Centenarians—the way to healthy vascular ageing and longevity:
a review from VascAgeNet by Sabrina Summer & Soner Dogan et al.
Open access paper:
AI Summary (CGPT5)
Here is a detailed summary of the paper “Centenarians—the way to healthy vascular ageing and longevity: a review from VascAgeNet” (Summer S. et al., GeroScience 2025, 47: 685-702) – with focus on the vascular ageing / longevity insights you’d expect given your longevity-/health-biomarker orientation.
Paper details and scope
- The review is authored by a large multidisciplinary consortium from the VascAgeNet network, and was published online 27 Dec 2024.
- It focuses on individuals aged 100 years or more (“centenarians”) – and sometimes near- (95-99), semi-super-(>105), or super-centenarians (>110) – but for simplicity they use the term “centenarians” unless stated otherwise.
- The key premise: despite advanced chronological age, many centenarians show relatively preserved vascular structure and function and delayed onset / lower incidence of cardiovascular diseases (CVD). By studying them we may glean mechanisms of “healthy vascular ageing” that support longevity.
- The authors delimit that they will not exhaustively review all cellular-mechanisms of vascular ageing (which exist elsewhere) but rather focus on how intrinsic + extrinsic factors in centenarians may modulate vascular ageing and thus longevity.
Key findings and arguments
Vascular phenotype of centenarians
- The review notes that age-related changes in vasculature (e.g., arterial stiffening, endothelial dysfunction, intima-media thickening, loss of elasticity) are typical in older adults.
- But many centenarians appear to show less severe deterioration: better preserved endothelial function, lower arterial stiffness, lower prevalence or delayed incidence of CVD risk factors and disease outcomes.
- The authors present a table (Table 1) of vascular‐ageing measurements in centenarians (e.g., carotid IMT, adventitial diameter, pulse wave velocity) and highlight that while changes still occur, the rate/extent is reduced compared to typical older cohorts.
- They emphasise that this vascular resilience is likely a composite outcome of multiple protective mechanisms (genetic, immunologic, metabolic, lifestyle) rather than a single “super gene.”
Intrinsic (non-modifiable) factors
These include sex, genetics/epigenetics, and others.
- Sex: Women outnumber men in centenarian cohorts; female sex generally has lower CVD risk, more robust immune responses, and longer average life expectancy.
-
Genetics/epigenetics :
- The offspring of centenarians tend to show better cardiovascular profiles.
- Gene polymorphisms associated with longevity and vascular health are discussed: for example, variants in eNOS (endothelial nitric oxide synthase), endothelin receptor genes, antioxidant enzyme genes (superoxide dismutase, glutathione peroxidase), lipid-metabolism genes (APOE, lipoprotein receptors), IL-6, ACE, KLOTHO, FOXO3A.
- Epigenetic modifications: centenarians show epigenetic profiles more similar to younger adults in some respects (attenuated DNA methylation drift, different miRNA expression, histone modifications).
-
Immune / inflammation profile :
- Centenarians often have lower levels of chronic inflammatory markers (IL-6, CRP) compared to typical older adults.
- They have higher regulatory T-cell (Treg) numbers, shifts in cytokine profiles toward anti-inflammatory states, preserved neutrophil/immune function in some cases.
Extrinsic (modifiable) factors
These include lifestyle, environment, gut microbiome, medication use, etc.
-
Diet / caloric intake :
- Centenarians often adhere to healthier dietary patterns (plant-rich, antioxidant-rich, moderate caloric intake) though there are cultural differences.
- Caloric restriction (CR) evidence is considered: while human data are limited, CR in younger cohorts (e.g., CALERIE trial) showed reductions in ApoB, glycoprotein acetylation, BP, total cholesterol, etc.
- The authors suggest that a lifelong (or long-term) lower caloric load (without malnutrition) may help preserve vascular health via mitochondrial function, reduced oxidative stress, SIRT1 activation, UCP (uncoupling protein) upregulation, etc.
-
Physical activity / exercise :
- Regular physical activity is emphasised as a key modifiable behavior: anecdotes/studies in centenarian cohorts link exercise or higher muscle strength / lung function / fitness with longevity.
