Do you use it every day ? Twice a day? Could you take a picture of the ingredients? Thank you very much
Not all red light is the same, and not all devices are equal. I did a fair bit of research on this a few years ago when I started with redlight therapy, and I settled on one company whose devices and research I trust: https://gembared.com/
I use and recommend Gembared devices. They are reasonably priced for high-quality. Check out their articles for more details.
Just looked at them and to be fair they are the first company I’ve seen giving real light output values:
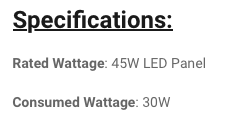
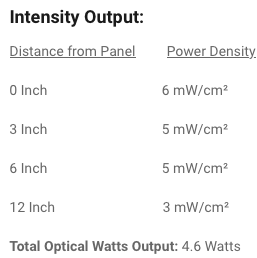
This is totally consistent with the measurements I made on a similar panel and very far from the “Marketing inflated” values of the amazon vendors who claim to have 100mW/cm2 or more.
Here, we demonstrate that murine melanocyte-specific Bmi1 deletion causes premature hair greying and gradual loss of melanocyte lineage cells. Depilation enhances this hair greying defect, accelerating depletion of McSCs in early hair cycles, suggesting that BMI1 acts to protect McSCs against stress. RNA-seq of McSCs, harvested before onset of detectable phenotypic defects, revealed that Bmi1 deletion derepresses p16 Ink4a and p19 Arf, as observed in many other stem cell contexts. Additionally, BMI1 loss downregulated the glutathione S-transferase enzymes, Gsta1 and Gsta2 , which can suppress oxidative stress. Accordingly, treatment with the antioxidant N-acetyl cysteine (NAC) partially rescued melanocyte expansion. Together, our data establish a critical function for BMI1 in McSC maintenance that reflects a partial role for suppression of oxidative stress, and likely transcriptional repression of Cdkn2a.
BMI1 is required for melanocyte stem cell maintenance and hair pigmentation
Fluoxetine promotes human hair follicle pigmentation ex vivo: serotonin reuptake inhibition as a new antigreying strategy?
DEAR EDITOR, The commonly prescribed antidepressant, fluoxetine, has been reported to (rarely) induce epidermal hyperpigmentation after systemic application.1 This selective serotonin reuptake inhibitor (SSRI) can also stimulate melanin production in murine hair follicles (HFs) in vivo under conditions of perceived stress and in cultured human epidermal melanocytes in vitro.2,3 Given the distinct neuroendocrine controls that human HF melanocytes underlie compared with epidermal melanocytes,4and that any pigmentary effects of fluoxetine observed in vivo may have been indirectly mediated, it remains entirely unclear whether fluoxetine impacts directly on human HF pigmentation, specifically in the absence of systemic and neural inputs. In the current pilot study we explored this question after determining the presence of the serotonin transporter and serotonin receptors 1A and 2A at the mRNA and protein levels (data not shown).
Specifically, we asked whether fluoxetine (chosen among other SSRIs for its long half‐life and known pigmentary effect in mice)2,3 can alter the pigmentation of microdissected, organ‐cultured human scalp HFs, using our previously reported HF pigmentation readouts and established protocols.5,6Pigmented, full‐length scalp HFs in anagen VI (obtained from facelift surgery of female donors after written patient consent and ethics approval) were treated for 48 h with 100 nmol L−1 and 1 μmol L−1fluoxetine in serum‐free supplemented Williams’ E medium.5,6 Given the very limited availability of human HFs, the fluoxetine test concentrations were selected based on previously published results.2
Quantitative Masson–Fontana histomorphometry showed that fluoxetine further and significantly increased melanin production in the HF pigmentary unit of already maximally pigmented anagen VI HFs ex vivo (Fig. 1a). This provides the first evidence that fluoxetine can directly stimulate human HF pigmentation in the absence of systemic or neural inputs.
