I don’t think any studies have been done to answer this question… at least I’ve not seen any.
This would be hard to measure. My approach and I probably take a higher dose than others, but very infrequently, is to be careful about increasing the dose. My last dose did not have any unusual side effects. Obviously I expect sleep disruption and high glucose etc and will probably be phoned by the lab when they find my WBC to be below 2G.
Also if I am getting sleep disruption I assume rapamycin is getting into the brain.
The only thing I ever heard was Blagosklonny’s position that a higher peak was better for passing the BBB. I assume that was a mechanistic assumption. I have followed a 2 week cycle with a “double dose” (~12-15mg) in part because of this position. I have no idea if it is right. I do not get sleep disruption as others report. I sleep better after a rapa dose.
Rapamycin doesn’t significantly cross the BBB. Why would higher doses help? (For sure, if 1% goes through the BBB and you take a mega dose, you’ll get some in the brain, but that will still be 1%.)
Kaeberlein… Attia all say the same. Hard to get anything across the BBB. And… personally… Blogsklonny might have been wrong about higher doses to achieve this.
Kaeberlein says that lowering inflammation at brain might be enough with the peripheral area of the brain getting benefits.
I recently came across this study: https://www.researchgate.net/publication/349295206_RapamycinSirolimus_Improves_the_Behavior_of_an_8-Year-_Old_Boy_With_Nonsyndromic_Autism_Spectrum_Disorder
Even though it is for a single person (child) and not a big group, it seems here rapamycin must have passed the BBB sufficiently to induce such a big change especially given the patient was given about 1mg daily continuous (low dose daily).
The only thing I can think of is ASD patients have been shown to have weaker BBB at times which might have helped rapamycin get in, though it might not be the case here, as if the symptoms improved then the BBB should have also gotten stronger so it wouldnt have been a continuous improvement as seen in the study
Rapamycin need not cross the BBB for it to have an immediate and profound impact on the brain. Note the case of klotho. In the Peter Attia podcast on klotho, his guest, the scientist who conducted klotho studies, discussed the impact of klotho on the brain. Klotho does not cross the BBB. Yet in her studies in mice there is a profound effect of klotho on the brain function within four hours of administration, measurable by rigorous functional tests. The effects are apparently mediated by klotho altering blood factors, platelet activation in particular, which then cross the BBB and affect the brain.
In other words, you don’t need to have a drug/molecule cross the BBB to rapidly and strongly impact the brain, it can do so by modifying other factors which subsequently do cross the BBB and impact the brain. It is possible that rapamycin might work in a similar way, not by directly crossing the BBB, it can modify some other factors and thus affect the brain. Obviously I’m speculating, but the point is that crossing the BBB is not the deciding factor in evaluating the impact of any given molecule on the brain.
One interesting thing I learned about ketoconazole is that it inhibits P-glycoprotein (P-gp), a key efflux transporter at the BBB. Since sirolimus is a substrate of P-gp, ketoconazole is thought to increase sirolimus penetration into the brain by reducing its efflux. So in addition to ketoconazole’s effects on CYP3A4, it may also aid in raising sirolimus levels in the brain. I’m currently experimenting with a once every 21-day dose of 6mg sirolimus with 200mg ketoconazole (taken two hours prior). I plan to share my results so far in a separate post, but compared to weekly dosing with GFJ+EVOO, the difference is quite remarkable.
This successful trial of an immunosuppressant drug in PD shows that compounds that do NOT cross the BBB can still have a beneficial impact: Parkinson's disease - #730 by adssx
What do you make of this paper?
