One of my major parallel hacks. Actually, the author is the one who got me onto this intervention years ago. And it’s easy and free, just like exercise.
Multivariate genomic scan implicates novel loci and haem metabolism in human ageing
“The strong signal for haem metabolism, in combination with the MR results, suggests the evidence for the involvement of this pathway in human ageing is reasonably robust. Haem synthesis declines with age and its deficiency leads to iron accumulation, oxidative stress, and mitochondrial dysfunction. In turn, iron accumulation helps pathogens to sustain an infection, which is in line with the known increase in infection susceptibility with age. In the brain, abnormal iron homeostasis is commonly seen in neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease and multiple sclerosis. Plasma ferritin concentration, a proxy for iron accumulation when unadjusted for plasma iron levels, has been associated with premature mortality in observational studies, and has been linked to liver disease, osteoarthritis, and systemic inflammation in MR studies”
Heme/Haem: Heme - Wikipedia
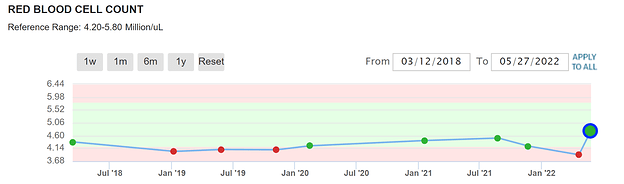
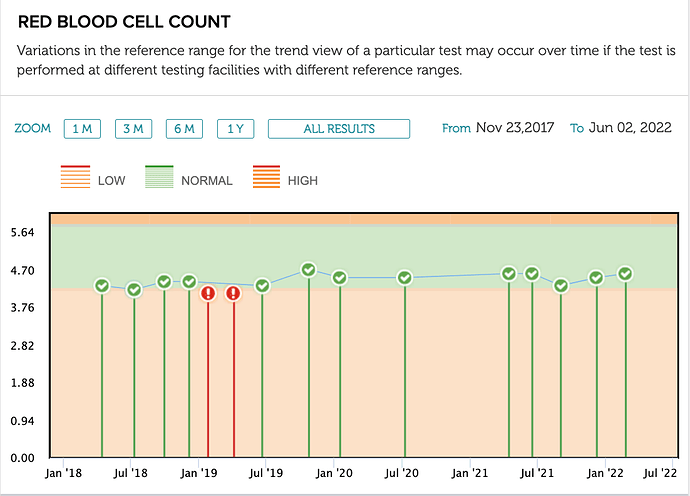
Haven’t read the book, but regularly donating blood to the Red Cross keeps my blood just above the anemic level. After my first 3 months of rapamycin, I dipped into the anemic
range. I started taking beet juice extract, B12, and folic acid. My latest test just put me back into the low normal range. So, now I will start donating blood again.
Interesting, keep us posted. Any side effects of your anemic definition threshold?
No, I don’t feel anything that I know of from having a relatively low RBC because I don’t have anything to compare it with. I have always been on the low side of normal.
The latest dip was after taking higher doses of rapamycin, 10 - 20mg w/GFJ. I don’t know for sure if it was caused by rapamycin. Anyway, I boosted my RBC by taking B12, folic acid, and beet juice extract. It worked quite quickly.
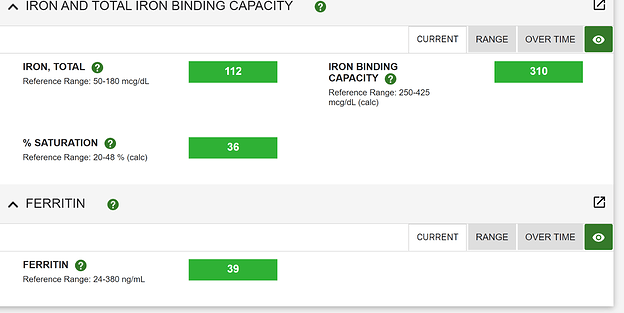
I am using a multi-parameter indication for “iron and anemia” management (no RBC):
Iron depletion: serum ferritin less than 20 µgr/dl.
Lack of iron stores: serum ferritin less than 12 µgr/dl.
