Part 4: Actionable Intelligence (Deep Retrieval & Validation Mode)
The Translational Protocol (Rigorous Extrapolation)
Note: As this study is a consensus review of lifestyle and systemic factors rather than a pre-clinical trial of a specific novel molecule, the standard “Mouse-to-Human” allometric scaling (HED) is not applicable. Instead, we define the “Behavioral Equivalent Dose” based on the epidemiological data reviewed.
-
Behavioral “Dose” (Weekend Warrior Protocol):
-
Protocol: High-volume, low-frequency aerobic activity.
-
Dose: 1–2 sessions per week.
-
Volume: >150–300 minutes of Moderate-to-Vigorous Physical Activity (MVPA) accumulated within this compressed window.
-
Target: 75–80% Max Heart Rate during vigorous bursts.
-
Efficacy: Associated with a ~25% reduction in mild dementia risk (Hazard Ratio 0.75).
-
Pharmacokinetics (Glymphatic Clearance):
-
Bioavailability (Sleep): The “drug” here is Slow-Wave Sleep (SWS). Glymphatic clearance of amyloid/tau is maximized during SWS.
-
Half-Life: Clearance efficiency drops significantly upon waking.
-
Dosing Window: 7–9 hours nightly. <5 hours acts as a neurotoxin by halting clearance.
-
Safety & Toxicity (Allostatic Load):
-
Toxicity Signal: Allostatic Overload.
-
Markers: Watch for “flatted diurnal cortisol rhythm” (waking with low energy, spiking late) and elevated hs-CRP (>2.0 mg/L) indicating chronic inflammatory load.
-
Liver/Kidney: N/A for behavioral interventions, but monitor Cystatin C if tracking renal function as a proxy for vascular aging.
Biomarker Verification
To verify “Target Engagement” of resilience interventions, track these downstream metrics:
- Biobehavioral Age Gap (BBAG):
-
Metric: Difference between Chronological Age and Phenotypic Age.
-
Testing: Open-source algorithms (PhenoAge/GrimAge) using albumin, creatinine, glucose, CRP, lymphocyte %, MCV, RDW, alkaline phosphatase, and WBC.
- Structural Brain Integrity:
-
Metric: Brain Age Gap via MRI (gray matter volume, hippocampal volume).
-
Target: Brain Age < Chronological Age.
- Autonomic Balance:
-
Metric: rMSSD (Heart Rate Variability).
-
Target: Upward trend in rMSSD (indicating parasympathetic dominance) correlates with reduced allostatic load.
Feasibility & ROI
-
Sourcing:
-
Weekend Warrior: Zero cost. High feasibility for time-poor professionals.
-
Brain Clocks:
-
Blood (PhenoAge): <$100 (standard lab panel). Widely available.
-
MRI (Brain Age): High barrier. Cost ranges from $500–$1,400+ out-of-pocket for “preventative” scans not covered by insurance.
-
Cost vs. Effect:
-
Exercise/Sleep: Near-infinite ROI (free intervention, high impact).
-
MRI Tracking: Low ROI for routine monitoring unless distinct pathology is suspected. Blood-based clocks offer better frequency/cost ratio.
Part 5: The Strategic FAQ (Restructured)
1. The Skeptic’s Inquisition & Analyst Response
Q1: “Is ‘Artificial Wisdom’ just a rebrand of a chatbot, or is there a distinct therapeutic mechanism?”
A: It is currently a conceptual framework, not a deployable product. While standard LLMs optimize for logic and information retrieval, “Artificial Wisdom” systems are theoretically architected to optimize for emotional regulation, prosocial decision-making, and conflict resolution. Early trials (e.g., telephone-based wisdom interventions in Hong Kong) show promise in reducing loneliness, but a dedicated “Wisdom AI” that effectively mimics this without hallucinating is not yet a commercial reality. Treat it as a “future therapeutic class,” not current tech.
Q2: “Can I really cram a week’s worth of cardio into Saturday and get the same neuroprotection as daily training, or is this statistical noise?”
A: The data suggests it is real. The 2024 Mexico City Prospective Study (N=10,033) specifically analyzed mild dementia and found a 25% risk reduction (Hazard Ratio 0.75) for “Weekend Warriors,” which was statistically comparable to regularly active individuals. The mechanism appears to be Total Volume (>150 min/week) driving sufficient glymphatic flow and BDNF release, regardless of whether that volume is compressed or spread out.
