So - I looked up this study that was referenced in the previous paper, and it seems far to short a study , for an acute situation, to conclude (as the previous paper did) that “these [many] benefits [of rapamycin use] were not translatable to humans, as shown in the CLEVER-ACS trial where mTORC1 inhibition using the rapalog everolimus failed to improve outcomes in patients with myocardial infarction.”
Controlled-Level EVERolimus in Acute Coronary Syndrome (CLEVER-ACS) - A phase II, randomized, double-blind, multi-center, placebo-controlled trial
AI SUMMARY:
Here’s a structured summary, novelty identification, and critique of the uploaded paper:
 Summary
Summary
Title: Controlled-Level EVERolimus in Acute Coronary Syndrome (CLEVER-ACS) – A phase II randomized, double-blind, multi-center, placebo-controlled trial (American Heart Journal, 2022).
Background:
- Acute myocardial infarction (AMI) triggers strong inflammatory responses that worsen infarct size and left ventricular (LV) remodeling.
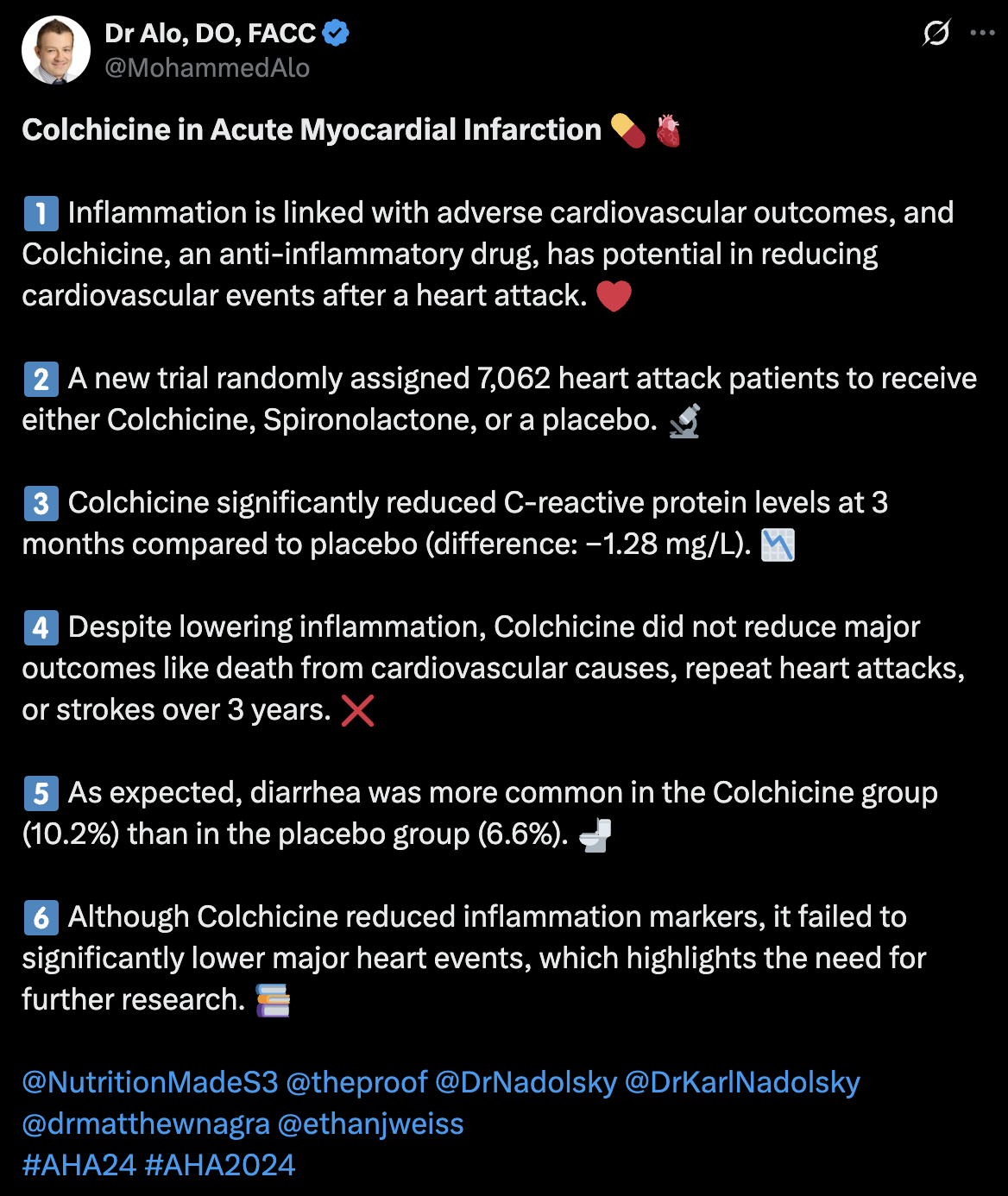
- Prior anti-inflammatory approaches (e.g., canakinumab in CANTOS, colchicine in COLCOT) have shown reduced cardiovascular events but mixed results for infarct size.