Iron Deficiency: serum ferritin less than 12 µgr/dl and transferin saturation percentage less than 15.
Iron deficiency anemia: serum ferritin less than 12 µgr/dl, transferin saturation percentage less
than 15, and Hb less than 14 mg/dl.
Donating on a 7 week schedule, whilst taking Rapamycin, I am just hovering above these thresholds, with no “apparent” impact on my energy/exercise baseline.
I don’t even look at RBC, although I did dip below cutoff couple of years ago, but this was before Rapamycin. I definitely hover just above low cutoff. Started Rapamycin Jan '21.
As I bump my Rapamycin, will be interesting to watch these markers.
Your RBC levels appear to be similar to mine. I just donated a pint to the Red Cross this morning. While they don’t tell me my actual iron levels they check to see if it is too low.
Once or twice over the years, it has been too low. Today it was “normal”.
I rarely see my doctor except for my annual physical. He rarely checks anything but the most common blood tests, though I did get him to request a ferritin level test last time.
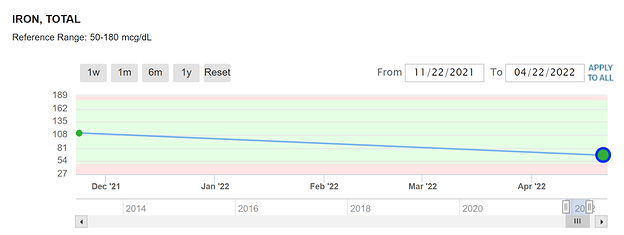
Mac. I just started in Nov 21, donating blood every two months (similar to your schedule). Have not noticed impact on energy levels either.
I think you have iron to dump yet based on your saturation, and other iron markers.
I won’t even go down the other health benefit pathways of dumping “old” signalling molecules, glycated albumin, reducing blood viscosity, and more…
There’s a whole other longevity world in plasma replacement/dilution.
Donating blood only achieves perhaps 10-15% of full on plasma exchange, but it yields a myriad of other health benefits, and is implicated universally in human aging.
My philosophy is to stack as many interventions on top of each other as possible.
MAC, you write: “my philosophy is to stack as many interventions on top of each other as possible.” You will to share your “stack”? Very interested in what you do for longevity. Also, how old are you? I think you shared this in another post but can’t recall. Thanks
MAC, you also write: “I think you have iron to dump yet based on your saturation, and other iron markers.” Can you explain further? Besides donating blood, any other ways to get rid of excess iron?
I read where Tumeric supplementation (500 to 2000 mg a day) can help rid body of excess iron. Thoughts?
Daily exercise resistance/aerobic
Strict keto (plant fat based), one meal a day fasting
7 week phlebotomy
Stack of supplements (D, Mag, Zinc, K1/K2, etc with anti inflammatory skew)
Exogenous Testosterone (male, 57)*
Rapamycin
DHEA
Cialis 5 mg/day (PDE5 inhibitors for neurodegenerative/vascular)
Socially engaged
Almost no alcohol (once/week red wine)
- my functional medicine doctor is very big on this for men and longevity/cognitive
MAC. This is helpful. I also don’t touch alcohol. Never have. I also do one meal a day fasting. Why DHEA and how much?
Borrowing from an iron forum summary:
First on Ferritin:
Serum ferritin is a test that was formerly thought to be directly related to the amount of tissue ferritin, and thus, something that could be used to measure the amount of stored iron, which was believed to always be stored bound to ferritin. Today, modern research has shown that actually, serum ferritin levels are not related to tissue ferritin levels, and that iron is only stored bound to ferritin in tissues that produce ferritin, like the liver, and is stored in free molecule form in other tissues, like cardiac muscle, that do not produce ferritin. There is no required serum ferritin level; you do not need to be concerned about “depleting” it.
