Thanks for posting this paper as I had not come across it before. I find this statement interesting:
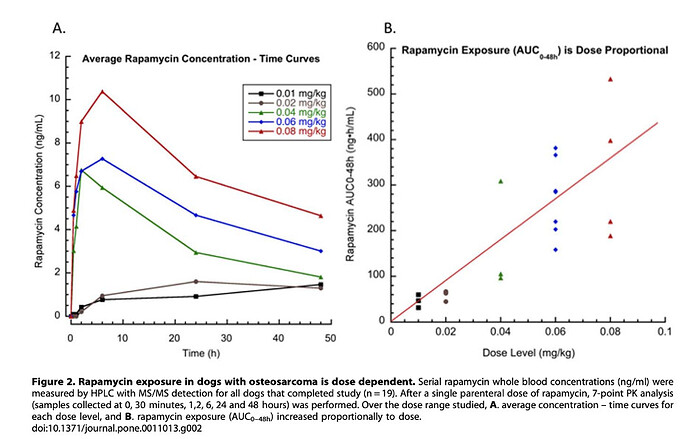
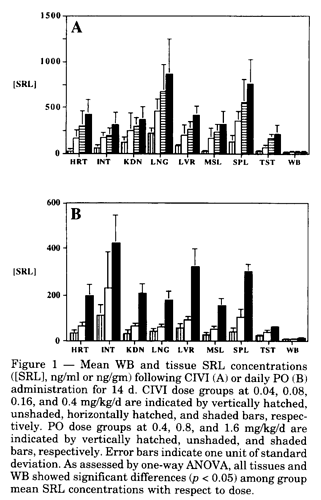
With regards to biodistribution, lipophilic Rapamune primarily partitions into red blood cells (95%) and then eventually accumulates in off-target organs, including the heart, kidneys, intestines, and testes,
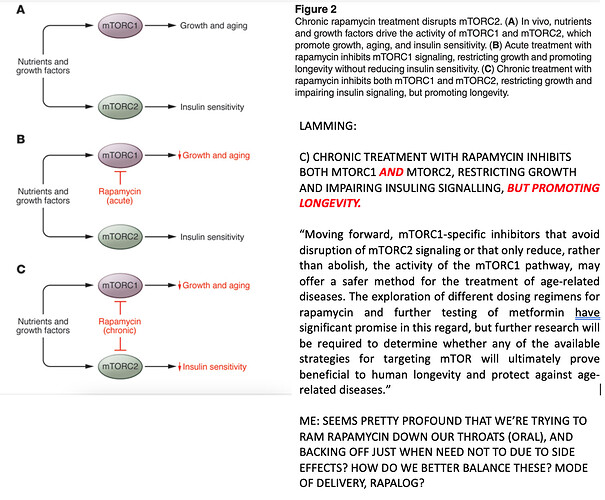
While the paper above is focused on the issue of “off-target” effects when delivered as part of a therapy for transplanted cells and tissue, we in the longevity community want (I suspect) rapamycin distributed to as many tissues and cells of the body, so the issue isn’t so much of “off-target” problems, but rather lack of the drug getting to some organs or cells enough so as to slow aging.
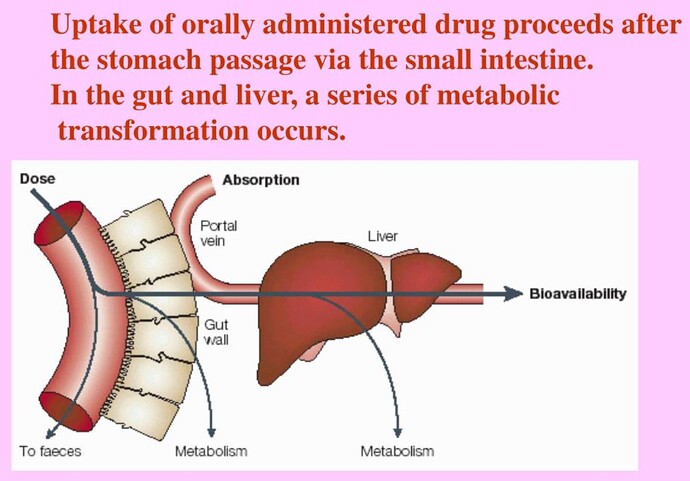
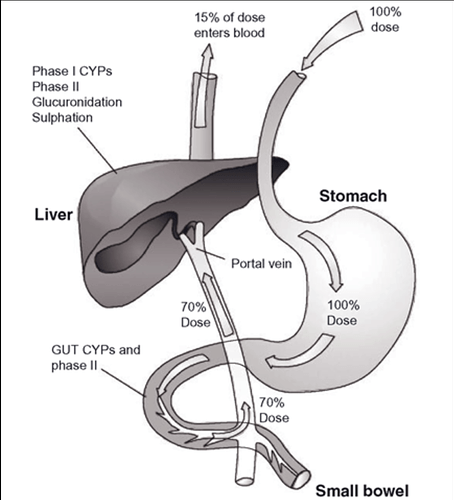
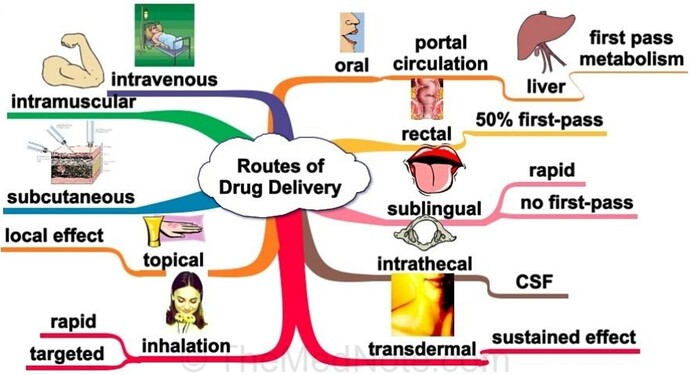
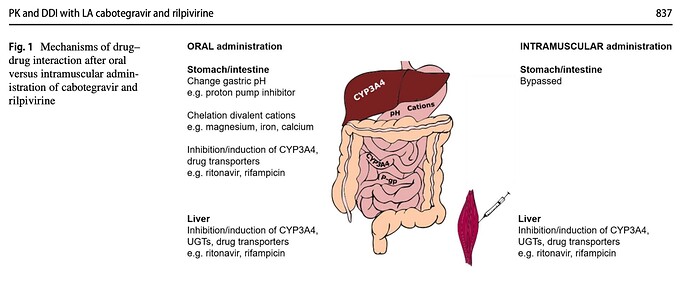
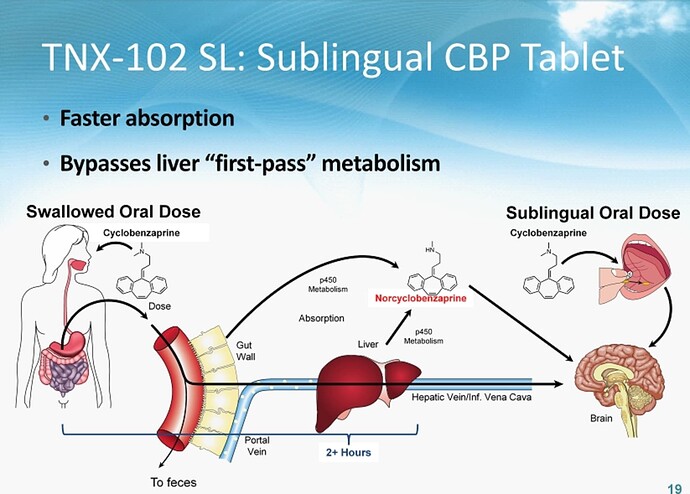