- Everolimus, an mTOR inhibitor, has broad immunosuppressive effects on innate and adaptive immunity and reduces infarct size in preclinical models.
Objective:
To test whether a short 5-day course of oral everolimus after ST-elevation myocardial infarction (STEMI) treated with primary PCI can reduce infarct size, LV remodeling, and inflammation compared with placebo.
The CLEVER-ACS trial used a short 5-day oral regimen of everolimus:
-
Days 1–3: 7.5 mg once daily
-
Days 4–5: 5.0 mg once daily
So patients received a tapered schedule (7.5 → 5 mg qd), designed to give strong inhibition during the early inflammatory phase and then reduce dose to minimize risks of prolonged immunosuppression
 Novelty
Novelty
-
First RCT using systemic mTOR inhibition in acute STEMI: Previous uses of mTOR inhibitors were mainly in transplantation and stents; this is the first to test short-term systemic oral everolimus in the acute MI setting.
-
Broad-spectrum immunomodulation approach: Unlike IL-1β or colchicine (targeted interventions), everolimus suppresses multiple immune pathways simultaneously, which may provide a stronger anti-inflammatory impact.
-
Integration of advanced imaging and biomarkers: The trial uses serial cardiac MRI for precise infarct size quantification plus a biobank of inflammatory markers, offering mechanistic insight into immune modulation.
-
Short, tapered regimen: A 5-day high-dose-to-lower-dose schedule is designed to capture early inflammation but minimize prolonged immunosuppression.
-
Bridging preclinical and human translation: Builds directly on animal data showing infarct size reduction with mTOR inhibition.
 Critique
Critique
Strengths:
-
Rigorous design: Phase II, randomized, placebo-controlled, double-blind, multi-center with independent DSMB and adjudication.
-
State-of-the-art endpoint: Use of cardiac MRI, gold standard for infarct size and LV remodeling.
-
Mechanistic depth: Biomarker profiling and immune cell analysis increase translational value beyond clinical outcomes.
-
Practical dosing: The short regimen reduces risks associated with long-term immunosuppression.
Limitations / Concerns:
-
Timing of intervention:
- Everolimus is oral only; initiation is delayed (up to 5 days after reperfusion).
- The most intense inflammatory phase occurs within the first 24–72 hours post-MI; late administration may miss this critical window.
-
Sample size & power:
- n=150 is modest and powered for infarct size change, not clinical outcomes.
- May be underpowered to detect subtle effects or safety signals.
-
Short follow-up (30 days):
- Remodeling and heart failure development often evolve over months.
- The design does not assess medium/long-term functional or clinical benefits.
-
Safety considerations:
- Even short mTOR inhibition may impair wound healing, infection defense, or cause cytopenias, especially in acutely ill patients.
- Immunosuppression in STEMI patients could have unforeseen risks (though prior sirolimus/everolimus trials in PCI show low side effects).
-
Comparator limitations:
- The placebo-controlled design is appropriate, but comparison to other anti-inflammatories (colchicine, IL-1 inhibitors) could provide more context on relative benefit.
 Overall Assessment
Overall Assessment
The CLEVER-ACS trial is an innovative and ambitious translational study, testing whether short-course systemic mTOR inhibition can reduce infarct size in STEMI patients. Its novelty lies in the broad-spectrum immunomodulatory approach, robust imaging endpoints, and translational biomarker work.
However, it faces practical limitations: modest sample size, late start of therapy relative to peak inflammation, and short follow-up. Even if positive, the findings would primarily justify a larger phase III trial rather than changing clinical practice.
Interpretation & Implications
Given the negative (null) primary and key secondary results, here are some considerations and caveats:
- Lack of efficacy vs negative result
- The trial failed to demonstrate a benefit of everolimus in reducing infarct size or MVO in this clinical setting.
- This suggests that either the hypothesis (that mTOR inhibition mitigates post-MI inflammation in a meaningful way) was incorrect, or that aspects of trial design (timing, dose, patient selection) limited the ability to detect an effect.
- Window of inflammation & timing
- Much of the injurious inflammatory cascade post-MI occurs very early (hours to 1–2 days). Because the intervention began within up to 5 days post-PCI, it may have missed the optimal therapeutic window.
- Even though “baseline” CMR was defined between 12 h and 5 days post-PCI, the modulation of inflammation may have been too late to alter infarct evolution.
- Dose, duration, and tissue penetration
- It’s possible the used dose and duration were insufficient to meaningfully suppress relevant inflammatory pathways in the myocardium (or in recruited leukocytes) without causing unacceptable systemic immunosuppression.
- Tissue-level drug delivery in infarcted myocardium, where perfusion is compromised, might have been suboptimal.