Okay, just to be sure - I did more research on the biochemistry side because it makes no sense that the FDA would say only at the evening and never at morning on the label, on top of my dermatologist being so specific. If you want to go against the experienced reviewers and safety experts…then you better have a good reason.
I assure you every single PA or NP I’ve talked to never goes into biochemistry or FDA/patient safety studies in depth - they defer to an expert and stay in their lane if they are not overconfident. Every single highly paid patient safety consultant I know is an MD.
“Animal studies on compounds with a similar mode of action to adapalene have suggested that these may enhance the development of skin cancers caused by UV light. Adapalene is essentially stable to oxygen and light and is chemically non-reactive. Whilst short term studies have shown no phototoxic to photoallergic potential of adapalene, small numbers of reactions consistent with phototoxicity were reported in clinical studies, the safety of using adapalene during long or repeated exposures to sunlight or UV radiation has not been established in animals or humans. Exposure to sunlight or UV irradiation (including sunlamps) should be avoided during treatment with adapalene. Use of sunscreen products and protective clothing over treated areas is recommended when exposure cannot be avoided.”
The recommendation goes against the FDA label as well as the safety studies above. Sunprotection does not necessarily mean sunscreen. I’ve seen some recommend staying in the shade or avoiding the outdoors, partly because some chemical sunscreens can cause cancer with benzene, see recent J&J sunscreen large-scale recalls. I’ve had the same midlevel practitioners never raise this specific benzene manufacturing concern, but the derms I had with deep research background said to use zinc oxide just to be sure based on FDA data GRASE: https://www.fda.gov/media/124655/download.
Indoor lamps have UV. UV can go through windows indoors as well and bounce off reflective surfaces like water. It’s not just sunlight outdoors.
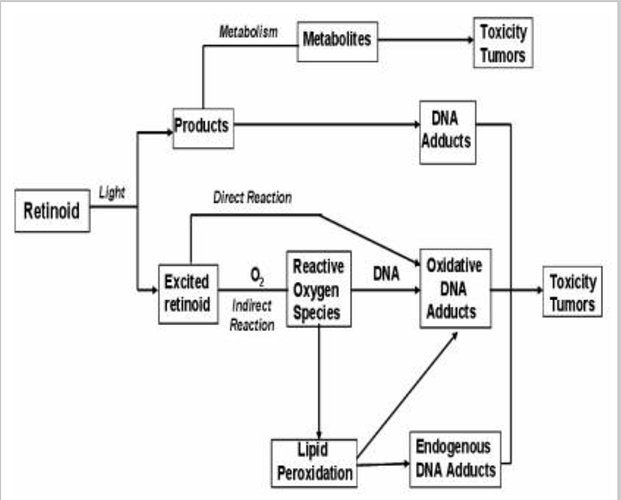
Biochemistry pathway of retinoids:
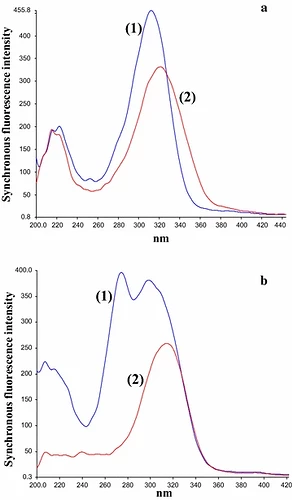
Relative “photostability” says nothing about UV stability. Here are the wavelengths at which adapalene is excited via UV light. As you can see, adapalene is much more stable in visible light than tretinoin from the graph (not perfect 100% either), but not UV light.
So yes, it is relatively high photostability for light in the visible spectrum, but not UV stable nor perfect photostability.
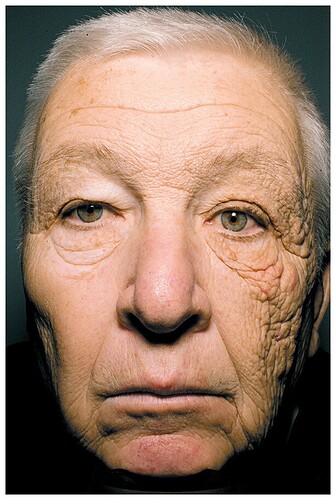
We know air pollution leads to ROS, which leads to premature skin aging, senescence, immunosuppression, and photocarcinogenesis - that’s why we use skin cleansers daily.
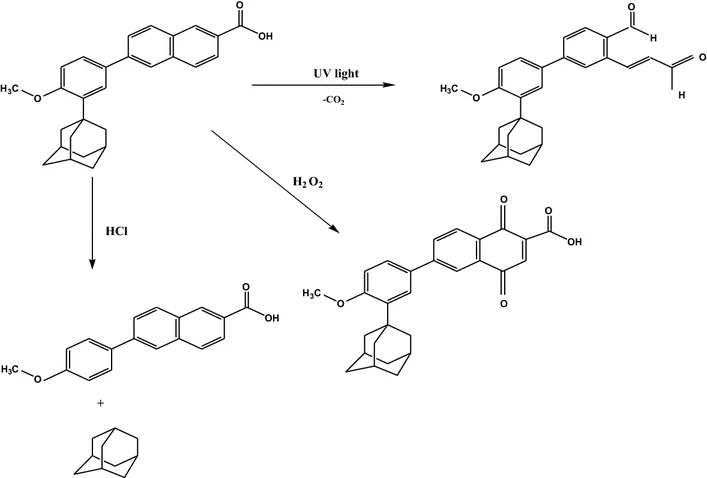
Adapalene without any UV exposure and only light exposure is probably safe or negligible - so yes, the study is not wrong to say it is “photostable” in visible light. Adapalene with UV exposure may cause cancer from metabolites and ROS production, as noted in safety studies empirically and retinoid mechanistic chemical pathways. It is probably exacerbated in morning use.
I use Retin-A in the evening (no light at all) partly to avoid mixing morning skin care products (acidity and presence of oxidation agents can accelerate degradation rates leading to possible metabolites that may be tumorigenic) and partly because of skin turnover rates, not just because of photolability. Just attributing it to photostable is missing all the subtleties of treatment. “15 years of derm experience” probably meant the same batch of uncomplicated/simple patients parroting the same advice without much complex thought, not complex derm patients and/or complex skincare formulations and/or in-depth dermatology research. Again, consistent with me and my colleagues’ observations of the proliferation of overconfident midlevel practitioners. All you have to do is ask your physician or check out the midlevel discussions. There are plenty of midlevels who openly talk about NP degree mills with 100% acceptance rates/online degrees and overconfident midlevels in their own reddit forums, it’s not just the physicians. There is also a reason private equity firms are funding midlevel education and lobbying for independent practice - churns out cheaper labor quickly (lower labor cost) with lower quality but the same bill = more unnecessary labs and consults = more profits = two-tier healthcare system.
I wouldn’t be surprised if the patients getting advice from someone with non-research backgrounds have a higher rate of aging and cancer when using adapalene in the morning over long periods of time. My guess is someone just ran with the “photostability” story and assumed you could just use it in the morning since there were no big issues in the short-term studies that used visible light only. It’s not a surprise to me when I ask for long-term safety studies - there are no answers and just a dodge. Nor was there a direct response to the multiple chemistry mechanisms showing an issue or patient safety issues in the empirical studies we already know about.
Here are the chemical pathways of adapalene in the presence of oxidation, acidity, and UV light (not visible light):