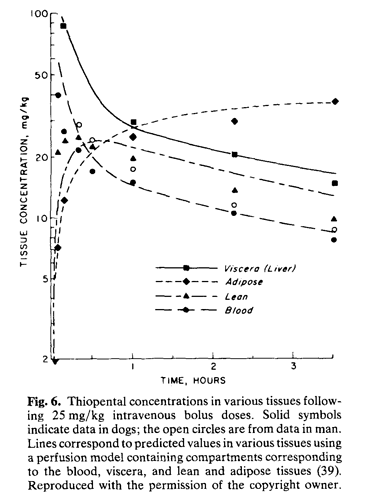
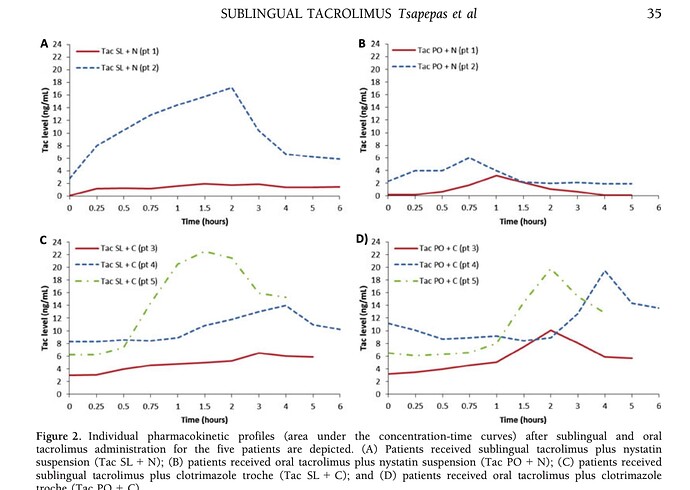
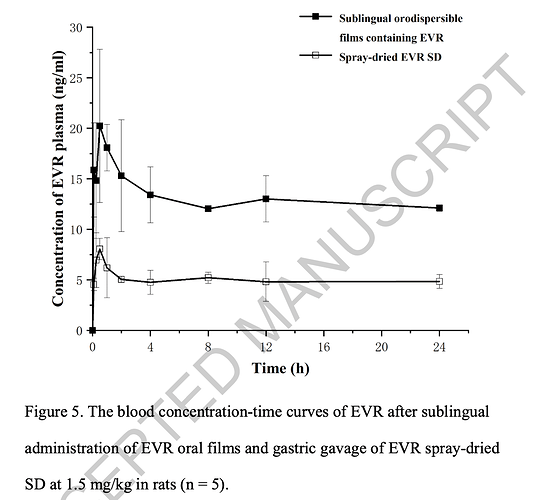
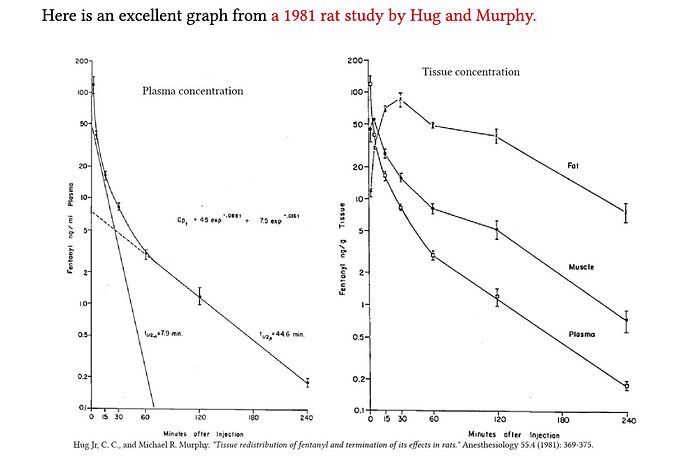
It seems that one of the issues we want to think about is that with oral (tablet-based) rapamycin there is a natural distribution pattern / effect throughout the body and I don’t know exactly what that distribution or effect pattern is. It would be interesting (for me at least) to better understand exactly where rapamycin is typically dispersed, and how well it gets into all the different tissue types, and organs. Perhaps different rapalogs have different distribution patterns?
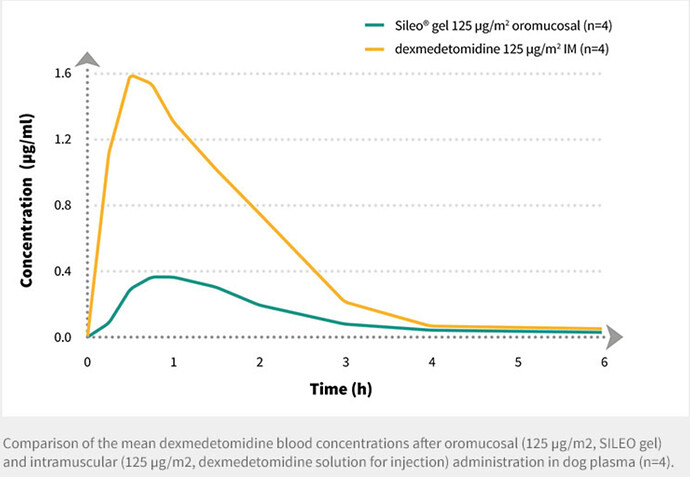
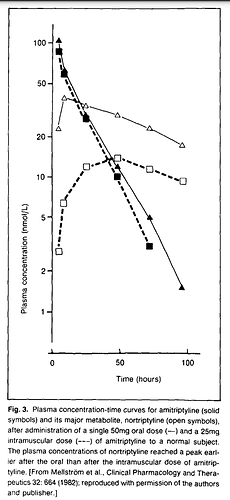
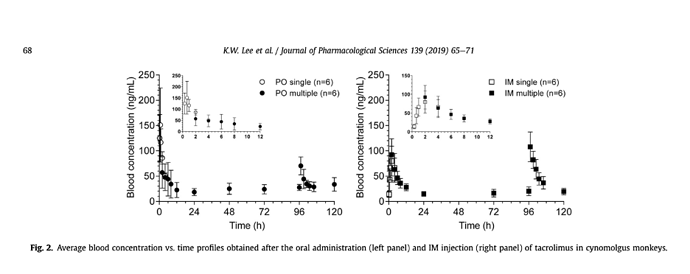
@MAC I know you are much less injection-adverse than I am - but it seems it would be interesting to understand and compare the distribution pattern of injectable rapamycin (rapalogs) like Temsirolimus. I wonder if they might be complimentary in terms of their benefits WRT organ and tissue distribution due to the different administration method and how it acts (more as a prodrug than simple mTOR inhibitor.
Temsirolimus also has a very short half life of 17 hours or so - about 70% shorter than rapamycin, so likely a much better side effect profile and lower risk of immune suppression.
Its a little hard to parse the Google Patent database to find out when Wyeth first patented Temsirolimus (Torisel) but it seems likely to have been in the late 1990s or early 2000s - in which case its soon going off-patent, if it hasn’t already. Not sure if the market is sufficiently large to justify a generic form… but researchers should be evaluating it for lifespan improvements. And of course, it would be great to know the lifespan effects of injection methods, vs. oral tablet rapamycin use, and different combinations of the rapalogs and administration approaches. So many avenues still to discover with this drug… and how to optimize its longevity effect.
My google patent search:
This patent did look interesting though: