My hsCRP has gone from 0.9 to 0.26 in the past two years. I’m thinking the key things I’ve changed during that time is adding ezetimibe and Ashwagandha (if the first post in this thread is accurate).
Yes. Mine has declined similarly but over a 3-4 year period. However, I have made so many changes that it is no longer possible to assign attributions. I also think doing so doesn’t make sense at some point. It seems likely that many interventions will lower baseline inflammation, and by a significant amount but each succeeding addition lowers it less in absolute terms even though the percent change may be similar. Austin’s law of diminishing fleas or something like that I think.
The population data suggests it is worth following up on if ASCVD is a concern on one’s overall profile.
The frequency of HNF1A variants associated with lower CRP and increased cardiovascular disease (CVD) risk varies by population and specific allele.
1. rs1169288 (HNF1A-I27L, A allele)
- Global Frequency: ~25-35%
- European ancestry: ~27-30%
- East Asian ancestry: ~30-40%
- African ancestry: ~15-20%
This variant has been linked to lower CRP, increased triglycerides, and a higher risk of type 2 diabetes and ASCVD.
2. rs1800574 (HNF1A-S487N, T allele)
- Global Frequency: ~5-10%
- European ancestry: ~7-10%
- East Asian ancestry: ~5-7%
- African ancestry: <5%
This variant has a weaker effect on CRP but is still linked to metabolic dysregulation and cardiovascular risk.
I have a CAC of 950. hsCRP three months ago was .2 at Quest. (So they might have rounded down from .24.) What does this tell me about my CVD ‘risk’?
If the above genetic variant issue is correct, it would depend on whether you are generically in the group of people who test low on CRP but actually have elevated risk. So far as I know, however, all of the knowable ASCVD risk is still subsumed by two markets: Lp(a) and Apo(b). This is likely a “to be continued” issue.
Assessing TNF-α & IL-10 will indicate the broader NF-κB pathway activity. This should give you good indication of the balance between pro- and anti-inflammatory cytokines and provide a crosscheck on your low CRP level.
I haven’t looked at these SNP’s but most complex traits are highly polygenic, with lots of SNP’s, so you have to sum up the effects of all the genes you have that are relevant (+ or -) for a total score or effect:
See this thread:
That’s great. And both were inline with other surrounding datapoint (and not just that you eg had an infection close to the first test but not second test)?
What else could it have been - did you change visceral fat / overall fat levels? I recall you also changed/increases some of your excessive regime?
Yes - normal health in both cases. I have ramped up my exercise program to about 1 hour +, 4 or 5 times a week. I’ve done this for the past 3 or 4 months - so that might have had an effect.
My CRP fell from 1.6 to 0.25 over a 9-month period. I believe the main contributors were starting ashwagandha 900 mg, quercetin 500 mg, and astaxanthin 24 mg. All of these have some studies reporting CRP lowering benefits.
My CRP actually rose a bit over my first 8 months of rapamycin. So, there hasn’t been any clear sign it is helping in that regard for me, but I am still taking it.
Ezetimibe did nothing to me and research shows it does nothing for hsCRP (the first post was incorrect and I fixed it). So ashwagandha might be the cause. How much do you take? Any thoughts on ashwagandha @John_Hemming?
I personally have tried aswaghandha twice. The first time was well before I really understood what was going on and I did not conclude it helped. The second time it made me ill (one of only two substances to do that the other being PQQ which was probably an interreaction with alcohol).
There is an Indian MD who campaigns against it because it can cause liver disease (which is true).
I don’t understand how it does any good if it does. It may do some good, but as a general principle I recommend against using it. I do maintain an open mind and if there was good evidence to take it then I would consider it.
