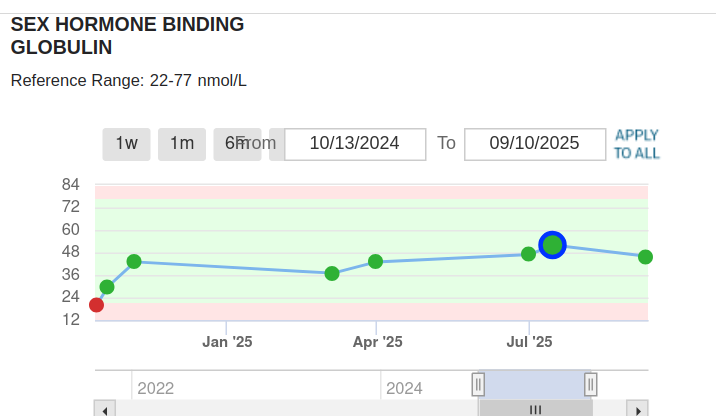
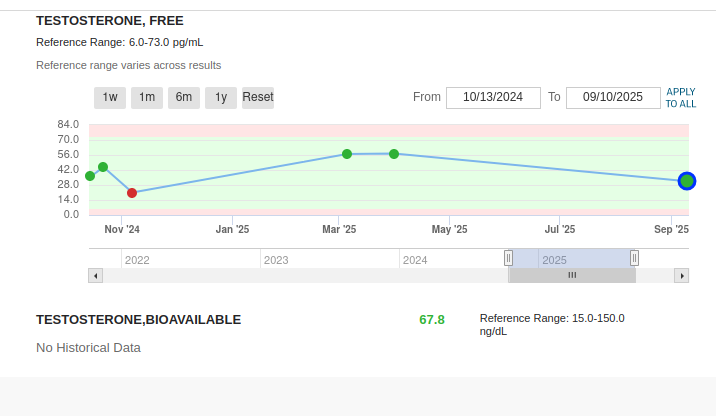
40% increase in chance to 90th percentile (Top 10%) for either SHBG or Estradiol
70% chance for SHBG to 99th percentile (Top 1%).
This is in females. What could be the mechanism of action? Could it be similar in males? Calorie restriction increases SHBG?
Also: this is a human study… not mice.
Great journal: Cell Medicine
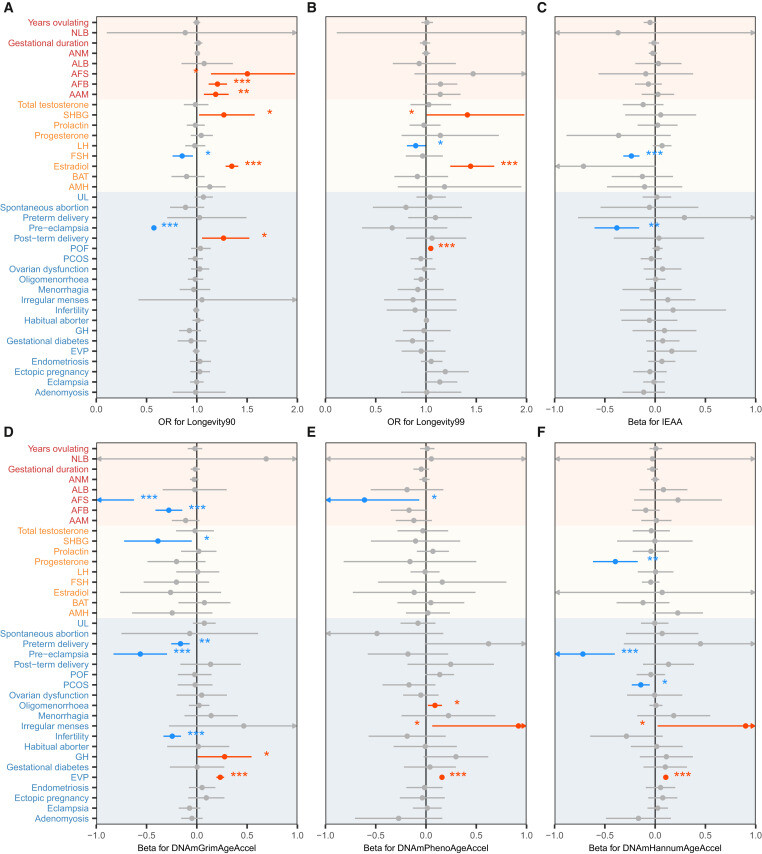
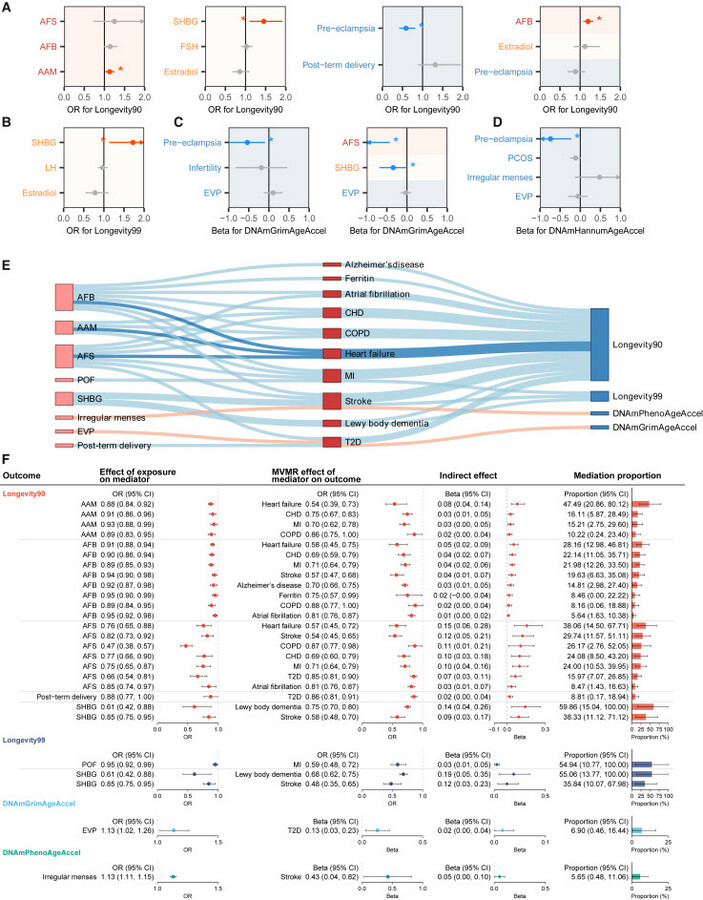
In this comprehensive study, we found that genetically determined later reproductive events, such as older AFB, AFS, and AAM, as well as elevated estradiol and SHBG levels, were causally associated with increased longevity and decelerated biological aging.
Genetically determined per year increase in age at first birth (AFB) (inverse-variance weighted [IVW]-estimated odds ratio [OR], 1.21; 95% confidence interval [CI], 1.12 to 1.30; p = 1.28 × 10−6) and per log-transformed unit increase in estradiol levels (OR, 1.35; 95% CI, 1.29 to 1.41; p = 4.02 × 10−36) were causally associated with higher odds of achieving 90th percentile longevity, both results remaining significant at the phenotype-adjusted Bonferroni threshold (p value < 2.25 × 10−4, Figure 2A). Conversely, genetic liability to pre-eclampsia was strongly associated with lower odds of reaching 90th percentile longevity. Genetically predicted older age at first sexual intercourse (AFS), AAM, and elevated sex hormone-binding globulin (SHBG) levels were suggestively associated with increased odds of achieving 90th percentile longevity, while genetically predicted levels of follicle-stimulating hormone (FSH) had the opposite effect (nominally significant, p < 0.05). However, reproductive behaviors were not significantly associated with 99th percentile longevity. For this extreme aging measure, genetically predicted levels of estradiol** (OR, 1.44; 1.24 to 1.68; p = 1.84 × 10−6) and SHBG (OR, 1.41; 1.01 to 1.98; p = 0.045) maintained positive effects