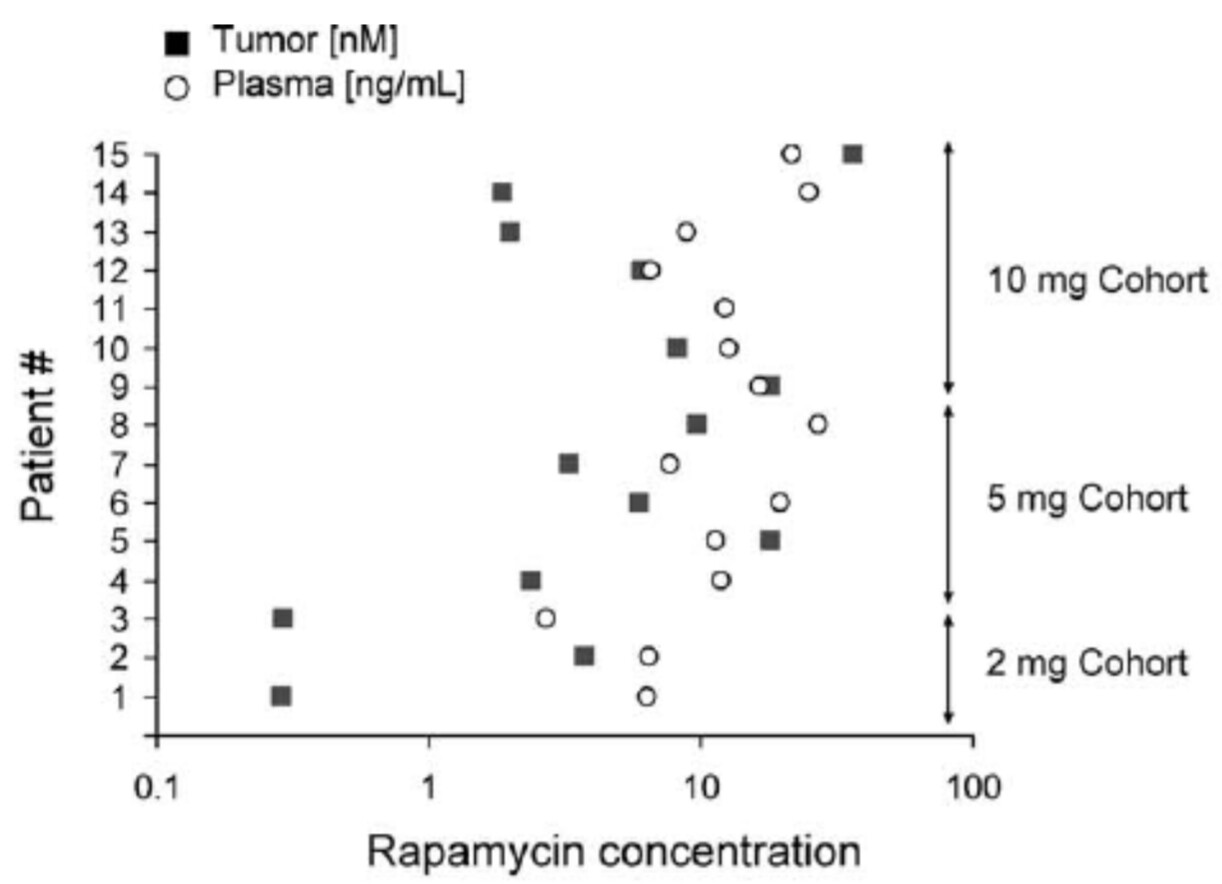
Looks like there is a huge individual variability but it clearly crossed the BBB.
The rapamycin doses are huge though: 2mg to 10mg per day for 7.5 days
For several patient the tumor concentration was 10+ times less than the plasma concentration but it’s better than nothing. Other patients had a higher concentration in the tumor than in the serum though.
Because rapamycin is a macrolide natural product whose
size could prevent distribution across the blood–brain
barrier, we measured rapamycin concentrations by mass
spectrometry in an aliquot of tumor tissue obtained at S2.
Rapamycin was detected in 14 of 14 tumors (insufficient
tissue was available from patient 11) at concentrations
ranging from 0.3–36.3 nM.
- They found: “Although intratumoral rapamycin concentrations that were sufficient to inhibit mTOR in vitro were achieved in all patients, the magnitude of mTOR inhibition in tumor cells (measured by reduced ribosomal S6 protein phosphorylation) varied substantially. Tumor cell proliferation (measured by Ki-67 staining) was dramatically reduced in seven of 14 patients after 1 wk of rapamycin treatment and was associated with the magnitude of mTOR inhibition (p ¼ 0.0047, Fisher exact test) but not the intratumoral rapamycin concentration. (PDF) Antitumor Activity of Rapamycin in a Phase I Trial for Patients with Recurrent PTEN-Deficient Glioblastoma.”
- More recent trials didn’t find rapa in CSF or brain mTOR engagement (see: Rapamycin and the Issue of Getting Through the Blood Brain Barrier - #45 by adssx & Rapamycin and the Issue of Getting Through the Blood Brain Barrier - #59 by alexvpickering )
- This recent paper (Exosomal delivery of rapamycin modulates blood-brain barrier penetration and VEGF axis in glioblastoma) citing that 2008 one says: “the drug’s limited ability to penetrate the BBB”.
