The year 2025 marks two major anniversaries that forever changed the fields of metabolism and cell signaling: the 50th anniversary of the discovery of rapamycin in 1975 1,2 and the 60th anniversary of the Medical Expedition to Easter Island (METEI) in 1964–1965,3 during which soil samples, containing Streptomyces hygroscopicus , the bacterium that produces rapamycin, were collected.
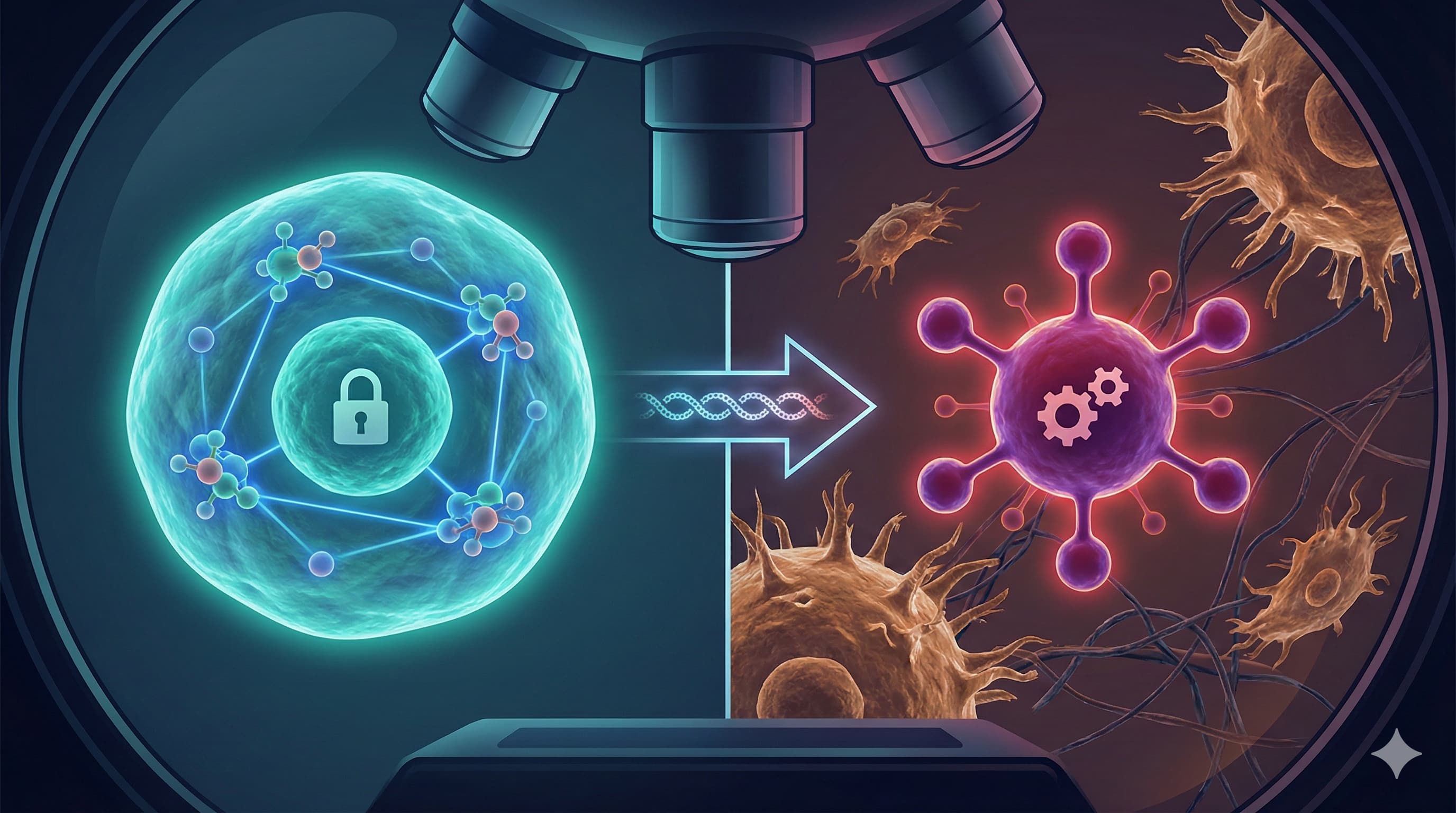
The discovery of rapamycin in the soils of Easter Island is an event that fundamentally altered the landscape of metabolic and longevity research. While early research characterized mTOR primarily as a nutrient sensor, this comprehensive 2025 review argues that mTOR must now be understood as half of a unified “metabolic hub,” functionally inseparable from the mitochondrial network.