- Mechanistically: exercise improves peripheral vascular function, increases capillarization, promotes shear stress → NO (nitric oxide) production, enhances mitochondrial biogenesis via PGC-1α, reduces oxidative stress and inflammation, counters sarcopenia.
-
Gut microbiome :
- Emerging evidence: centenarians have distinct gut microbiota composition (higher biodiversity, enriched Akkermansia, Bifidobacterium, Christensenellaceae) compared to younger old or general elderly.
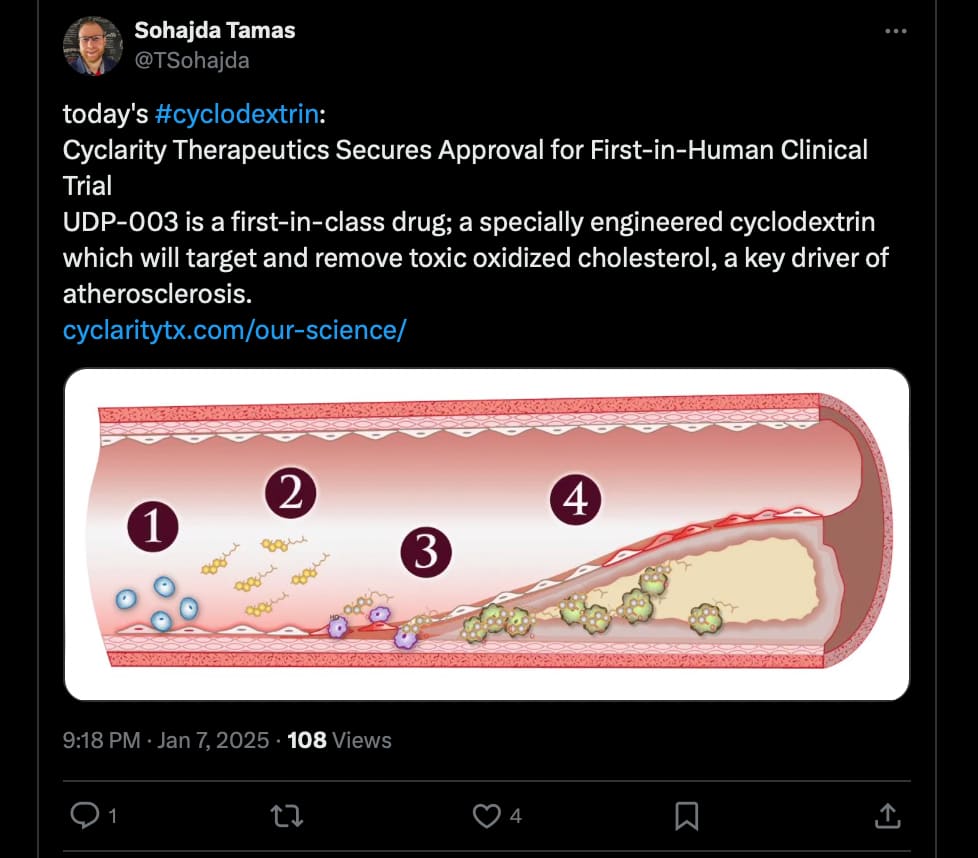
- Gut microbiota influences systemic metabolism, inflammation, and vascular ageing; hence favourable microbiome in centenarians may contribute to preserved vascular health.
-
Medication / medical treatment :
- Paradoxically, some studies show centenarians have lower use of some cardiovascular medications (e.g., antithrombotics, β-blockers, ACE inhibitors) compared to younger old age groups.
- The authors caution that whether this reflects healthier baseline status (fewer treated diseases) or selection bias is unclear.
-
Other lifestyle / environmental factors :
- Socio-economic status, access to healthcare, social network/support, low chronic stress exposures, favourable early-life conditions are also mentioned as contributing to vascular resilience.
Integration: How do these factors merge to promote healthy vascular ageing?