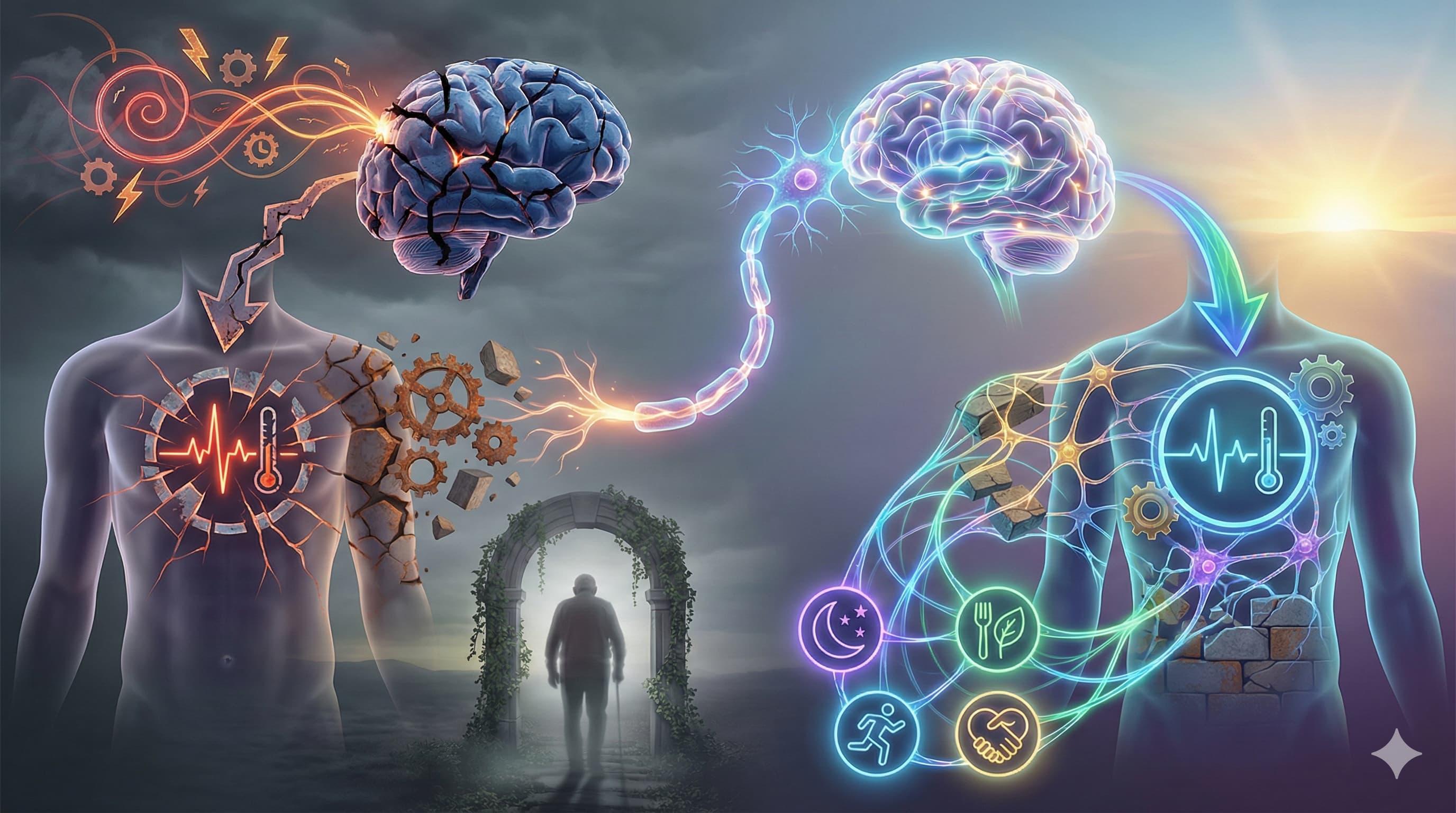
Q3: “You claim inequality accelerates brain aging—is this a permanent scar or reversible plasticity?”
A: The review argues for plasticity, but with caveats. While “Exposome” factors (pollution, chronic stress) cause measurable atrophy (scars), the brain’s “Cognitive Reserve” is dynamic. Interventions like education and rigorous exercise can increase this reserve even in late life, effectively “masking” the structural pathology so clinical symptoms do not manifest. You may not reverse the atrophy, but you can reverse the functional deficit.
Q4: “How do I measure ‘Allostatic Load’ without living in a research clinic?”
A: You cannot measure it directly without a spinal tap or fMRI, but you can track validated physiological proxies at home:
-
HRV (rMSSD): Look for a chronic downward trend, indicating loss of parasympathetic tone.
-
Morning Cortisol: Watch for dysregulation (low morning, high evening).
-
hs-CRP: Chronic elevation (>2.0 mg/L) indicates the systemic inflammation driving the “wear and tear.”
-
Hba1c: Metabolic strain is a core component of the allostatic load index.
Q5: “Does the ‘Biobehavioral Age Gap’ (BBAG) actually predict dementia, or just general mortality?”
A: It predicts both. A higher BBAG (where Biological Brain Age > Chronological Age) is explicitly linked to future declines in specific cognitive domains (executive function, memory) and daily functioning, distinct from general mortality risk. It is a tissue-specific aging clock, not just a systemic one.
Q6: “Why focus on ‘Eudaimonia’ (purpose) when we have tangible targets like amyloid or tau?”
A: Because targeting amyloid has largely failed to reverse symptoms. The paper cites evidence that “Purpose” (Eudaimonia) is linked to a distinct gene expression profile (Conserved Transcriptional Response to Adversity), specifically down-regulating inflammatory genes and up-regulating antiviral/antibody genes. It addresses the upstream driver (systemic inflammation) rather than the downstream symptom (plaque).
Q7: “Is the ‘Swiss Brain Health Plan’ just bureaucracy, or does it offer a deployable protocol I can use?”
A: It is largely bureaucracy and policy. It focuses on public awareness, “brain capital” metrics for economists, and workforce training. While it validates the importance of the field, it does not contain a deployable biohacker protocol. Extract the principles (prevention, biomarkers), but do not look to it for a user manual.
Q8: “What is the minimum effective dose of ‘social connection’ before it becomes diminishing returns?”
A: The paper does not specify a “minute” threshold but notes that subjective loneliness increases dementia risk by 50%. The intervention need only be sufficient to subjectively remove the feeling of isolation. For some, this is a daily call; for others, a weekly group activity. The metric is feeling connected, not time spent.
Q9: “Does Metformin interfere with the mitochondrial benefits of the ‘Weekend Warrior’ strategy?”
A: High Risk. Recent data confirms that Metformin can blunt improvements in VO2 max and vascular insulin sensitivity normally gained from aerobic exercise. The drug triggers a “low energy” signal that may conflict with the exercise-induced adaptation signal.
-
Protocol Adjustment: If your primary goal is the aerobic/mitochondrial benefit of the Weekend Warrior protocol, avoid taking Metformin on your training days.