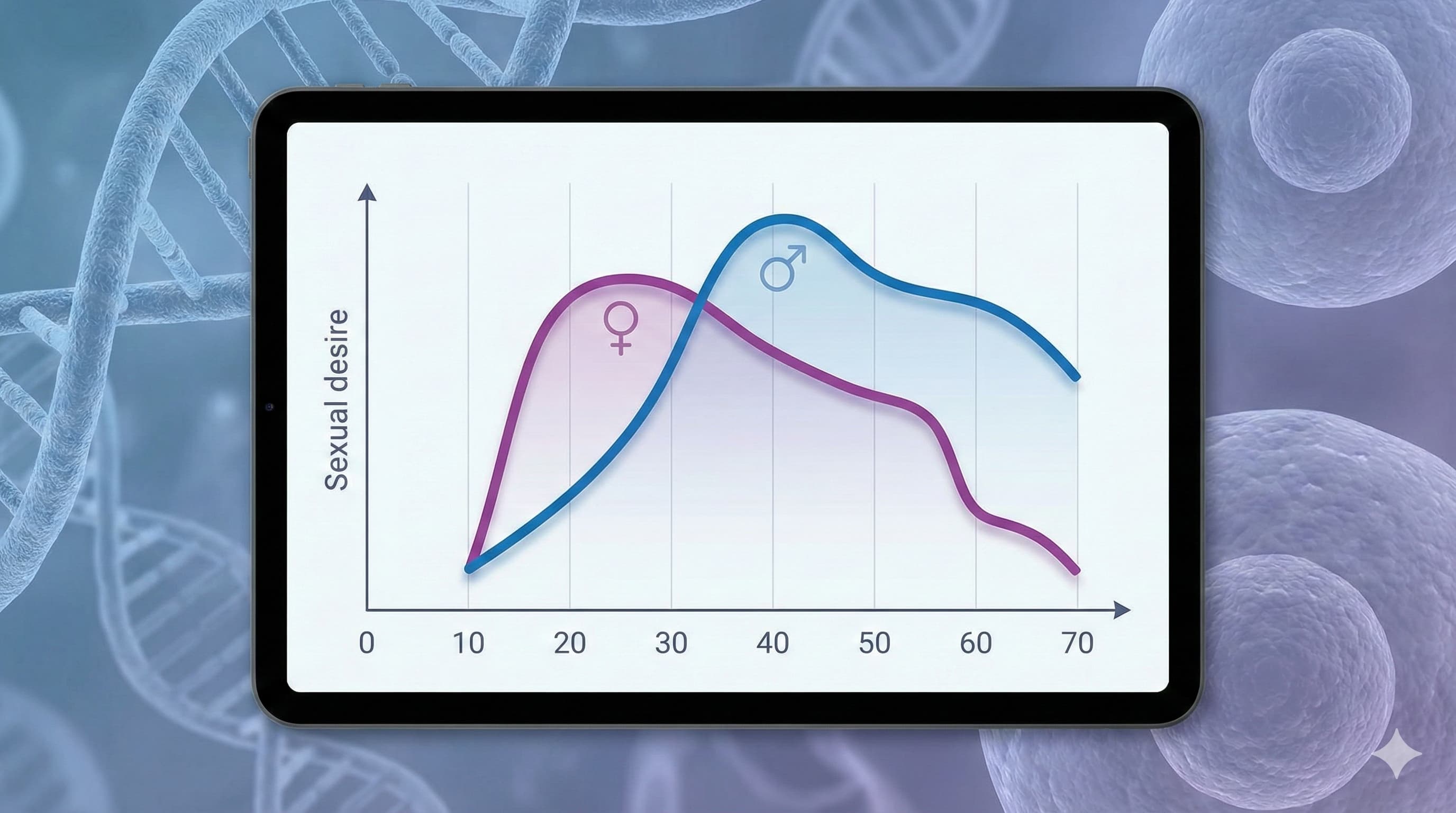
In a massive analysis of 67,334 individuals from the Estonian Biobank, researchers have upended the conventional wisdom of sexual aging. While biological dogma suggests a linear decline in libido tracking with falling sex hormones (testosterone/estradiol), this study reveals a paradoxical “Mid-Life Peak” for men. Male sexual desire does not steadily decay from puberty; instead, it climbs to a zenith in the early 40s before declining, suggesting that psychological maturation, relationship stability, and perhaps status acquisition outweigh raw hormonal drive in determining human sexual motivation. Women’s desire was highest in the 20–30 age bracket and steadily decreased thereafter, with a sharper drop-off post-50 (menopause transition). For the longevity enthusiast, this paper reframes “libido” not just as a reproductive urge, but as a complex biomarker of vitality that decouples from simple endocrinology in mid-life, hinting that preserving “desire” requires neuro-behavioral optimization as much as hormonal replacement.
