The Endogenous Toxin: How “Bad Arginine” Drives Senescence and Why Filtering Your Blood Might Be the Future.
In a comprehensive new review published in Hormone and Metabolic Research, researchers from the Technical University of Dresden and King’s College London posit that Asymmetric Dimethylarginine (ADMA) is not merely a bystander in the aging process, but a central “aging toxin” that drives cellular senescence, vascular decline, and mitochondrial dysfunction.
The “Big Idea” is that ADMA acts as an endogenous inhibitor of Nitric Oxide (NO) production. NO is essential for vascular health and mitochondrial biogenesis. As we age, ADMA levels rise, effectively choking off our NO supply. Worse, ADMA “uncouples” nitric oxide synthase (NOS) enzymes, causing them to produce toxic superoxide radicals instead of healthy NO. This creates a vicious cycle of oxidative stress and inflammation—the hallmarks of “inflammaging.”
While caloric restriction and exercise are known to lower ADMA, the authors highlight a radical translational frontier: Therapeutic Apheresis. They propose that mechanically filtering ADMA from the blood could be a potent anti-aging intervention, bypassing the limitations of dietary supplements. This paper reframes ADMA from a simple cardiovascular risk marker to a modifiable target for extending healthspan.
Part 2: The Biohacker Analysis
Study Design Specifications
- Type: Narrative Review & Meta-Synthesis (Not a primary clinical trial).
- Subjects: Summarizes data from Human clinical cohorts (cardiovascular/renal disease) and Rodent models (Mice/Rats) of ischemia and atherosclerosis.
-
Lifespan Data:
- Direct Extension: The review does not present new data showing a specific % lifespan extension from ADMA removal alone.
- Proxy Data: Cites studies where ADMA reduction (via DDAH overexpression or Citrulline/Arginine) reversed endothelial senescence and improved organ recovery in ischemic injury models. High ADMA is consistently cited as an independent predictor of all-cause mortality in humans.
Mechanistic Deep Dive
The paper identifies ADMA as a “molecular saboteur” of the Nitric Oxide pathway:
- NO Inhibition: ADMA competes with L-Arginine for the binding site on Nitric Oxide Synthase (NOS), shutting down NO production.
- NOS Uncoupling: In the presence of high ADMA, NOS enzymes become “uncoupled,” producing Superoxide (O2-) instead of NO. This combines with any remaining NO to form Peroxynitrite (ONOO-), a highly damaging radical that nitrates proteins and damages DNA.
- Senescence Trigger: This oxidative burst triggers the DDR (DNA Damage Response), activating p53/p21 and forcing cells into senescence.
- Organ Priorities: The review identifies the Vasculature (Endothelium) and Kidneys as the primary organs devastated by ADMA accumulation.
Novelty
The paper’s primary novelty is Therapeutic Apheresis as a proposed longevity intervention. While removing lipids (LDL apheresis) is standard, proposing the specific removal of small molecules like ADMA to reverse systemic aging is a significant conceptual shift, moving beyond “supplementing good things” to “filtering out accumulated metabolic waste.”
Critical Limitations
- Translational Gap: The “Therapeutic Apheresis” for ADMA is theoretical in the context of healthy longevity; no clinical trial data is presented showing it reverses aging in healthy humans.
- No “Magic Bullet”: The paper admits there are currently no approved drugs specifically designed to lower ADMA directly (only indirect methods like Citrulline or managing risk factors).
- Causality vs. Correlation: While ADMA predicts death, it is often elevated by renal failure. Whether lowering it independently extends lifespan (without fixing the underlying kidney issue) remains a debate in the literature.
Part 3: Actionable Intelligence
Actionable Intelligence (Deep Retrieval & Validation Mode)
Since “Therapeutic Apheresis” is not accessible to most biohackers, the analysis below focuses on the most effective pharmacological/supplemental strategies to lower ADMA identified in the external search.
The Translational Protocol: L-Citrulline Supplementation
Why Citrulline? It bypasses the liver (unlike Arginine), does not induce Arginase activity (which would destroy it), and effectively outcompetes ADMA at the NOS enzyme site.
-
Human Equivalent Dose (HED):
- Standard Effective Dose: 3,000 mg – 6,000 mg per day.
- Calculation: Based on clinical trials for hypertension/endothelial function, a 6g dose is standard.
- Math: No animal conversion needed as human data exists. If converting from mouse efficacy (1g/kg): $1000 \times (3/37) \approx 81$ mg/kg Human Dose. For a 70kg human $\approx 5.6$g/day.
-
Pharmacokinetics (PK/PD):
- Bioavailability: High (>80%). Reaches peak plasma levels in ~1-2 hours.
- Half-life: Short (~1 hour), but elevates plasma Arginine for 12-24 hours.
-
Safety & Toxicity Check:
- NOAEL: Data suggests safety up to 15g/day in humans.
- Side Effects: Mild GI distress (significantly less than L-Arginine).
- Toxicity: No liver/kidney toxicity signals found at standard doses.