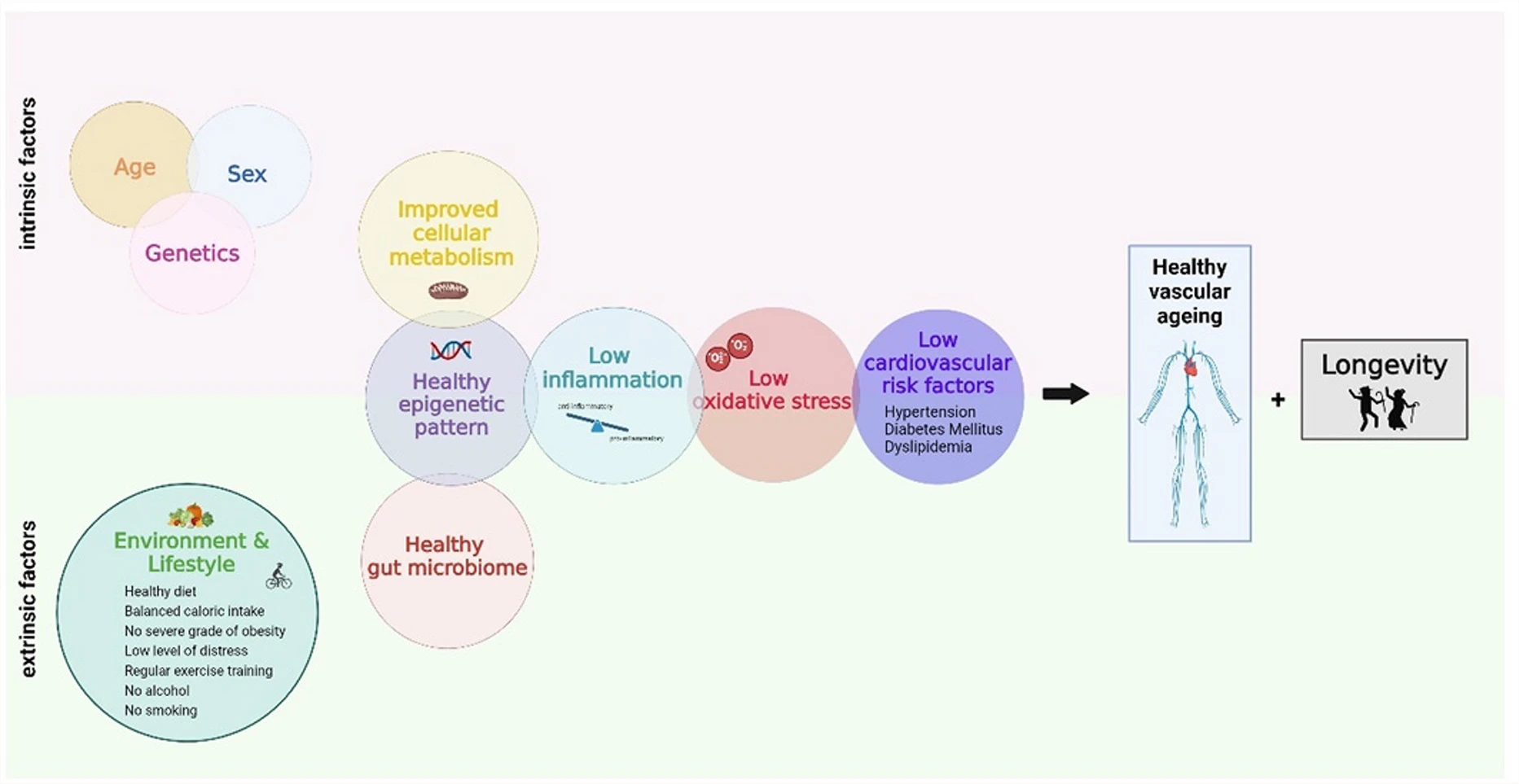
The authors present a schematic (Figure 2) showing how intrinsic + extrinsic factors interrelate to preserve vascular structure/function, delay or mitigate age-related vascular damage, and thereby support longevity.
Specifically:
- Genetic/epigenetic resilience sets a favourable baseline (better antioxidant response, lipid handling, endothelial repair).