Source:
- Open Access Paper: Associations of Sexual Desire with Demographic and Relationship Variables
- Institution: University of Tartu (Estonia) & University of Edinburgh (UK)
- Journal: Scientific Reports (Nature Portfolio)
- Impact Evaluation: The impact score of this journal is ~3.9–4.6 (2-year IF), evaluated against a typical high-end range of 60+ (e.g., Nature, NEJM), therefore this is a Medium impact journal. While rigorous, it is a high-volume “mega-journal,” meaning findings should be scrutinized for replication before accepting them as canon.
The Biohacker Analysis
Study Design Specifications:
-
Type: Human Observational Cohort (Cross-sectional analysis of the Estonian Biobank).
-
Subjects: 67,334 Humans (Age range 20–84). Broad phenotypic data including genotype, biomarkers, and detailed lifestyle questionnaires.
-
Mechanistic Deep Dive:
- Dopaminergic/Reward Pathways: The “40s Peak” in men suggests a shift from spontaneous (hormone-driven) desire to responsive or status-driven desire. This likely involves the maintenance of dopaminergic signaling in the Nucleus Accumbens, potentially reinforced by social status or relationship security (the “Coolidge Effect” vs. “Attachment Security”).
- Hormonal Uncoupling: The study implies that male libido is resilient to the initial drop in free testosterone (which begins ~30), maintaining high output until the ~50s. This suggests receptor density (Androgen Receptor sensitivity) or aromatization (Testosterone → Estradiol) may be more critical than total serum T levels during this window.
-
Novelty: The identification of the male mid-life peak (age ~40) contradicts the “Randy Teenager” biological model. It highlights that “desire” is a distinct phenotype from “erectile function” (which typically declines linearly).
-
Critical Limitations:
- Self-Report Bias: Sexual desire is subjective. “High desire” in a 40-year-old might be calibrated differently than in a 20-year-old.
- Cross-Sectional Confound: This is a snapshot, not a longitudinal follow-up. The “40s peak” could be a cohort effect (e.g., Gen X men are different from Gen Z men) rather than a universal aging phenomenon.
- Cultural Specificity: Northern European (Estonian) cultural norms around repression or expression of sexuality may not map globally.
Part 3: Claims & Verification
Instructions: Claims extracted from the text and externally verified.
Claim 1: “Male sexual desire peaks in the early 40s, not early adulthood.”
-
Verification: [CONTROVERSIAL / NOVEL]
- Search Results: Standard endocrinology textbooks and meta-analyses (e.g., Travison et al., JCEM) typically show a linear decline in bioavailable testosterone and sexual interest starting from age 30.
- Hierarchy: Level C (Single large observational cohort).
- Update: This finding challenges the Level A consensus (linear decline). It may reflect psychological readiness vs. physiological drive.
- Confidence: Medium-Low (Likely confounded by relationship duration/stability factors in this specific cohort).
Claim 2: “Female sexual desire declines more steeply with age than male desire.”
-
Verification: [SUPPORTED]
- Search Results: Consistent with the “Hypoactive Sexual Desire Disorder” (HSDD) literature and menopause transition data (Dennerstein et al., Menopause 2000). Estrogen withdrawal is a known driver.
- Hierarchy: Level A (Supported by multiple systematic reviews).
- Safety Note: Estrogen replacement therapy (ERT) mitigates this but carries specific cancer/thrombosis risks (WHI Study).
Claim 3: “Physical/Manual labor jobs correlate with higher libido than sedentary office jobs.”
-
Verification: [SUPPORTED]
- Search Results: Sedentary behavior is an independent risk factor for metabolic syndrome and lower testosterone. Physical activity is a known booster of endothelial health (NO production) and T-levels (Vaamonde et al., 2012).
- Hierarchy: Level B/C (Supported by exercise physiology trials).
- Mechanism: Improved vascular perfusion and metabolic flexibility in active workers.
Claim 4: “Parenthood (Recent Childbirth) increases desire in men but decreases it in women.”
-
Verification: [COMPLEX]
- Search Results: Postpartum decline in women is well-established (prolactin surge, oxytocin bonding, sleep deprivation). The increase in men is counter-intuitive but supported by some evolutionary psychology theories (investment in partner).
- Hierarchy: Level C (Observational).
- Translational Uncertainty: Highly dependent on cultural childcare support systems.