Genetically predicted SHBG levels remained positively related with higher odds of both the 90th (1.45; 1.10 to 1.92; p = 9.79 × 10−3) (Figure 3A) and 99th (1.72; 1.13 to 2.62; p = 1.11 × 10−2) (Figure 3B) percentile longevity following the respective adjustments.
Among cardiovascular diseases, heart failure mediated the largest proportion of the association between AFB and 90th percentile longevity (28.16%; 95% CI, 12.98%–46.81%), followed by coronary heart disease (CHD), myocardial infarction (MI), stroke, and atrial fibrillation. Alzheimer’s disease (14.81%; 95% CI, 2.98%–27.40%) and chronic obstructive pulmonary disease (COPD) (8.16%; 95% CI, 0.06%–18.88%) were also significant mediators. Ferritin, associated with trace element disorders, accounted for 8.46% of the association. Heart failure also mediated a significant proportion of the association between AFS and longevity (38.06%; 95% CI, 14.50%–67.71%). Other diseases, including atrial fibrillation, type 2 diabetes (T2D), MI, CHD, COPD, and stroke, mediated 8.47%–29.74% of the total effect, with T2D and stroke additionally mediating the association between AFS and DNAm-based biological age acceleration. For AAM, heart failure mediated the largest proportion of its association with 90th percentile longevity, followed by CHD, MI, and COPD. Regarding reproductive hormones, the association between SHBG and 90th/99th percentile longevity was mediated primarily by stroke and Lewy body dementia, accounting for 35.84%–59.86% of the total effects. Lung diseases—such as COPD, lung cancer, lung adenocarcinoma, and lung squamous cell carcinoma—primarily mediated the associations between AFB, AFS, preterm delivery, and DNAm-based biological age acceleration, accounting for 11.88%–44.07% of the total effect. The mediators of the relationships between primary ovarian failure, irregular menses, EVP, post-term delivery, and aging phenotypes were MI, stroke, and T2D
https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(25)00554-3