MAC. This is helpful. I also don’t touch alcohol. Never have. I also do one meal a day fasting. Why DHEA and how much?
Borrowing from an iron forum summary:
First on Ferritin:
Serum ferritin is a test that was formerly thought to be directly related to the amount of tissue ferritin, and thus, something that could be used to measure the amount of stored iron, which was believed to always be stored bound to ferritin. Today, modern research has shown that actually, serum ferritin levels are not related to tissue ferritin levels, and that iron is only stored bound to ferritin in tissues that produce ferritin, like the liver, and is stored in free molecule form in other tissues, like cardiac muscle, that do not produce ferritin. There is no required serum ferritin level; you do not need to be concerned about “depleting” it.
Transferrin Saturation %:
Transferrin saturation is the indicator of excess iron storage, and needs to be below 40% in everyone, more especially those individuals who have HH. When transferrin saturation is over
40%, which indicates that iron storage sites around the body have reached their normal capacity, two things happen. One, is the liver releases the HFE protein (starting when %TS is over 20%),
which is supposed to bind with receptors in other cells, stimulating the release of hepcidin, which in turn binds with receptors in intestinal cells, halting the absorption and release into the blood stream of iron molecules. The second one is the reason that 40% was chosen as the threshold - at 40%, there’s not enough transferrin to bind with all of the iron being secreted to the bloodstream by the intestinal cells, causing free iron molecules to circulate in the bloodstream, getting deposited wherever they can, where they act as free radicals, causing damage
When deironing, the removal of red blood cells via phlebotomy results in increased RBC manufacture in the bone marrow, which picks up iron from the transferrin and uses it to make hemoglobin. This results in a temporary lowering of %TS - which then rises again as tissues release stored iron, which binds with the transferrin, once again increasing saturation. As phlebotomies continue during de ironing, this continues to occur until finally all excess stored iron is gone from tissues. In order to coax all of the excess stored iron out, the transferrín saturation must be low - which is why the target during de ironing is 20% or lower. Once deironed, the thing to watch out for is transferrin saturation over 40%, which signals the start of iron loading and damage from free iron molecules. Some people with HH (wonky iron genes) have adverse reactions once transferrin saturation enters the “normal reference range”, which starts at 15% for women, 20% for men. Which is why, those with HH, should try to keep my %TS as low as possible. It’s also important to note that there is no such thing as a too low %TS. Instead, you would do a CBC to check the Red Blood Cell counts, and hemoglobin levels - if they are normal, then RBC manufacturing is taking place normally which means your body has sufficient iron for its use.
Besides phlebotomy, there is chelation:
https://irondisorders.org/chelation-therapy/
Then there are dietary pathways to removal:
Re DHEA:
25 mg, twice a day
I think in the US, it’s an over the counter supplement, but a regulated med in Canada.
Rapamycin has done many things for me, but it has not increased my energy levels. (Perhaps I am too old for anything to do that.)
What has your personal subjective, objective benefits been?
I really would like to explore the benefits of DHEA. Somewhere, unfortunately, I can no longer find it, I read that the lack of conclusive results of DHEA supplementation was due to the study doses being way too small and the studies not being carried out long enough. There is also some confusion as to measuring DHEA serum levels as opposed to cellular levels as we find with some other supplements.
My take away from what I have read so far is that the usual dosages are too small and the dangers are over-emphasized.
This is a good article with many references:
The Case for DHEA
EDITORIAL
Dehydroepiandrosterone (DHEA): A Fountain of Youth?
“Very large doses of DHEA have demonstrated antitumoral
effects as underlined by A Schwartz et al. in ref. 6 and 7,
provoking prevention and / or regression in spontaneous or
chemically induced skin and colon cancers, in specific strains
of rodents. Independently, a few reports have suggested low
production of DHEA(S) in women at risk of/or having breast
cancer.”
“Serum DHEA and Its Sulfate Are Associated With Incident Fall Risk in Older Men: The MrOS Sweden Study”
I left this reply here because I think it is of general interest to rapamycin users.
I have to go back in my notes, but I think the DHEA my doc has added is part of supporting the overall hormonal axis.
MAC, you wrote:
"That’s very low saturation, and based on your elevated other iron markers, appears you do have iron absorption issues. Do you have iron labs before Rapamycin? Have you checked for any wonky iron genes? Family history?
I am going to surmise it’s not do to Rapamycin, given discordance in markers."
I’m repeating my iron numbers below:
“My recent labs were all pretty good in terms of CBC, CMP, Lipids, Insulin. However, my ferritin was low (24 with range of 30 to 400); my TIBC was high (499 with range of 250-400); my UIBC was high (437 with range of 111-343); and my Iron Sat was low (12 with range of 15-55).” I did not give you my IRON reading. It was 62 in a range of 38-169.
Question. These numbers suggest to you I have iron storage I need to get rid of? If so, explain. Also, which of these numbers in the iron panel do you consider the most important to suggest one has enough iron but not too much?
To answer your question above, years ago, I did a battery of tests with a hematologist (given my Dad had a number of blood clotting disorders) and all were negative.
Thanks for your time.
Taking a closer look, considering your very low TS and high TIBC, blood donations, and vegan like diet, appears you are iron deficient (look iron at definitions above)
Suggest you stop donating for now, take Vitamin C, consider iron supplement, rebuild your iron stores.
Review all this with your healthcare professional. I am not qualified to offer medical advice.
