People have made it to 120 without statins or rapamycin. Does that mean we will?
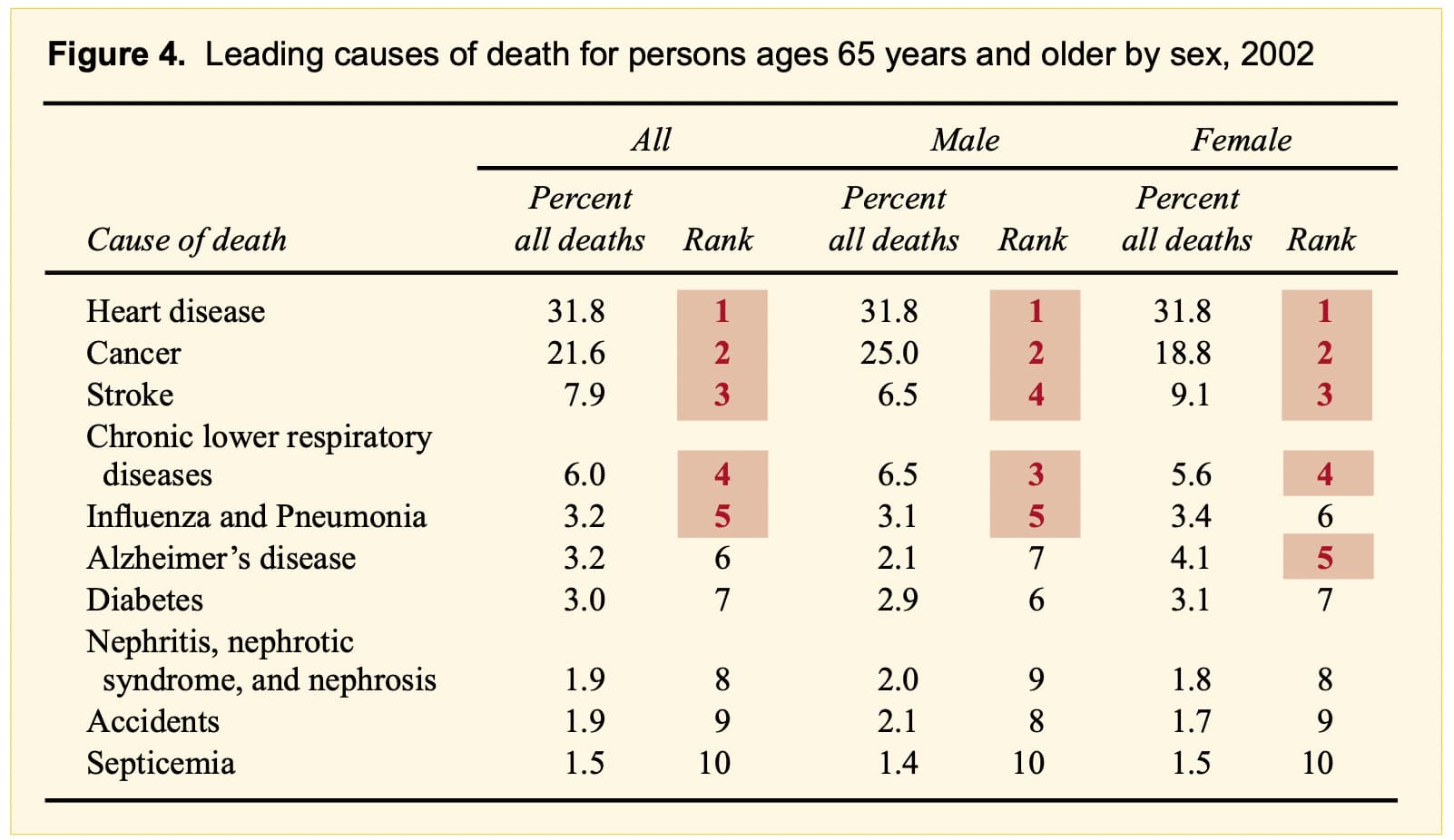
I’m not disagreeing with your data on the GrimAge (or other bioclocks), but how do we reconcile that data, with the fact that “heart disease” is the number one killer:
Source: https://www.cdc.gov/nchs/data/ahcd/agingtrends/06olderpersons.pdf
It may not be a predictor of life span, but it is a predictor of heart disease and stroke.