Biomarker Verification Panel
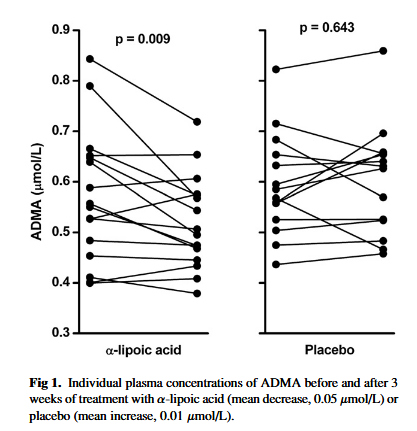
- Primary Target Marker: Plasma ADMA levels (Specialty lab test, ref range: <0.45 µmol/L).
- Functional Surrogate: hs-CRP (Inflammation) and Homocysteine (often correlates with ADMA).
- Blood Pressure: Tracking reductions in systolic BP is a valid proxy for NO restoration.
Feasibility & ROI
- Sourcing: L-Citrulline (pure powder) is widely available as a workout supplement.
- Cost: Low ($20–$30/month for 6g/day).
- ROI: High. Given the low cost and strong evidence for vascular protection, this is a high-value intervention for anyone over 40.
Population Applicability
- Contraindications: Hypotension (low blood pressure), recent heart attack (consult cardiologist regarding NO boosters), or Herpes Simplex (Arginine can trigger outbreaks, though Citrulline is less likely, caution is advised).
Part 4: The Strategic FAQ
1. Is ADMA just a marker of bad kidneys, or does it actually cause aging?
Answer: Evidence suggests causality. ADMA uncouples NOS, directly creating oxidative stress (superoxide) that damages telomeres and induces senescence, even in the absence of kidney disease. It is an active toxin, not just a passive signal.
2. Why not just take L-Arginine to outcompete ADMA?
Answer: L-Arginine has poor bioavailability due to the “First Pass Effect” (liver arginase breaks it down). It can also trigger a feedback loop that increases Arginase activity, making the problem worse long-term. L-Citrulline converts to Arginine in the kidneys, bypassing the liver and providing a sustained Arginine spike without the feedback drawback.
3. The paper mentions “Apheresis.” Can I actually get my blood filtered for longevity?
Answer: Technically, yes, via “Therapeutic Plasma Exchange” (TPE) or specific lipid apheresis available in some clinics (e.g., in Germany or specialized US longevity clinics). However, it is invasive, expensive ($ thousands/session), and currently off-label for “anti-aging.”
4. Does Metformin lower ADMA?
Answer: Yes. External search confirms that Metformin lowers ADMA levels in Type 2 Diabetic patients, likely by improving insulin sensitivity and reducing DDAH inhibition. This reinforces Metformin’s role in vascular protection.
5. How do I test my ADMA levels?
Answer: Standard LabCorp/Quest panels do not include ADMA. You must order a specialty “Endothelial Function” panel or a specific ADMA LC-MS/MS test (Code: 91001 or similar depending on lab).
6. Does Rapamycin interact with ADMA?
Answer: Indirectly. Rapamycin inhibits mTOR. High ADMA activates mTOR via oxidative stress. Therefore, Rapamycin may counteract the downstream effects of ADMA (senescence), but there is no strong evidence that Rapamycin lowers ADMA levels directly.
7. Are there dietary sources of ADMA I should avoid?
Answer: ADMA is formed endogenously (inside your body) when proteins containing methylated arginine are broken down. You cannot “eat” ADMA directly, but eating high-methionine foods (excessive muscle meat) can raise Homocysteine, which inhibits the enzyme (DDAH) that clears ADMA.
8. What is the relationship between Homocysteine and ADMA?
Answer: They are “partners in crime.” High Homocysteine inhibits DDAH activity. DDAH is the enzyme that breaks down ADMA. Therefore, if you have high Homocysteine (MTHFR mutation or B-vitamin deficiency), you almost certainly have high ADMA.
9. Can Nebivolol help?
Answer: Yes. Unlike other beta-blockers, Nebivolol has unique NO-boosting properties and has been shown in studies to lower ADMA levels and improve endothelial function.
10. What is the “Nuclear Option” if supplements fail?
Answer: Beyond Apheresis, the aggressive pharmacological approach involves a “Vascular Stack”: Telmisartan (ARB) + Rosuvastatin (Statin) + Nebivolol. All three have shown potential to lower ADMA or mitigate its vascular harm, but this requires a prescription and medical management.
Context:
- Institution: Technical University of Dresden (Germany) / King’s College London (UK).
- Journal: Hormone and Metabolic Research (Thieme).
- Impact Evaluation: The impact score of this journal is 1.8 (JIF) / CiteScore ~3.8, evaluated against a typical high-end range of 0–60+ for top general science. Therefore, this is a Low/Niche impact journal. Note: While the impact factor is modest, the multi-center collaboration adds credibility.
Research Paper (open access): Asymmetric Dimethylarginine: A Never-Aging Story