- Lifestyle/environment act continuously over decades to maintain vascular health: healthy diet → lower oxidative stress / lipid peroxidation; physical activity → improved endothelial shear stress, capillarization; favourable gut microbiome → lower systemic inflammation.
- Immune ageing (“inflamm-aging”) is blunted or modulated in centenarians; their vascular endothelium remains more reactive and less dysfunctional compared to typical elderly.
- The cumulative effect is a vasculature that ages “slower” (or is better protected) — less stiffening, less atherosclerosis, fewer macrovascular complications — contributing to delayed onset of CVD and longer healthspan.
The authors emphasize that while chronological age is high, biological/vascular age appears “younger” in many centenarians.
Implications for biomarkers & interventions
From your viewpoint (blood biomarkers, longevity interventions), several key implications:
- Vascular ageing metrics (pulse-wave velocity, carotid IMT/adventitial diameter, endothelial function) remain important biomarkers to assess healthspan / mortality risk in extreme ageing.
- Genetic/epigenetic markers identified in centenarians (e.g., variants in FOXO3A, KLOTHO, IL-6 promoter, antioxidant enzymes) could inform risk stratification or identify resilience phenotypes.
- Lifestyle interventions (dietary quality, caloric load modulation, exercise) have mechanistic plausibility for vascular protection; however, the review cautions about translation and the fact that much evidence is observational or indirect (especially in extreme age groups).
- The gut-vascular axis (microbiome → inflammation/metabolism → vascular ageing) emerges as a potentially under-explored target in longevity research.
- The fact that centenarians may require less pharmacologic intervention (or show fewer medications) but still have preserved vascular health suggests a potential for lifestyle/biological resilience rather than purely drug-driven approaches.
Limitations & Future Directions
The authors provide a balanced discussion of limitations:
- Small sample sizes: Studies in centenarians are limited by logistics, fragility of participants, heterogeneity, and attrition.
- Selection bias: Survivors to 100+ years are inherently a highly selected population; results may not generalise to mid-life or younger old.
- Cross-sectional rather than longitudinal: Much data is snapshot rather than tracking vascular trajectories over decades.
- Mechanistic gaps: While many associations exist (genetic variants, microbiome patterns, lifestyle habits), causality and mechanistic pathways remain incompletely defined.
- Biomarker standardisation: The review notes need for standardised measurement of vascular ageing and banking of centenarian‐samples to generate comparative data.
- Sex/gender differences: Under-studied; many centenarian cohorts are female-skewed and sexes may differ in vascular ageing trajectories.
- Future directions suggested include larger consortia, more longitudinal vascular phenotyping in oldest-old, integrating multi-omic data (genetics, epigenetics, microbiome, metabolome) with vascular imaging, and testing whether centenarian‐derived protective mechanisms (e.g., epigenetic signatures) can be leveraged in mid-life interventions.
My critical assessment (relevant to your longevity/biomarker orientation)
- The review is useful because it explicitly links vascular ageing (a key organ‐system dimension) with exceptional longevity, rather than treating longevity in isolation. That aligns with a multi‐system, biomarker-driven longevity framework.
- From a biomarker perspective, I’d highlight the following gaps to flag:
- There is no meta‐analysis of effect sizes (i.e., how much “younger” is the vascular age in centenarians) — the review remains descriptive.
- Given your interest in health‐span optimization, the review suggests but does not quantify which behavioural/lifestyle factors (in adulthood/midlife) are most predictive of vascular resilience in the oldest-old—so there remains a translational gap.
- For entrepreneurial/clinical intervention thinking: one takeaway is that vascular age (e.g., PWV, endothelial function) remains a promising “lever” for longevity intervention. If you build a dashboard with biomarkers, ensuring vascular markers are included is supported by this literature.
- The gut microbiome → vascular link is currently under-explored but seems a promising avenue for next‐generation longevity biomarkers/interventions (prebiotics, microbiome modulation) in relation to vascular health.
- One caution: the centenarian phenotype may reflect resilience rather than prevention of damage (i.e., they may have endured and survived sub‐optimal exposures, rather than been “perfect” lifelong). That means translating findings into younger populations may be non-trivial.