As white HFs occasionally retain a few functionally active melanocytes in their pigmentary unit,7 we next asked whether fluoxetine can stimulate some degree of repigmentation in a very small number of white HFs isolated from five female donors with > 50% canities over a period of ≥ 6 years. These HFs were obtained from 6‐mm punches collected by a contract research organization after receiving written patient consent and ethics approval. Strikingly, fluoxetine induced significant restimulation of intrafollicular melanin production after 6 days of HF organ culture, as measured by quantitative Masson–Fontana histomorphometry (Fig. 1c). This was accompanied by a tendency for upregulation of gp100 immunoreactivity (data not shown), indicating increased premelanosome production and melanocyte activity.5,6 This preliminary evidence in a low number of HFs suggests that at least some canities‐affected HFs can, in principle, be reactivated by fluoxetine to produce melanin
Given that α‐melanocyte‐stimulating hormone (MSH) is a key neuroendocrine stimulator of human HF pigmentation and is synthesized within human anagen scalp HFs,4 and that fluoxetine can modulate the expression and production of α‐MSH in rats and humans,8 we next investigated the effect of fluoxetine on this melanotropic neurohormone. Immunofluorescence microscopy for α‐MSH was performed on anagen HFs and assessed by quantitative immunohistomorphometry in a defined reference area (proximal outer root sheath). This showed that 1 μmol L−1 fluoxetine slightly, but not significantly, stimulated α‐MSH protein expression. While overall this did not reach statistical significance, individual HFs showed a marked increase of α‐MSH immunoreactivity (Fig. 1b). Essentially the same effect was seen in white HFs (Fig. 1d).
Given the low number of HFs we could analyse, the current pilot data are obviously preliminary and require rigorous reproduction in additional HFs from more individuals. However, our preliminary observations strongly suggest that fluoxetine directly promotes human HF pigmentation and may even reverse the depigmentation of at least some ‘white’ female human scalp HFs. Furthermore, the observation that fluoxetine can also upregulate the intrafollicular production of a melanotropic neurohormone (α‐MSH) in some white HFs of women with long‐standing canities suggests that this SSRI may exert longer‐lasting, neuroendocrine changes within white HFs. This would facilitate HF repigmentation by enhancing the capacity of ‘white’ HFs to restore their pigmentation production capacity before the point of no return in HF greying, i.e. when HF melanocyte stem cells have been lost.
The obvious clinical key challenge now is to study whether the observed ex vivo effects of fluoxetine translate to the in vivo situation (ideally after topical application) and to dissect whether or not topical application of this SSRI also stimulates epidermal hyperpigmentation, which would be undesired in the scalp skin of most individuals undergoing hair greying. In any case, our pilot study strongly encourages systematic exploration of fluoxetine as a candidate hair antigreying agent.
seems like this might relate to the senolytic approaches, and sphingolipids: Senolytics Topically Administered to Skin for Antiaging Effects
Posted that in the IL-17 thread but it’s relevant to that thread too.
[Edit] I just noticed this has been posted before. Sorry about that but the link with the IL-17 discussion makes it more relevant.
Latanoprost, a prostaglandin (PG) F2α analogue, is an effective and widely used medication in the treatment of open-angle glaucoma.1 Since its introduction, several adverse effects have been reported, prominent among which has been increased pigmentation of the iris and eyelashes.2 We describe a patient who developed repigmentation of her previously white hair after latanoprost therapy.
A 65-year-old woman with open-angle glaucoma of 3 years duration mentioned recent changes in her hair colour. She was in a good state of health. Treatment with topical 0.005% latanoprost, 1 drop (∼20 μL) every evening, was started in her both eyes on April 2007. The patient first noticed gradual darkening of her hair, which had been completely white for 20 years, approximately 3 years after she started latanoprost therapy. She referred that her hair had gone progressively greying over the years and she did not report any trigger factors like systemic diseases or stressful events. The repigmentation with the original colour took about 1 year. It started from the root and the proximal part of the hair and then interested all the hair length. She denied the use of any dyeing or new shampoo or any lotion for the scalp during this whole interval. On physical examination, hair darkening was spreading (Fig. 1). Eyebrows and the skin around patient’s eyes were instead unchanged. The patient continued latanoprost therapy and the pigmentation of her hair has persisted after 9 months of follow-up.