“Elevated LDL-C level is an independent predictor of atherosclerotic cardiovascular disease. Decreased LDL-C level can reduce the incidence of cardiovascular disease and cardiovascular events such as AMI and ischemic stroke”
One of many, many studies:
Predictive value of LDL/HDL ratio in coronary atherosclerotic heart disease | BMC Cardiovascular Disorders | Full Text.
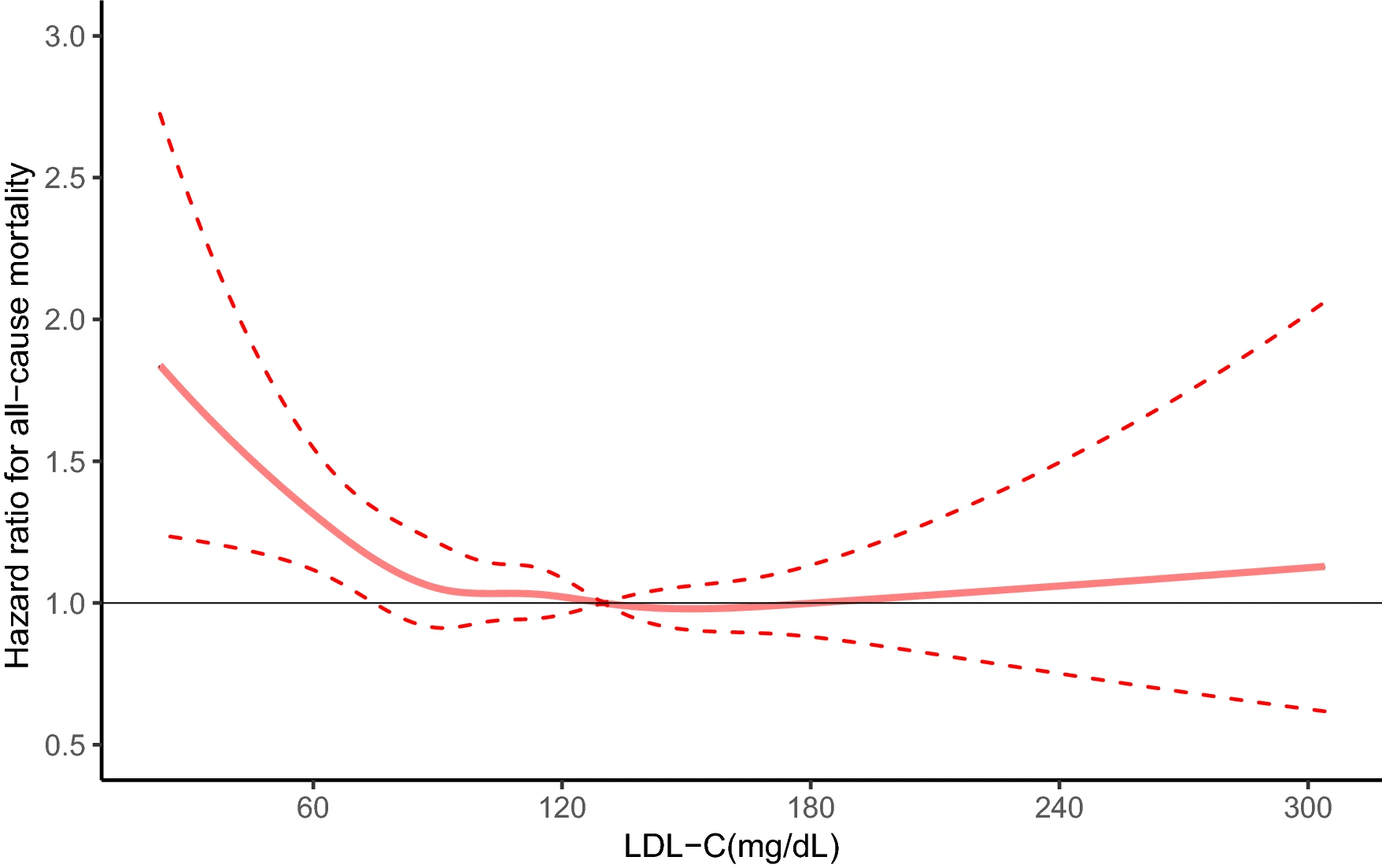
I feel the same and focus more on my glucose levels. Now that you mention your grandparents, there’s some conflicting literature on the optimal LDL level, especially in older adults, that suggests moderate levels may be protective. Association between low density lipoprotein cholesterol and all-cause mortality: results from the NHANES 1999–2014 | Scientific Reports
Overall if I had to guess, I would tend towards lower LDL is better, but given the conflicting results don’t think its a good biomarker to focus on.
