts.
High O-GlcNAc and ROS suppress eNOS/NO signaling and KLF2/KLF4 flow-protective programs. You see more heparanase, MMPs, ADAMs, and hyaluronidases that literally shave the glycocalyx; and less expression of core proteoglycans (syndecans, glypicans) and GAG-chain enzymes (EXTs, NDSTs, HAS2).- Glycocalyx thins, then collapses.
Lose that sugar-brush and you lose charge-selective filtering, mechanotransduction, and local antioxidant docking (EC-SOD rides those GAGs). Now leukocytes stick, permeability rises, and microvascular flow regulation tanks.- System-level fallout.
Leaky, inflamed endothelium worsens insulin delivery, tissue hypoxia, and organ-level stress signals. That amplifies glucose intolerance. Congratulations, your feedback loop now feeds itself.Why call it a “Saboteur Factory”
Because the HBP doesn’t just respond to glucose; it manufactures the post-translational edits that quietly derail both mitochondrial hardware (via PHB) and nuclear software (via chromatin/TF O-GlcNAc). The output is a phenotype that self-perpetuates endothelial dysfunction and glycocalyx loss. Subtle, sneaky, annoyingly effective.
Testable predictions if this model is right
- Biomarkers: higher circulating syndecan-1 or heparan-sulfate fragments; reduced RBC/retinal glycocalyx thickness proxies; elevated heparanase; lower flow-mediated dilation; rising cell-free mtDNA.
- Molecular readouts: increased global O-GlcNAc, with PHB O-GlcNAc detectable by IP/lectin blot; suppressed KLF2 target genes; reduced eNOS Ser1177 phosphorylation.
- Interventions that help: anything that lowers post-prandial glucose peaks or HBP flux should improve glycocalyx measures and endothelial NO within days to weeks.
Where the levers probably are
- Reduce glucose spikes so HBP isn’t bathing everything in UDP-GlcNAc.
- Restore flow signaling: exercise that raises laminar shear boosts KLF2/KLF4 and eNOS, which are pro-glycocalyx.
- Mito protection: tamp ROS and keep PHB-dependent complexes stable; if mitochondria stop screaming, the sheddases calm down.
- Direct glycocalyx support: curb heparanase/MMP activity and rebuild GAGs/proteoglycans; you know the usual suspects from the endothelial literature.
One-line TL;DR
Too much glucose pushes the HBP to over-O-GlcNAcylate prohibitin, which scrambles mitochondrial output and gene programs, tipping endothelial cells into a glycocalyx-shedding, low-NO, high-inflammation state that spirals into whole-body metabolic trouble. Neat in theory, brutal in practice.
You said:
is glycanage an indirect measure of sialyation at glycocalyx
ChatGPT said:
Thought for 58s
Short answer: no. GlycanAge reads IgG N-glycans in your blood, not the endothelial glycocalyx on your vessel walls. It’s a decent thermometer for immune-system “inflammaging,” but it is not a secret periscope into glycocalyx sialylation. Aging-US+2Frontiers+2
What it actually measures: a composite of IgG glycan features (mainly galactosylation, plus bits of sialylation, fucosylation, bisecting GlcNAc) that shift with age and health. Useful, yes. Glycocalyx-specific, no. Aging-US+1
Why that’s different from the glycocalyx: your glycocalyx is a cell-surface sugar brush made of proteoglycans and glycoproteins whose terminal sialic acids help maintain negative charge and barrier function. Changes there show up as leaky microvessels, altered surface charge, and shed fragments in plasma. That biology is separate from IgG glycosylation. Frontiers+1
If you actually want a read on glycocalyx status, look at:
- Sublingual PBR via sidestream dark-field imaging (higher PBR ≈ thinner glycocalyx). Nature+1
- Shedding markers in blood: syndecan-1, heparan sulfate, hyaluronan. PubMed+1
Bottom line: GlycanAge can hint at your systemic inflammatory milieu, which often co-travels with glycocalyx trouble, but it is not an indirect measure of glycocalyx sialylation. Different compartment, different molecules, different story. If you want the vessel sugar-coat report card, use PBR and shedding markers, not an antibody glycome clock.
Where did you see this?
This is my concept.
And there is more.
Related Article:
Highlights
- Treating old mice with [Endocalyx] containing HMW-HA for 10 weeks increased the thickness of the glycocalyx, a layer of carbohydrates on the outer surface of many cells.
- Old mice given the HMW-HA supplement also exhibited lower frailty, as measured with an assessment of spinal curvature.
- Moreover, HMW-HA-supplemented old mice displayed an improved maximal exercise capacity, as measured with running time to exhaustion.