The first reported and most prominent adverse effect of latanoprost eye drop is darkening of the irides. More recently reported adverse effects of that drug are hyperpigmentation of the eyelid, neck, back or temporal area of the face2 and also change of eyelashes and vellus hair in the treated eye including pigmentation, increased length, thickness and misdirected growth of eyelashes.1
The underlying mechanism of latanoprost-associated hair and skin change in growth and pigmentation is poorly understood. As latanoprost is a selective agonist for the PGF2α receptor, it is likely that the phenomenon is mediated by this receptor. PG is one of the most potent stimulants of melanogenesis[6] and melanocyte growth7 and the release of PGs, primarily PGE2 and PGF2α, in the skin is one of the mechanisms of action of ultraviolet rays,8the best-known stimulant of melanogenesis.
A study on a guinea pig model has demonstrated that PGF2α analogues (including latanoprost) topically applied increase skin pigmentation.[9]. A study on a murine model has demonstrated the influence of PGF2α and its analogue latanoprost on hair regrowth and follicular melanogenesis.[10]
Preliminary experiments carried out in a human model have shown that a very brief (<21 days) latanoprost exposure cause hypertrichosis of eyelashes that persists also in the absence of the drug.[1]
Although drug-induced repigmentation was the most probable explanation for the hair-colour change in our patient, the relation between drug intake and hair darkening would have been proven only if hair had returned to its original colour after drug withdrawal. We were unable to make such an observation as the patient continued the treatment. Repigmentation of hair is an uncommon phenomenon, and the mechanism continues to defy explanation. We have described a further case illustrating that hair greying is not an irreversible process. In this patient, the repigmentation was imputated to latanoprost therapy, an association not previously reported. Advances in understanding the pathophysiology should promote development of therapeutic approaches to avoid or repair the greying process.
Ask them.
Cheap from the regular India-based suppliers… About $1 to $2 per small bottle…
I wonder if scalp topical use would be a good thing to try with this… mix with transcutol or DMSO…
I’ve been using this for years on my eyebrows and eyelashes and it works for me wherever it’s applied. I have not noticed my scalp hair darkening or graying reversed. That said my grays have not increased. It’s hard to know whether or not it might have been worse if I’d not started using it.
A couple of months ago about the same time that I made my topical rapamycin skin treatment I put a full 3ml bottle bimatoprost eye drops in distilled water and transcutol to use as a scalp spray in hopes of repigmentation. I’ll keep y’all posted if it works.
Interesting article, @Bezesk. Here’s support for this in treating skin depigmentation from vitiligo in a small clinical trial. My understanding is that both the Lantanoprost cream and the UV light treatment are temporary, meaning they last for a few months but need to be administered pretty much forever (maybe pulsed, but forever). I had the laser treatment for vitiligo (miraculously insurance paid for it) and the dermatologists said it was much better than the cream (although that may have been because they bought the excimer laser already) — treatment was a real pain: 30 sessions coming in to the office over 12 consecutive weeks, it maybe darkened spots a bit (suggested 25-75%) and only supposed to last 9-18 months, so every year I’d have to spend 12 weeks coming into my doctor’s office 3x per week….not the most convenient for those of us not yet retired, or who travel.
The effect of latanoprost on vitiligo: a preliminary comparative study
Tag S Anbar et al. Int J Dermatol. 2015.
Abstract
Latanoprost (LT), a prostaglandin F 2alpha (PGF2a ) analogue used in the treatment of glaucoma, was found to induce skin pigmentation in guinea pigs in addition to its known periocular and iridal pigmentation side effects. This study aims to evaluate the efficacy of topical LT in the induction of skin repigmentation in patients with vitiligo and to compare its potency with narrow band ultraviolet (UV) B (NB-UVB). The result of their combination was also assessed. This study involved 22 patients with bilateral and symmetrical vitiligo lesions, stable for the last three months, divided into three groups: group I, to evaluate LT vs. placebo; group II, to evaluate LT vs. NB-UVB; and group III, to evaluate the effect of their combination. The response to treatment was evaluated by taking photographic records of the treated lesions with follow-up photography every two weeks. After three months, assessment of the degree and extent of repigmentation was performed. Follow-up assessment was done six months after termination of the trial for the persistence of pigmentation, recurrence, or development of any side effects. LT was found to be better than placebo and comparable with the NB-UVB in inducing skin repigmentation. This effect was enhanced by the addition of NB-UVB. LT could be a promising treatment for vitiligo, especially the periocular variant. Its effect on skin repigmentation could be enhanced by NB-UVB exposure.