Transferrin Saturation %:
Transferrin saturation is the indicator of excess iron storage, and needs to be below 40% in everyone, more especially those individuals who have HH. When transferrin saturation is over
40%, which indicates that iron storage sites around the body have reached their normal capacity, two things happen. One, is the liver releases the HFE protein (starting when %TS is over 20%),
which is supposed to bind with receptors in other cells, stimulating the release of hepcidin, which in turn binds with receptors in intestinal cells, halting the absorption and release into the blood stream of iron molecules. The second one is the reason that 40% was chosen as the threshold - at 40%, there’s not enough transferrin to bind with all of the iron being secreted to the bloodstream by the intestinal cells, causing free iron molecules to circulate in the bloodstream, getting deposited wherever they can, where they act as free radicals, causing damage
When deironing, the removal of red blood cells via phlebotomy results in increased RBC manufacture in the bone marrow, which picks up iron from the transferrin and uses it to make hemoglobin. This results in a temporary lowering of %TS - which then rises again as tissues release stored iron, which binds with the transferrin, once again increasing saturation. As phlebotomies continue during de ironing, this continues to occur until finally all excess stored iron is gone from tissues. In order to coax all of the excess stored iron out, the transferrín saturation must be low - which is why the target during de ironing is 20% or lower. Once deironed, the thing to watch out for is transferrin saturation over 40%, which signals the start of iron loading and damage from free iron molecules. Some people with HH (wonky iron genes) have adverse reactions once transferrin saturation enters the “normal reference range”, which starts at 15% for women, 20% for men. Which is why, those with HH, should try to keep my %TS as low as possible. It’s also important to note that there is no such thing as a too low %TS. Instead, you would do a CBC to check the Red Blood Cell counts, and hemoglobin levels - if they are normal, then RBC manufacturing is taking place normally which means your body has sufficient iron for its use.
Besides phlebotomy, there is chelation:
https://irondisorders.org/chelation-therapy/
Then there are dietary pathways to removal:
Re DHEA:
25 mg, twice a day
I think in the US, it’s an over the counter supplement, but a regulated med in Canada.
Rapamycin has done many things for me, but it has not increased my energy levels. (Perhaps I am too old for anything to do that.)
What has your personal subjective, objective benefits been?
I really would like to explore the benefits of DHEA. Somewhere, unfortunately, I can no longer find it, I read that the lack of conclusive results of DHEA supplementation was due to the study doses being way too small and the studies not being carried out long enough. There is also some confusion as to measuring DHEA serum levels as opposed to cellular levels as we find with some other supplements.
My take away from what I have read so far is that the usual dosages are too small and the dangers are over-emphasized.
This is a good article with many references:
The Case for DHEA
EDITORIAL
Dehydroepiandrosterone (DHEA): A Fountain of Youth?
“Very large doses of DHEA have demonstrated antitumoral
effects as underlined by A Schwartz et al. in ref. 6 and 7,
provoking prevention and / or regression in spontaneous or
chemically induced skin and colon cancers, in specific strains
of rodents. Independently, a few reports have suggested low
production of DHEA(S) in women at risk of/or having breast
cancer.”
“Serum DHEA and Its Sulfate Are Associated With Incident Fall Risk in Older Men: The MrOS Sweden Study”
I left this reply here because I think it is of general interest to rapamycin users.
I have to go back in my notes, but I think the DHEA my doc has added is part of supporting the overall hormonal axis.
MAC, you wrote:
"That’s very low saturation, and based on your elevated other iron markers, appears you do have iron absorption issues. Do you have iron labs before Rapamycin? Have you checked for any wonky iron genes? Family history?
I am going to surmise it’s not do to Rapamycin, given discordance in markers."
I’m repeating my iron numbers below:
“My recent labs were all pretty good in terms of CBC, CMP, Lipids, Insulin. However, my ferritin was low (24 with range of 30 to 400); my TIBC was high (499 with range of 250-400); my UIBC was high (437 with range of 111-343); and my Iron Sat was low (12 with range of 15-55).” I did not give you my IRON reading. It was 62 in a range of 38-169.
Question. These numbers suggest to you I have iron storage I need to get rid of? If so, explain. Also, which of these numbers in the iron panel do you consider the most important to suggest one has enough iron but not too much?
To answer your question above, years ago, I did a battery of tests with a hematologist (given my Dad had a number of blood clotting disorders) and all were negative.
Thanks for your time.