MAC. This is quite helpful. I know you are not a medical doctor so no worries there. Your reply helps me better understand the situation and thus better able to discuss with my PCP.
Keep up the great artistry.
Thanks
I really like this article because it explains things that a layman can understand.
So, the main thought is iron is one of the primary causes of aging?
“It can be seen from all of the above that iron is a common theme in many if not most life-extension interventions.”
Yes, I have come to believe iron is implicated in many aging pathways. Beyond the physiological minimum (just above anemia), the excess is just harmful. And now we see the benefits of say phlebotomy and rejuvenating the proteome.
Iron has underlying support in other lifespan extending interventions. CR and low protein (say low animal protein) is essentially low heme iron. Eating less red meat is eating less heme iron. Vegan/vegetarian diet is low heme iron. Women generally liver longer vs men…less iron stores over a lifetime.
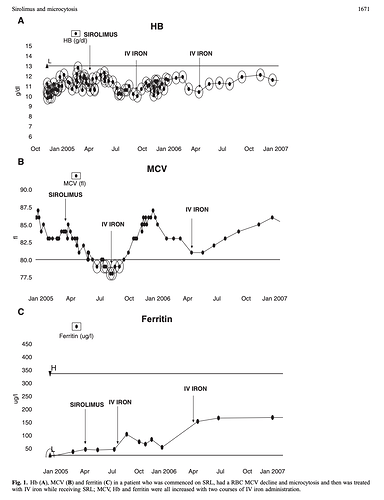
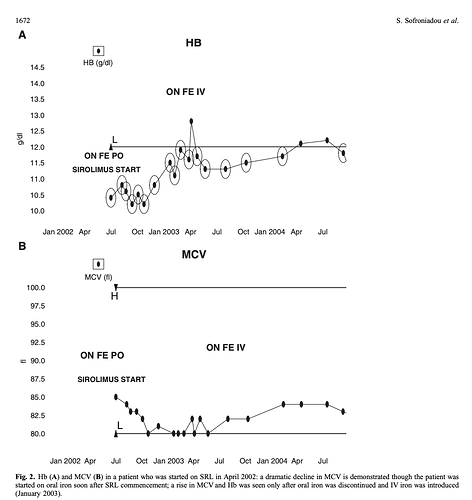
Here’s a little gem paper on Rapamycin, RBC MCV, and iron supplementation (2010).
It would appear that for those crossing into significant RBC microcytosis* (in this paper, chronic Rapamycin dosing cancer patients), iron supplementation WILL reverse. But ONLY IV iron, NOT oral, indicative of some form of gastro/liver Fe dysregulation by Rapamycin.
*“The RBC MCV exhibited a significant gradual decline within 1 month after SRL commencement until the end of the observation period (24 months). During this interval, the mean MCV fell from 91.0 fl at time point −1 to 82.0 fl at time point 24”
Where I am at, my lab range for MCV is 80-98 fl.
"In conclusion, our results suggest that SRL-based immunosuppression cause early, profound and sustained RBC microcytosis that is reversed after drug discontinuation. This microcytosis is independent in time and degree from SRL-induced anaemia. The factors that correlate with MCV decline and microcytosis appearance are SRL levels and utilization of IV iron; the former having a negative impact and the latter a positive one. Both of these findings are novel ones. The fact that IV iron utilization was shown to be the only independent predictor of the MCV change despite the effect of SRL levels probably indicates a functional iron-deficient state induced by SRL. We feel that functional iron deficiency is the possible mechanism for SRL-induced microcytosis development probably reflecting the impact of SRL on hepcidin, but further ideally prospective studies are warranted to clarify the underlying pathogenetic pathways. Understanding the impact of mTOR on iron pathways may throw new light on this fascinating class of drugs, while also spare patients from invasive procedures to investigate ‘chronic iron loss states’.
Yes, this is the same data that I highlighted in the exercise thread.
I noted that runners (serious competitive runners) often have low iron and that its thought that they lose much of it through sweat. I spiked in serum iron due to the combo of eating liver, switching to an iron skillet, taking vitamin C, and stopping saunas with my gym closed for C19.
Luckily when i saw my blood panel results it was spring and i could start running again. My gym sauna opened again and I went for 40 minute sessions at 180 F degrees. These two factors combined with giving the skillet away and greatly reducing organ meats brought my iron waaay down.
I also donate blood now and try to keep TS around 20%
PPIs and antacids can reduce iron absorption. And bleeding in the GI tract from ulcers can reduce iron levels.
I thought I would mention this just because of how common it is.
I got a hair tissue mineral analysis a couple years ago from evenbetternow.com . It says my copper is nearly in the low and iron is nearly in the high, the ratio they have as dangerous. Never really noticed it before since they were both in the acceptable range. I need to up my copper. Thanks guys.
Never would have noticed this.
Great that you found this so you could correct. There’s an independent researcher (not affiliated with any university or research lab) who, out of curiosity, went way down a rabbit hole on iron metabolism. He says he read about 3,000 papers to figure it out. His conclusion was the importance of primarily copper and secondarily retinol to allow for the healthy recycling of iron. Without copper excess iron will get stored in tissues.
Here’s a recent interview he gave on a podcast.
What dose of copper is recommended?
I take 2mg of copper bisgycinate chelate about 3 times a week. I also eat beef liver once a week. This keeps my serum level a little above 100.
Everyone is different so researching it, experimenting with how you feel and doing a blood test for levels is a good approach.
Thank you for the reply!