Example :1 Effects of Topical PAI-1 inhibitor formulation on Hair Graying
[02431 A topical study oftopical PAI-1 inhibitor formulation after topical
administration ofa topical formulation ofPAI-1 inhibitor (e.g… see Table 1) in man is
performed. The study is designed to test whether the topical formulation of PAI-1 inhibitor
significantly reduces hair graying in man by measuring hair color change following topical treatment with a PAI-1 inhibitor.
[0244] The study includes two groups of 25 human subjects each. Both groups have subjects with varying levels ofhair follicle density and varying numbers and/or density of gray hairs. The scalp ofeach subject in the second group is treated twice a day for 6 months topically with a fixed volume of aPAI-1 inhibitor formulation that is at a fixed
concentration ofthe PAI-1 inhibitor. The concentration of the PAI-1 inhibitor in the formulation is 5% w/w. The administration of the topical preparation to the scalp takes about 5 minutes, after which the suspension is left on the site for about 8 to 12 hours. The scalps of the subjects in the first group are treated twice a day for 6 months topically with an empty formulation and is the control.
[0245| The expected effect of such a treatment is a reduction in the density of gray hairs at the site of the PAI-I inhibitor formulation treatment. The number of gray hairs at the treatment sites is measured by two methods: 1) A photograph of the treated area is taken to observe a change in the hair color; or 2) A gray hair density test, wherein the gray hair count in a small site on each subject’s scalp is measured. The small site on the scalp is selected prior to the commencement of the study.
[0246] A photograph and the gray hair density test method are employed at baseline prior to a PAI-1 inhibitor treatment. Following this photographs of the scalp of each subject is obtained every four weeks after start oftreatment and at the end of the 6-month study; the gray hair density test is also performed every four weeks after start of treatment and at the end of the 6-month study. The study finds that at Baseline, the average amount of gray hairs counted by either the gray hair density tests or as observed from the photographs is approximately equal across the control and treatment groups. Photographs of the scalps of the subjects of the treatment group on average show a visual reduction in the total number of gray hairs with every four weeks. The gray hair density test also on average shows a reduction in the number of gray hairs in the site selected on the scalp of each subject belonging to the treatment group with every four weeks. In contrast subjects in the control group showed no visual reduction in gray hairs in the treatment site, or reduction in the density ofgray hairs in the selected site on the scalp.
[02471 This study establishes that topical administration of the topical formulation of PAI-1 inhibitor reduces gray hair count and reverses hair graying in humans.
Example 2: Effects of Oral PAI-1 inhibitor formulation on Hair Graying
[0248] A study of oral administration of an oral formulation of PAI-1 inhibitor in man is performed. The study is designed to test whether the oral formulation of PAI-1 inhibitor significantly reduces hair graying in man by measuring hair color change following oral treatment with a PAI-1 inhibitor.
[02491
The study includes two groups of 25 human subjects each. Both groups have subjects with varying levels of hair follicle density and varying numbers and/or density of
gray hairs. Each subject in the second group is administered an oral preparation of PAl-1 inhibitor formulated as a 75 mg capsule thrice a day for 6 months. Each subject in the first group are administered an oral empty preparation formulated as a 75 mg capsule thrice a day for 6 months and serve as the control.
[02501
The expected effect of such a treatment is a reduction in the density of gray hairs due to the PAI-1 inhibitor formulation treatment. The number of gray hairs on the scalps of the subjects is measured by two methods: 1) A photograph of the scalp is taken to observe a change in the hair color, or 2) A gray hair density test, wherein the gray hair count in a small site on each subject’s scalp is measured. The small site on the scalp is is selected prior to the commencement of the study.