The “Big Idea” emerging from this synthesis is that cellular fate dictates—specifically the decision between growth and repair—are governed by a bidirectional crosstalk between mTOR complexes and mitochondria. mTORC1 does not merely respond to nutrients; it actively dictates mitochondrial biogenesis by regulating the master transcriptional coactivator PGC-1α. Simultaneously, it manages mitochondrial quality control, suppressing autophagy and mitophagy when nutrients are abundant, and releasing these brakes to clear damaged organelles during stress. The failure of this coordination is the hallmark of aging and neurodegeneration.
The review highlights a critical pivot in therapeutic strategy. First-generation rapalogs often failed in oncology because they incompletely inhibited mTORC1 substrates (specifically 4E-BP1) and triggered compensatory survival loops via AKT. The frontier has now shifted to “third-generation” inhibitors like RapaLink-1, a bitopic molecule that physically tethers rapamycin to a kinase inhibitor to overcome drug resistance.
Practically, the data suggests that the “more is better” approach to mTOR inhibition is flawed. Chronic inhibition disrupts the delicate mTORC2-mediated control of insulin sensitivity, leading to metabolic derangement. The future of longevity therapeutics lies in intermittent or context-specific modulation that preserves the mitochondrial-mTOR axis, extending healthspan without compromising the immune or metabolic integrity of the host.
Source
- Open Access Paper: mTOR signaling networks: mechanistic insights and translational frontiers in disease therapeutics
- Institution: CNRS UMR9018, Université Paris-Saclay, Gustave Roussy (France) and Zhengzhou University (China).
- Journal: Signal Transduction and Targeted Therapy (STTT).
- Impact Evaluation: The impact score of this journal is 39.3 (JIF) / 18.4 (CiteScore), Therefore, this is an Elite impact journal. (Note: STTT is a Nature Portfolio journal with an exceptionally high citation rate, indicating strong consensus relevance in the field.)
Part 2: The Biohacker Analysis
Study Design Specifications
- Type: Comprehensive Review & Meta-Synthesis (Not a single experimental trial).
- Data Source: Synthesizes data from ~500 primary papers, spanning Yeast (S. cerevisiae), Worms (C. elegans), Flies (D. melanogaster), Mice (M. musculus), and Human clinical trials.
-
Lifespan Data (Aggregated):
- Mice: Cites ITP and Harrison et al. (2009) where rapamycin extended median lifespan by ~9-14% and maximum lifespan significantly in heterogeneous mice.
- Mechanism: Confirms lifespan extension is dose-dependent and sex-dependent (often stronger in females due to PK differences).
Mechanistic Deep Dive: The Mitochondrial Connection
The authors shift the focus from simple translation inhibition to Organelle Crosstalk.
- Mitochondrial Biogenesis (The Build): mTORC1 activates PGC-1 alpha via YY1 interaction, driving the creation of new mitochondria. This explains why chronic high-dose mTOR inhibition can cause muscle wasting (sarcopenia) and fatigue—you stop building the power plants.
- Mitophagy (The Clean-up): This is the longevity payoff. Active mTORC1 phosphorylates ULK1 and TFEB, blocking them. Inhibiting mTORC1 releases this brake, allowing the cell to digest defective mitochondria.
- The “Axolotl Paradox”: The review identifies a specific evolutionary divergence. Axolotls have an mTOR variant that remains active even during low nutrient availability, allowing massive regeneration without the “shutdown” seen in mammals. This suggests human mTOR is evolutionarily “tuned” for survival over regeneration.
Novelty: What’s New?
- mTORC3? The paper tentatively introduces mTORC3, a complex involving ETV7, which is rapamycin-resistant and lacks typical subunits. Its function is poorly defined but represents a potential “escape route” for cancer cells treated with current inhibitors.
- Mitochondria-Lysosome Contacts (MLROs): The identification of “Mitochondria-Lysosome Related Organelles” describes a direct disposal pipeline for mitochondrial debris that mTORC1 regulates, independent of classical autophagy.
