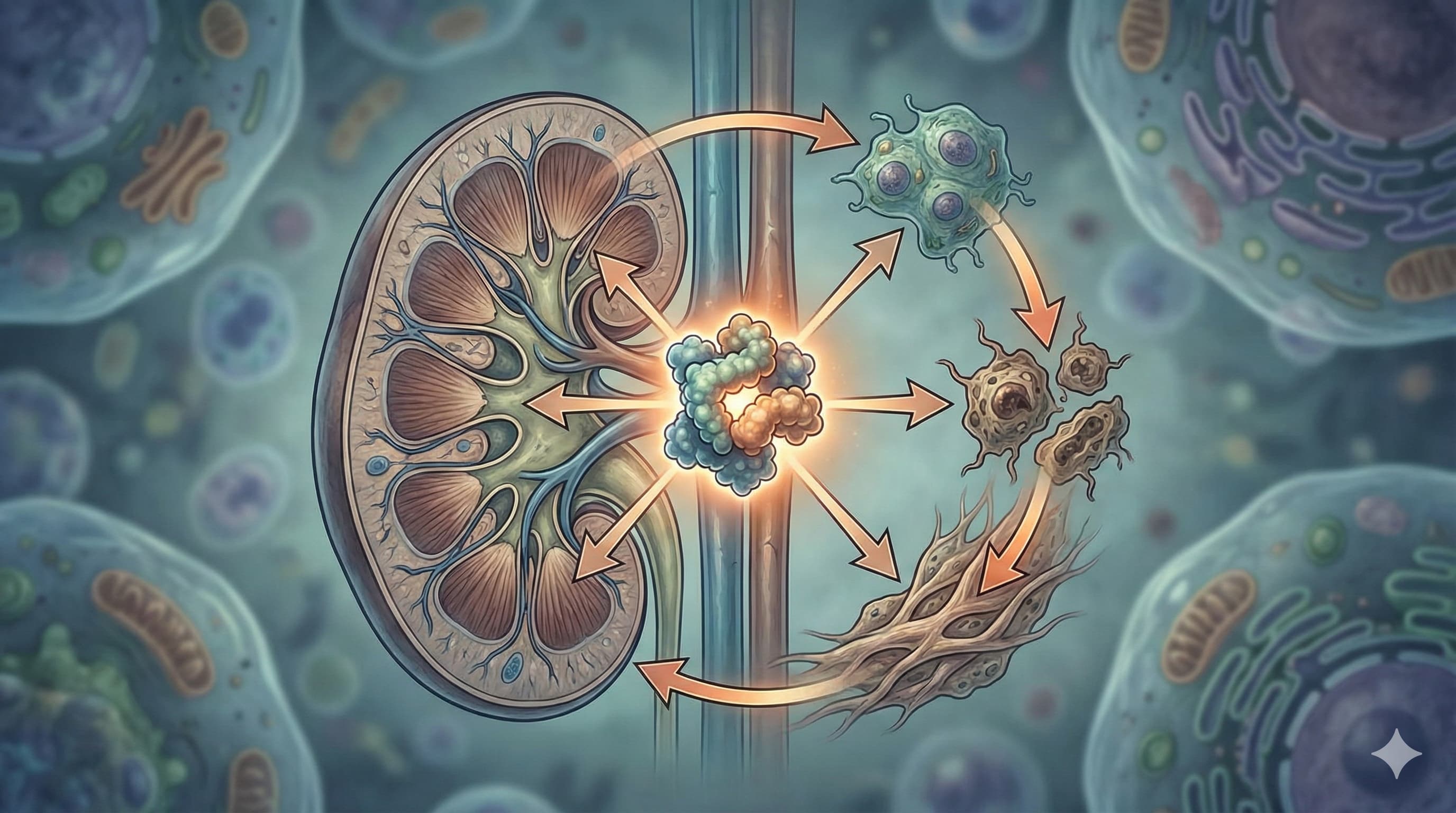
We often treat heart disease, diabetes, and kidney failure as separate battles. A new review from the Czech Academy of Sciences argues they are actually a single war fought on three fronts, coordinated by one master switch: mTOR(mammalian Target of Rapamycin). While longevity enthusiasts know mTOR as the “growth pathway” we want to suppress to slow aging, this paper reveals a more sinister, organ-specific “vicious cycle.”
The big idea here is the interconnectivity of organ failure driven by nutrient sensing. The authors detail how overactive mTORC1 isn’t just about cellular aging; it is the mechanical driver of cardiac hypertrophy (thickening of the heart), hepatic steatosis (fatty liver), and renal fibrosis (kidney scarring).
Crucially, the paper highlights a “backdoor” to mTOR activation that many biohackers miss: Salt. In salt-sensitive individuals, high sodium intake triggers an enzyme called Nox4 in the kidneys. This generates hydrogen peroxide (H2O2), which activates mTORC1 independently of insulin or glucose. This means even if you are fasting and keeping your insulin low, a high-salt diet could still be keeping your pro-aging mTOR pathway hyperactive in your kidneys, driving hypertension and organ damage.