Lol the U-shape curve again. ![]()
I just love when new members don’t bother to read the forum before posting.
To be honest - even I stopped reading the Rapamycin and risk of cardiovascular disease thread at about 1,000 posts ![]()
Most people only read a small fraction of the posts on the forum, so we try to direct them to the main past threads when we can.
That’s a good point and question: the heart disease risk may be accounted for in other biomarkers such as glucose and triglyceride, which make the LDL reading redundant when they are all collected together - the table I posted was for the bicorrelations among multiple variables.
But if the only measurement you have is for LDL, it may still be a good predictor of heart disease risk. However if you have the choice of what biomarkers to measure, I think the table suggests it is better to focus on glucose/triglyceride vs LDL
They don’t have to read the entire thread.
Just start from the end read in reverse order. The debunk is strongest there.
I am aware of the controversies regarding this chart and the optimal LDL level in general. As I said, “overall if I had to guess, I would tend towards lower LDL is better”.
Also there is no such thing as “debunking”. There is only conflicting research, the most recent of which suggests lower is better. But the tide can shift the other way in the future as it did before here.
Since we are much closer to the 4.7ppm dose that produces a 3% and 16% median LS increase in males and females respectively (in mice), this seems to suggest female users of rapamycin on this forum may experience much stronger benefits/effects from rapamycin use. I wonder if that is the case in practice? Made me notice there a fewer posts on rapamycin effects by females on this forum.
After half a century of research, it’s become pretty clear that the lower your apoB the better. Whether there is a lower limit or not is unknown, but it’s definitely lower than whatever clinical guidelines recommend today.
Maybe instead of worrying so much about LDL, see it as a marker that you’re messing with mtorc2, and figure out if that’s bad?
Have you ever checked for LADA/ late onset type 1? This can be confused with T2, bc of similar symptoms.
Basically you’re saying to ignore it ![]()
It’s exactly what you said though. Ignore LDL because it increases because of mTOR inhibition and figure out if that’s bad.
It’s called ignoring LDL.
Right now my markers are okay, below the limits of pre-type II diabetes even with rapamycin, so I am not worried about it enough to pursue it.
Hardly. Mtorc2 impacts numerous metabolic processes. It would be narrow minded to simply say that Rapa increases LDL, so we’ll take a statin and all is good. IMO, we should look at an elevated LDL as a marker of mtorc2 synthesis inhibition and decide whether that is important. Now, I may be wrong, maybe LDL elevation is related to mtorc1 inhibition?
No it is not important at all. You increase LDL you will increase your risk of heart disease.
Or I don’t even know what you’re talking about.
Here is a good paper on MTOR inhibition on lipids and glucose. MTORi dosages usually started at 5 or 10 mg daily (for everolimus).
mTOR inhibitors are known to induce dyslipidemia in 25–76% and hyperglycemia in 13–50% of patients [8–10].
In the EXIST trials (follow-up up to 5 years), the phase III trials that led to approval of mTOR inhibition in TSC patients, dyslipidemia was reported in 5–30%, but no new cases of diabetes were reported [3, 4, 6]. In a small prospective study among mainly children with TSC using mTOR inhibition, dyslipidemia and hyperglycemia were reported in 72% and 22% of children, respectively, but the highest fasting glucose did not reach diabetic levels (108 mg/dl (6 mmol/l)) [11].