Crossing the BBB is not a black or white issue, it’s a %. And besides the crossing, we want to know if rapamycin can engage with brain mTOR. As of today, there is no evidence that sirolimus significantly engages with brain mTOR as doses typically used for longevity.
Quick update: I’ve been increasing the dose from 6mg (w/ 200mg ketoconazole two hours prior) to 7mg and now 8mg along with giving my body more time to clear between doses (now every four weeks instead of three), and let me say, the word remarkable is an understatement. All inflammatory biomarkers (hs-CRP, ESR, etc.) have reached lows that even my doctor is astonished by…all signs/symptoms of inflammation in my body are gone…no joint aches, old injuries don’t bother me while resistance training, zero brain fog, etc. CBC was also optimal when recently tested at the trough. I need to get sirolimus levels tested again soon, but I’ll be sticking with this protocol for the coming months based on these changes. I think there is something to be said for spiking levels intermittently to as high as one can tolerate versus low(er) weekly dosing. In the case of using 8mg alongside ketoconazole, I would guess the equivalent dose of rapamycin is at least 5x (40mg), potentially higher. I also have had zero side effects (lipids and glucose are perfect) other than tiredness for 1-2 days after the dose.
Potential solution to the problem? Monepantel: a brain-penetrant mTOR inhibitor (cross posting to get more feedback)
Matt said that rapamycin inhibits brain mTOR in mice. He’s interested (2 weeks ago) in the results of the ERAP trial of 7 mg/weekly for 6 months in early AD whether it is has effects, is detected in CSF, among other things (but mentioned that it can inhibit brain mTOR without crossing the BBB):
Support for cerebral target engagement (i.e. mTOR inhibition) in humans comes from the use of rapamycin as a first-line treatment for the cerebral manifestations of TSC [51]. TSC is a genetic disorder that activates the mTOR pathway, leading to the growth of benign tumors in various organs, including the brain. Inhibition of mTOR with rapamycin analogues is the only approved pharmacological treatment of the disease, and the only feasible mechanism of action is mTOR inhibition in cells behind the BBB.
I think we should keep the focus on one thing: brain mTOR inhibition, that’s where confusion might come from. Whether it crosses the BBB or not to do that. In that case, Rapamycin might work considering treatment for TSC, and same for everolimus? (With regards to inhibiting brain mTOR). The mechanism basically of systemic mTOR inhibition inhibiting brain mTOR is interesting (that Matt brought up, among other things).
I recall reading a human study a while ago iirc where they used rapamycin daily (around transplant use doses) for brain tumours and later when the tumour was removed they studied it and found it to contain rapamycin particles.
I actually think that daily dosing probably inhibits mTOR in the brain better than very high dose intermittent (so 2mg daily compared to 20mg weekly/biweekly). As ultimately what matters is the average blood sirolimus level (ng/ml) over a given period. There was also a similar everolimus study posted in this forum before but we know that everolimus passes bbb easier than rapamycin.
I wonder if the TSC human studies will be of any help in knowing whether rapamycin affects human brain mTOR. We already know it changes the response to ketamine in humans.
The MSA trial found no brain mTOR inhibition with daily rapamycin.
In the discussion section they concluded it could be that, or that brain mTOR inhibition doesn’t affect MSA:
We found no evidence that oral sirolimus has any clinical or biomarker effect in patients with MSA. Potential explanations for this include that the mTOR-autophagy pathway is not essential in synucleinopathies, that the burden of synucleinopathy in patients with probable MSA is too high to be impacted by autophagy inhibitors, and that CNS biodistribution and target engagement were poor. Unfortunately, our study did not include CSF sirolimus levels or putative autophagy-related biomarkers, which could have provided information on the CNS activity of sirolimus.
I don’t understand how mTOR inhibitors shrink brain tumors (SEGA) or glioma in TSC (that’s from upregulated mTORC1), and are FDA approved for this, if it wasn’t from brain mTOR inhibition:
When either TSC1 or TSC2 is deficient, mTOR complex 1 is constitutively up-regulated, leading to abnormal cellular growth, proliferation, and protein synthesis.
https://www.nejm.org/doi/full/10.1056/NEJMoa1001671
Check their later paper. Their measured brain mTOR engagement and found none.