Given the situation with the global shipments and new tariffs/taxes and duties on international products, and the fact that I’ve gotten used to the independence of being able to choose exactly what longevity medications I want to try, and when … with only minimal work with my doctor, I’m a little concerned about how long my current inventory of rapamycin will last.
We know that ketoconazole provides about a 5.6X multiplier effect on the bioavailability of rapamycin as outlined in this thread: Improve Bioavailability of Rapamycin (2)
So, I’ve decided to start using some Ketoconazole in my dosing program. It turns out I have a good amount of it because I purchased it for use in my DIY hair tonics I’ve been trying - so already have plenty of it to last a few years (at once per week dosing).
But, of course you have to be careful with Ketoconazole because of how it can also impact other medications you may be taking, or supplements.
So here is my approach that I’ve taken:
I looked at the Ketoconazole interactions with supplements to make sure there were no contraindications with anything I’m currently taking:
Yes — ketoconazole can affect certain supplements, mainly because it is both:
- A strong inhibitor of CYP3A4, the liver enzyme that metabolizes many compounds.
- A potent inhibitor of P-glycoprotein (P-gp), a transporter that pumps drugs and supplements out of cells (especially in the gut and brain).
- A drug with its own toxicity (notably to the liver), which can add to risks from hepatotoxic supplements.
Here’s a breakdown:
1. Supplements impacted via CYP3A4 inhibition
If a supplement is normally cleared by CYP3A4, ketoconazole can cause its levels to rise, increasing side effects. Examples include:
- St. John’s Wort (though this is more a CYP3A4 inducer; if someone stops St. John’s Wort while on ketoconazole, levels of other drugs/supplements can rise unpredictably).
- Resveratrol, quercetin, and other flavonoids — partially metabolized by CYP enzymes; ketoconazole could theoretically raise their levels.
- DHEA and other steroidal supplements — metabolized through CYP3A pathways; effects may be amplified.
2. Supplements impacted via P-gp inhibition
- Curcumin and berberine are substrates of P-gp. Inhibiting P-gp with ketoconazole may increase absorption and systemic exposure, potentially intensifying GI upset or liver stress.
- Coenzyme Q10 (CoQ10) and some polyphenols are also affected by P-gp; ketoconazole could raise bioavailability.
3. Liver toxicity overlap
Ketoconazole itself is hepatotoxic. Combining it with supplements that also stress the liver increases risk:
- Green tea extract (EGCG in high doses)
- Kava
- Black cohosh
- Red yeast rice (contains lovastatin-like compounds)
- High-dose niacin
These combinations can magnify liver enzyme elevations or, in rare cases, cause severe liver injury.
4. Other possible interactions
- Caffeine (common in pre-workouts, green tea, yerba mate) → levels may increase, leading to jitters or palpitations.
- Grapefruit-derived supplements (naringenin, bergamot) → already CYP3A4 inhibitors; combined with ketoconazole, they may over-amplify interactions.
Summary:
- Ketoconazole can raise blood levels of supplements metabolized by CYP3A4 or pumped by P-gp.
- The biggest practical concern is liver safety, since many herbal supplements already have hepatotoxic potential.
- Caution and monitoring are warranted if someone takes ketoconazole along with herbal extracts (curcumin, berberine, green tea extract, kava, red yeast rice, black cohosh, etc.) or hormonal supplements (DHEA, pregnenolone).
Then I checked my Statin’s potential for interaction:
Pravastatin and ketoconazole generally do not have a major interaction, unlike other statins such as simvastatin, lovastatin, or atorvastatin. Here’s why:
Mechanism
- Ketoconazole is a strong inhibitor of the CYP3A4 enzyme, which metabolizes many statins.
- Pravastatin, however, is not significantly metabolized by CYP3A4. It is primarily cleared through non-CYP pathways (such as sulfation and renal excretion).
Clinical significance
- Because pravastatin avoids CYP3A4 metabolism, the risk of increased blood levels (and muscle toxicity like myopathy/rhabdomyolysis) is much lower compared to other statins when taken with ketoconazole.
- There is no well-documented harmful interaction between pravastatin and ketoconazole in the major drug interaction databases.
Minor considerations
- Both drugs can affect the liver: pravastatin can rarely elevate liver enzymes, and ketoconazole is known for hepatotoxicity risk. Using them together doesn’t directly amplify metabolism-related risk, but periodic liver function monitoring is reasonable if combined.
- Always watch for general side effects of statins (muscle pain, weakness, dark urine), even if the interaction risk is low.
Summary:
Pravastatin and ketoconazole can generally be used together safely, with no major pharmacokinetic interaction expected. The main caution would be overlapping liver effects, so monitoring is prudent.
Ketoconazole impact on Empagliflozin (SGLT1 inhibitor)
let’s look at empagliflozin (Jardiance) with ketoconazole.
Metabolism of empagliflozin
- Empagliflozin is primarily cleared unchanged in urine and feces.
- Metabolism plays only a minor role. When it is metabolized, it goes mainly through UGT enzymes (glucuronidation, UGT2B7, UGT1A3, UGT1A8, UGT1A9).
- CYP enzymes (like CYP3A4) are not significant in empagliflozin metabolism.
Effect of ketoconazole
- Ketoconazole is a strong CYP3A4 inhibitor, but since empagliflozin is not CYP3A4 dependent, there’s no meaningful pharmacokinetic interaction.
- Clinical studies have shown that co-administration with CYP3A4 inhibitors (like ketoconazole or verapamil) does not significantly alter empagliflozin blood levels.
Practical considerations
- No dose adjustment of empagliflozin is recommended with ketoconazole.
- The main cautions with empagliflozin remain the usual ones: risk of urinary/genital infections, dehydration, hypotension, and rare ketoacidosis — but ketoconazole does not amplify these.