[02511 A photograph and the gray hair density test method are employed at baseline prior to a PAI-1 inhibitor treatment. Following this photographs ofthe scalp of each subject is obtained every four weeks after start of treatment and at the end ofthe 6-month study; the gray hair density test is also performed every four weeks after start of treatment and at the end of the 6-month study. The study finds that at baseline, the average amount of gray hairs counted by either the gray hairdensity tests or as observed from the photographs is approximately equal across the control and treatment groups. Photographs of the scalps of the subjects of the treatment group on average show a visual reduction in the total number of gray hairs with every four weeks. The gray hair density test also on average shows a reduction in the number ofgray hairs in the site selected on the scalp of each subject belonging to the treatment group with every four weeks. In contrast subjects in the control group showed no visual reduction in gray hairs in the treatment site, or reduction in the density of gray hairs in the selected site on the scalp.
[0252]
This study establishes that oral administration of the oral formulation of PAI- 1inhibitor reduces gray hair count and reverses hair graying in humans.
Could you share the name of the pharmacy that produces a compounded cream version of tacrolimus? I would like to ask my dermatologist if she will send an Rx there for me. I am currently using the ointment and it is a bit annoying. Thank you!
What questions do you have for them?
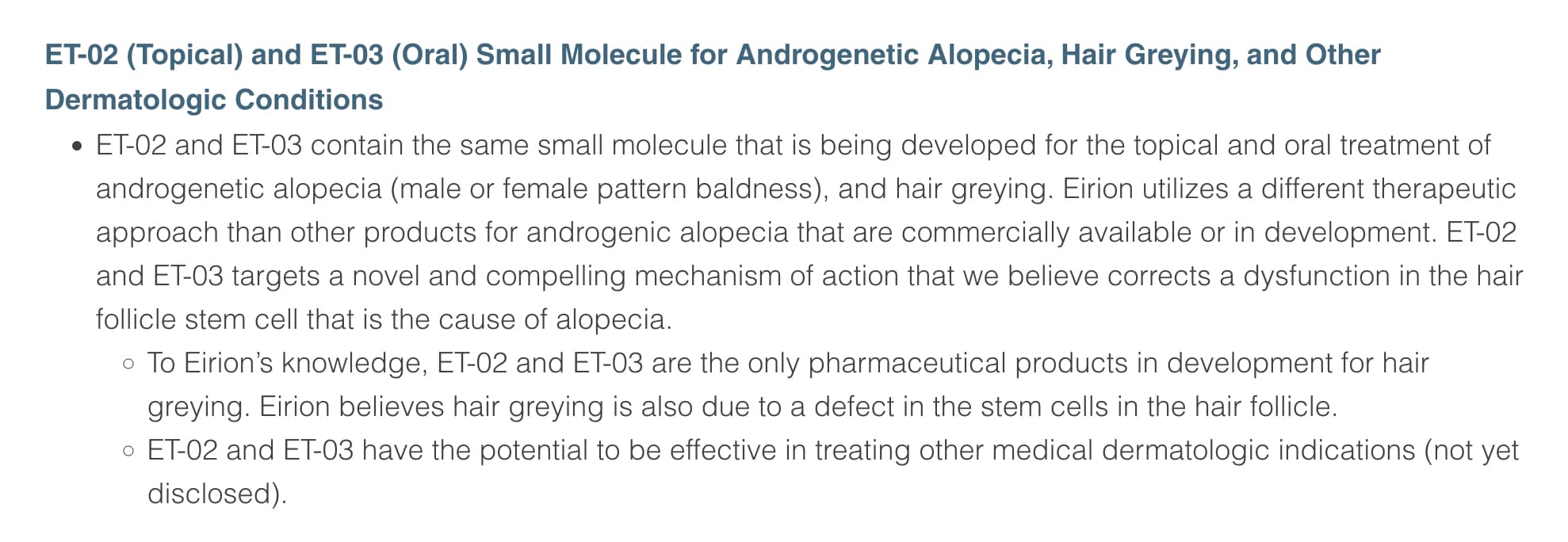
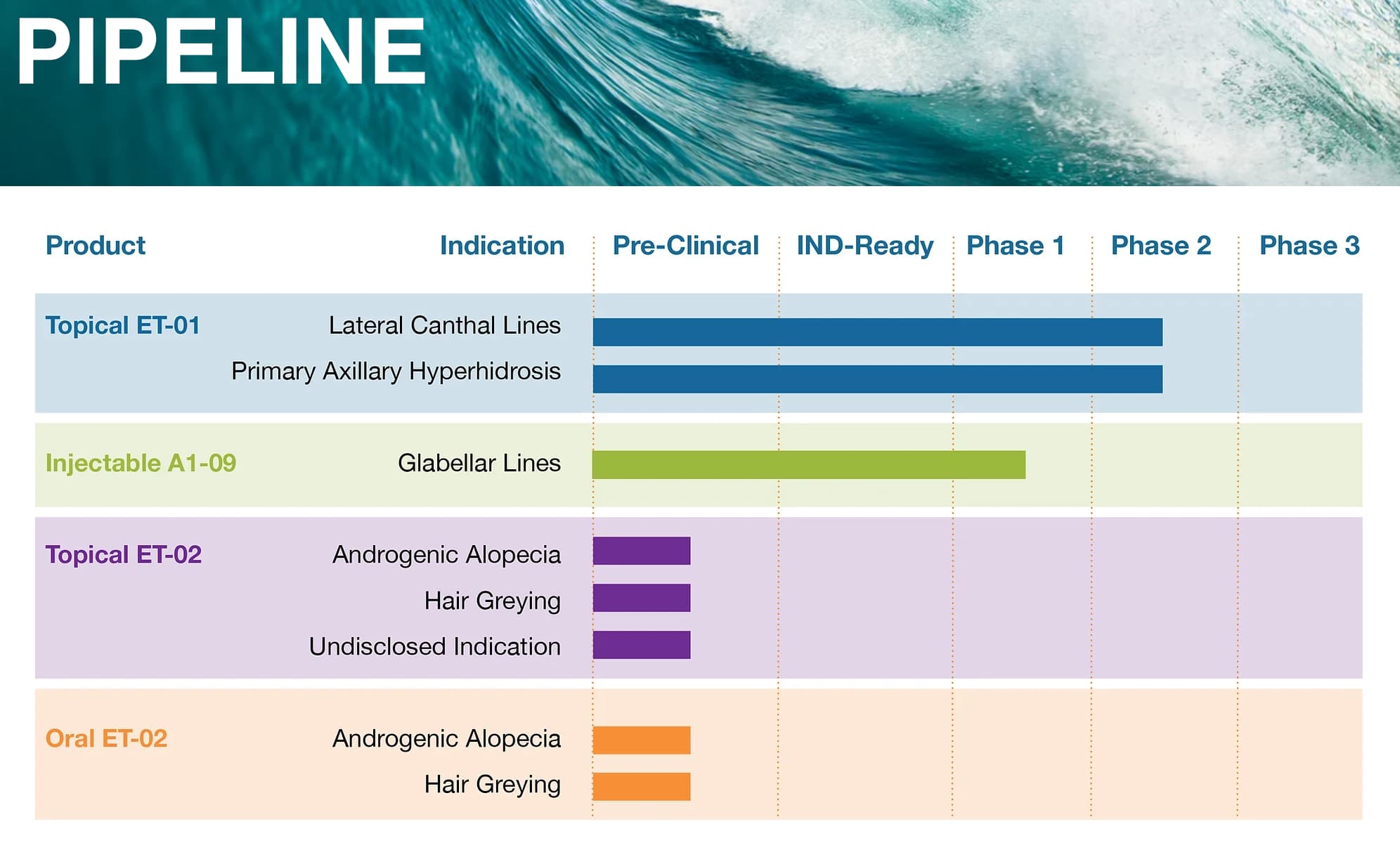
It seems like its still really early in their development program (and given the state of the biotech funding world (very bad) that may be a sign they are moving slowly : https://moonink6.wixsite.com/eirion/pipeline
If they really nail a efficient cure for gray hair, I reckon it’ll be the biggest medical game-changer since Viagra.