Critical Limitations
- Translational Gap: While the review lauds “intermittent dosing” to spare mTORC2 (and thus prevent insulin resistance), it offers no specific human protocol (e.g., 6mg/week vs. 20mg/biweekly). It remains theoretical.
- mTORC2 Ambiguity: The review admits we still cannot selectively inhibit mTORC1 without eventually hitting mTORC2 with rapamycin monotherapy. This “bleed-over” is the primary cause of metabolic side effects (hyperglycemia/hyperlipidemia) in human longevity protocols.
- Missing Data: There is a distinct lack of data on mTORC1-specific biomarkers in healthy humans. We rely on surrogates (immune response) rather than direct tissue biopsies showing reduced p-S6K1 levels.
Part 4: The Strategic FAQ
1. Does the focus on mitochondria change the timing of my dosing? Answer: [Confidence: Medium] Possibly. Since mTORC1 regulates mitochondrial biogenesis (daytime/anabolic) and mitophagy (nighttime/catabolic), taking rapamycin in the morning might align better with circadian rhythms to suppress inappropriate aging-associated diurnal mTOR hyperactivity, while allowing nightly recovery.
2. Is mTORC2 inhibition inevitable with chronic rapamycin use? Answer: [Confidence: High] Yes, with chronic daily use. The review confirms that while rapamycin is selective for mTORC1 acutely, prolonged exposure sequesters the mTOR protein, preventing mTORC2 assembly. Pulsed (weekly) dosing is the best theoretical workaround to mitigate this.
3. Does this paper suggest any “stack” to mitigate mTORC2 side effects? Answer: [Confidence: Medium] Indirectly. The paper notes that metformin inhibits mTORC1 via AMPK (a different pathway). Stacking Metformin might allow for a lower dose of Rapamycin, potentially preserving mTORC2 function while still crushing mTORC1.
4. What is “mTORC3” and should I be worried about it? Answer: [Confidence: Low] The review mentions mTORC3 is rapamycin-resistant. Currently, this is a research curiosity with no clinical intervention. It suggests that even with perfect rapamycin usage, some mTOR-like signaling persists.
5. If I am building muscle (anabolic), will Rapamycin destroy my gains? Answer: [Confidence: High] Yes, if timed poorly. mTORC1 is required for protein synthesis and hypertrophy. Taking rapamycin immediately post-workout would blunt the anabolic signal. Biohackers typically dose on “rest days.”
6. Can I test if Rapamycin is working without a muscle biopsy? Answer: [Confidence: Medium] It is difficult. Commercial tests for p-S6K1 in blood cells (PBMCs) are rare. The best proxies are “side effect” tracking (e.g., small mouth sores indicate high drug exposure) and tracking biological age clocks (PhenoAge, GrimAge), although their responsiveness to Rapamycin is currently debated.
7. How does Rapamycin affect my risk of bacterial infection? Answer: [Confidence: Medium] It is nuanced. While it suppresses rejection (T-cells), the review notes it can enhance pathogen clearance by boosting autophagy (lysosomal degradation of bacteria). However, if you have an active bacterial infection, stop dosing.
8. Does the review support “cycling” (e.g., 3 months on, 1 month off)? Answer: [Confidence: Medium] The review cites transient treatment in middle-aged mice extending lifespan. This strongly supports the idea that you do not need to be on the drug 24/7/365 to harvest the longevity benefits, supporting a cycling protocol.
9. What about “RapaLink-1” or “Third Generation” inhibitors mentioned? Answer: [Confidence: High] These are for cancer, not longevity. They are designed to kill cells by totally blocking mTOR (1 and 2). Avoid these for healthspan; they are too toxic for a healthy biohacker.
Rapamycin Conflict Check:
- Metformin: Synergistic. Both inhibit mTORC1 but via different routes (Direct binding vs. AMPK activation).
- Acarbose: Synergistic. Targets glucose spikes which feed upstream mTOR activation.
- 17-alpha Estradiol: Likely compatible (males only), acts via distinctive metabolic pathways.
- SGLT2 Inhibitors: Synergistic. Lowers insulin/glucose, reducing upstream pressure on mTOR.
Reasoning Framework:
- Priors: Rapamycin is the gold standard.
- Update: This review solidifies the mitochondrial mechanism as the primary driver of its success, rather than just “slowing growth.”
- Uncertainty: Human optimal dosing remains the largest “unknown” in the field.