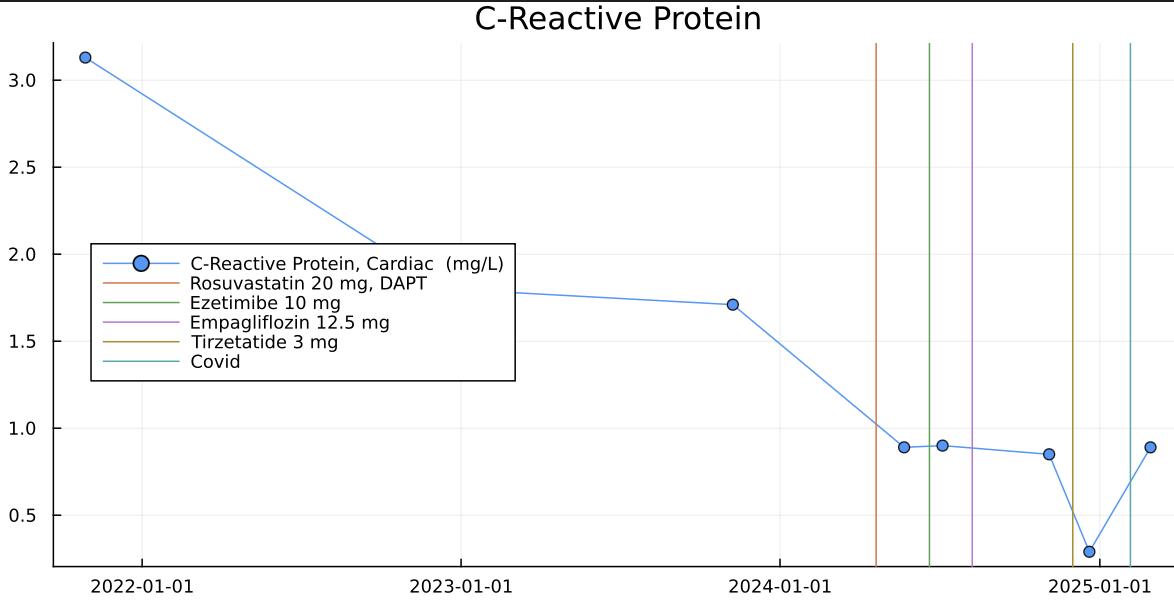
Same for me. My hsCRP was going down slowly but went below 1 with rosuvastatin 20mg.
Ezetimibe and Empagliflozin did not improve that further but Tirzepatide did and at 0.29 it was improved by a factor of more than 10 compared to the bad state I started.
Obviously Covid increased it but it’s still below 1.
I take 2 capsules (1,000mg total) every day of this product: https://www.costco.com/youtheory-ashwagandha-1000-mg%2C-180-vegetarian-capsules.product.4000181013.html
Seems pretty consistent with everything I’ve read… you want a low CRP (under 1.0, and the lower the better), and also low LDL-C / APOB, (lower the better) for low cardio risk.
ChatGPT agrees:
However CRP lowering drug don’t seem to work to lower the risk. The colchicine RCT failed.
I’m taking colchicine as a preventative and just googled after I read your comment.
I am seeing a few sources that conclude it didn’t change outcomes, but then I also read the following… I’d love your thoughts? Just trying to figure out if I should consider going off of it
https://academic.oup.com/eurheartj/article/46/26/2552/8123897#google_vignette
Conclusions
This updated meta-analysis of RCTs demonstrated a substantial reduction in MACE, MI, ischaemic stroke, and recurrent coronary revascularization with colchicine compared with placebo. Therefore, the results support the use of colchicine to reduce recurrent cardiovascular events.
That’s not a particularly good indicator of whether lowering CRP is beneficial or not. Colchicine is a bit of a dirty drug that can do a lot of negative things besides lowering CRP. It disrupts microtubule assembly, which is an important process for many things in the body.
Which RCT trial is that?
From Thomas Dayspring in the comments:
Acute MI is a very different process than use of colchicine in stable chronic CAD where studies have shown it to reduce residual risk …
I don’t like the significant increase in non-CVD related deaths (even though ACM wasn’t significant), in the other trial.
The therapeutic index is very low as well.
So for stable CAD it might’ve not failed, but it’s not a home run.
On the topic of CRP, I think I’ve seen some studies showing a MR relationship of IL-6 and CVD, other than that it’s kind of meh currently, good to keep low mostly for other reasons (mouse aging and association studies in humans), IMO, with a small signal for CVD.