The review ultimately positions mTOR inhibitors (like Rapamycin) not just as anti-aging drugs, but as “circuit breakers” that can stop the feedback loop where liver dysfunction ruins the heart, and kidney failure poisons the blood.
Source:
-
Open Access Paper: Pathogenic Role of mTOR Signaling in Cardiometabolic Disease:
Implications for Heart, Liver, and Kidney Dysfunction (pdf)
Impact Evaluation: The impact score of this journal (CiteScore) is 4.5 (2024), evaluated against a typical high-end range of 0–60+ for top general science (e.g., Nature or Science); therefore, this is a Medium impact journal. It is a respected, peer-reviewed physiological publication with a focus on mechanistic depth.
Part 2: The Biohacker Analysis
Study Design Specifications
- Type: Literature Review (Analysis of multiple in vivo rodent and in vitro studies).
- Subjects: Predominantly Rats (Dahl Salt-Sensitive, Sprague-Dawley, Zucker Fatty) and Mice (C57BL/6J, KO models for Raptor/Rictor).
- Sex: Highlighted sexual dimorphism; females often show distinct cardioprotective mTOR signaling compared to males, influenced by estrogen.
- Lifespan Data: Not the primary endpoint of this review, but it notes that mTORC1 blockade increases mouse longevity and reduces age-associated cardiac dysfunction.
Mechanistic Deep Dive
Mechanistic Deep Dive
The authors deconstruct mTOR into two distinct complexes with opposing roles in longevity:
-
The Villain (mostly): mTORC1
- Heart: Chronic activation drives pathological hypertrophy (thickening) and heart failure. Inhibition (Rapamycin) reverses this remodeling.
- Liver: Drives de novo lipogenesis via SREBP-1, leading to fatty liver (MASLD). Overactivation blocks insulin signaling, causing systemic insulin resistance.
- Kidney: Activated by high glucose and high salt (via Nox4). Drives podocyte injury and proteinuria (leaking protein).
-
The Nuanced Protector: mTORC2
- Heart: Essential for cardiomyocyte survival. Deletion of mTORC2 leads to heart failure, suggesting that “total” mTOR obliteration is dangerous.
- Kidney: Regulates sodium/potassium handling. Overactivation here contributes to salt-sensitive hypertension.
Novelty
The paper integrates the “gut-liver-heart-kidney” axis, specifically highlighting how high-salt intake depletes Lactobacillus murinus, which normally inhibits pathogenic TH17 cells. It also identifies Osteopontin as a predictive marker for liver fibrosis linked to mTOR-driven stellate cell activation.
Critical Limitations [Confidence: High]
- Translational Gap: Most data rely on “extreme” rodent models (e.g., 8% salt diets or genetic knockouts) that do not perfectly mirror human dietary patterns.
- Specificity: Current “Rapalogs” (Rapamycin) do not fully inhibit mTORC1’s phosphorylation of 4E-BP1, leaving some pathogenic protein synthesis unchecked.
- Missing Data: There is a lack of long-term human data on mTOR kinase inhibitors (TORKinibs) like KU-0063794 for metabolic disease due to potential systemic toxicity.
Part 3: Actionable Intelligence
The Translational Protocol
-
Human Equivalent Dose (HED): Based on the study’s reference to 2 mg/kg in mice for anti-obesity effects:
- Calculation: 2 mg/kg (Mouse)×(3/37)≈0.16 mg/kg for humans.
- For a 70 kg adult, this is ≈11.2 mg daily, which is significantly higher than standard weekly longevity doses (5–10 mg/week).
- Pharmacokinetics: Rapamycin (Sirolimus) has low oral bioavailability (≈15%) and a long half-life (≈60–80hours). Peak blood levels occur at ≈2 days post-dose.
- Safety & Toxicity: LD50 in rats is >2500 mg/kg. NOAEL is generally not established for longevity, but human Phase I data for transplant patients show risks of mouth sores, hyperlipidemia, and impaired wound healing at chronic high doses.
Biomarker Verification Panel
- Efficacy Markers: reduction in SREBP-1c (lipogenesis), increase in Beclin-1 (autophagy), and reduction in hsCRP.
- Safety Monitoring: ALT/AST (liver), Cystatin C or ACR (kidney), and Fasting Glucose/HbA1c (to monitor for rapamycin-induced insulin resistance).
Feasibility & ROI
- Sourcing: Rapamycin is prescription-only (Sirolimus). KU-0063794 is a research chemical only and not for human use.
- Cost vs. Effect: Estimated cost for 6 mg weekly is ≈$40–$80/month. High “ROI” for heart/kidney protection in salt-sensitive individuals, but risk of “off-target” effects such as metabolic disruption if not cycled.