Summary:
No significant interaction exists between empagliflozin and ketoconazole, because empagliflozin is cleared mostly by glucuronidation and excretion, not by CYP3A4. Safe to use together without dose adjustment.
Would you like me to extend this and create a table of SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin, ertugliflozin) showing whether ketoconazole (or other CYP3A4 inhibitors) meaningfully affect each one?
And I did the same thing for all medications I take.
Then I dove more into the specific details on ketoconazole:
Ketoconazole has a relatively short plasma half-life:
- Initial distribution half-life: about 2 hours
- Terminal elimination half-life: usually 6–10 hours after a single dose
With repeated dosing, the half-life can become somewhat longer (around 8 hours), due to saturation of hepatic metabolism.
Because it is extensively metabolized in the liver (CYP3A4 substrate and inhibitor), clearance can vary depending on liver function and drug–drug interactions.
Do you want me to also give you a table comparing the half-life of ketoconazole to other common azole antifungals (like fluconazole, itraconazole, voriconazole) for context?
For oral ketoconazole, the T-max (time to reach peak plasma concentration) is typically:
- 1 to 2 hours after administration when taken with food (which enhances absorption).
- Absorption is reduced and sometimes delayed if taken on an empty stomach or with low gastric acidity (e.g., when combined with antacids, proton pump inhibitors, or H2 blockers).
So, under usual dosing conditions with food and normal gastric acidity, expect T-max ≈ 1–2 hours.
Would you like me to also put this into a PK summary table (half-life, T-max, bioavailability, metabolism, excretion) for ketoconazole?
So my action plan has been to:
- Take 200mg of ketoconazole with food about 1 hour prior to taking rapamycin
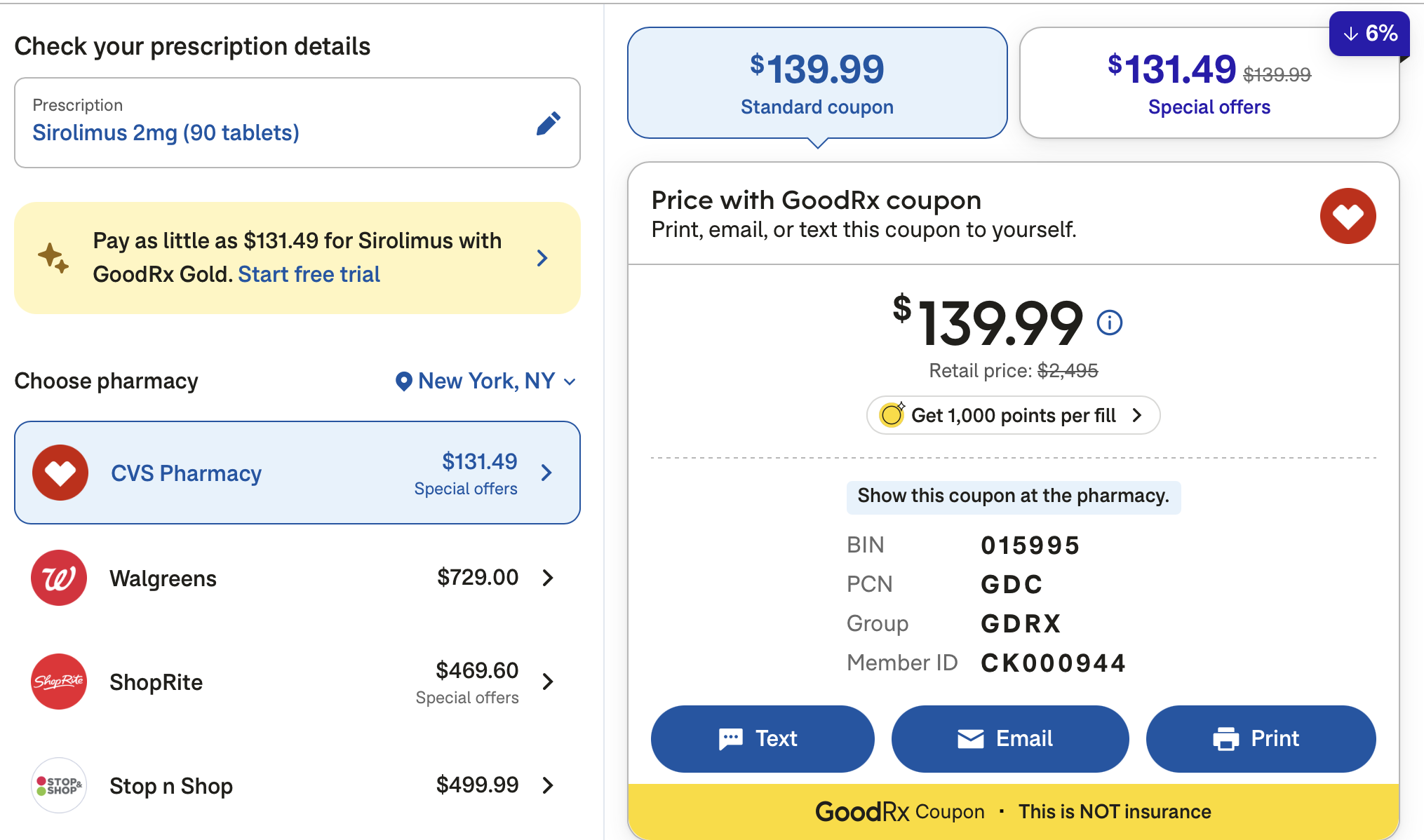
- Take 2mg of rapamycin, which should be equivalent to about 11mg regular rapamycin dosing.
Anyone else doing anything like this now, given the India shipment halt?