My thoughts:
I hate “5 year survival”. Especially when it gets correlated with “cure”. I’ve known countless people who died from their cancer in year 6 or 7.
I think it’s overly optimistic to think we can reduce our risk by 50% by behavior. There is a lot of overlap, rather than separate risk to each behavior, and some of it is correlation rather than causation.
It’s way too simplistic to think cancer has a common mechanism. It will take multiple different treatments individualized to specific cancer types to treat and cure.
At our current level of treatment, early detection is huge. Unfortunately, we don’t have diagnostic methods yet for many cancers to detect early enough.
The 5y period is useful to standardize. Then you can use compounding to get the survival over a longer period of time. For instance 75% 5y survival rate would imply only 56% over 10y. That’s why we need to get to 95% 5y survival, which would imply 90% over 10y and 81% over 20y.
According to this paper from last month authored by the world’s best cancer researchers, these factors don’t overlap and it’s causal: Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019 2024
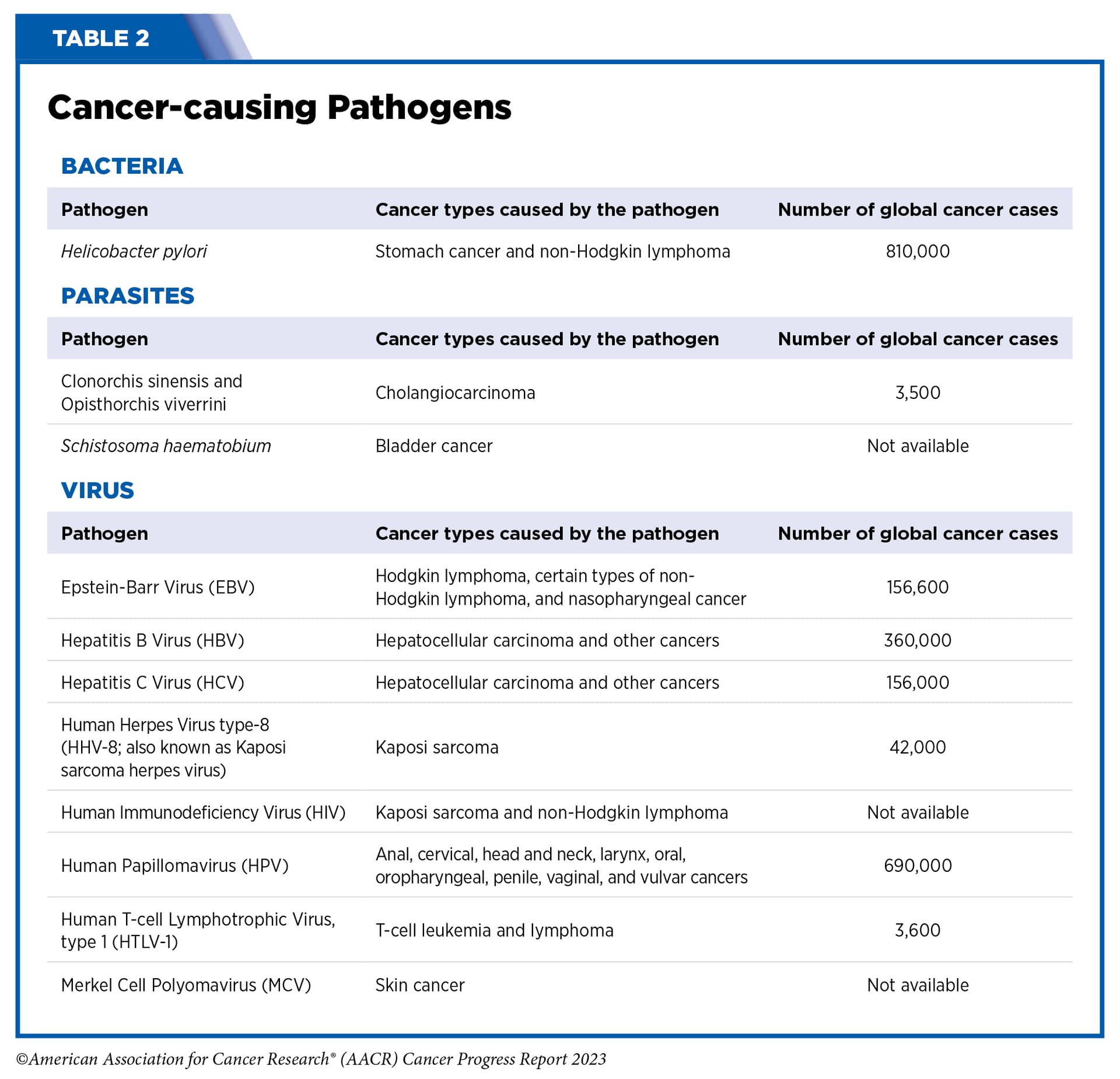
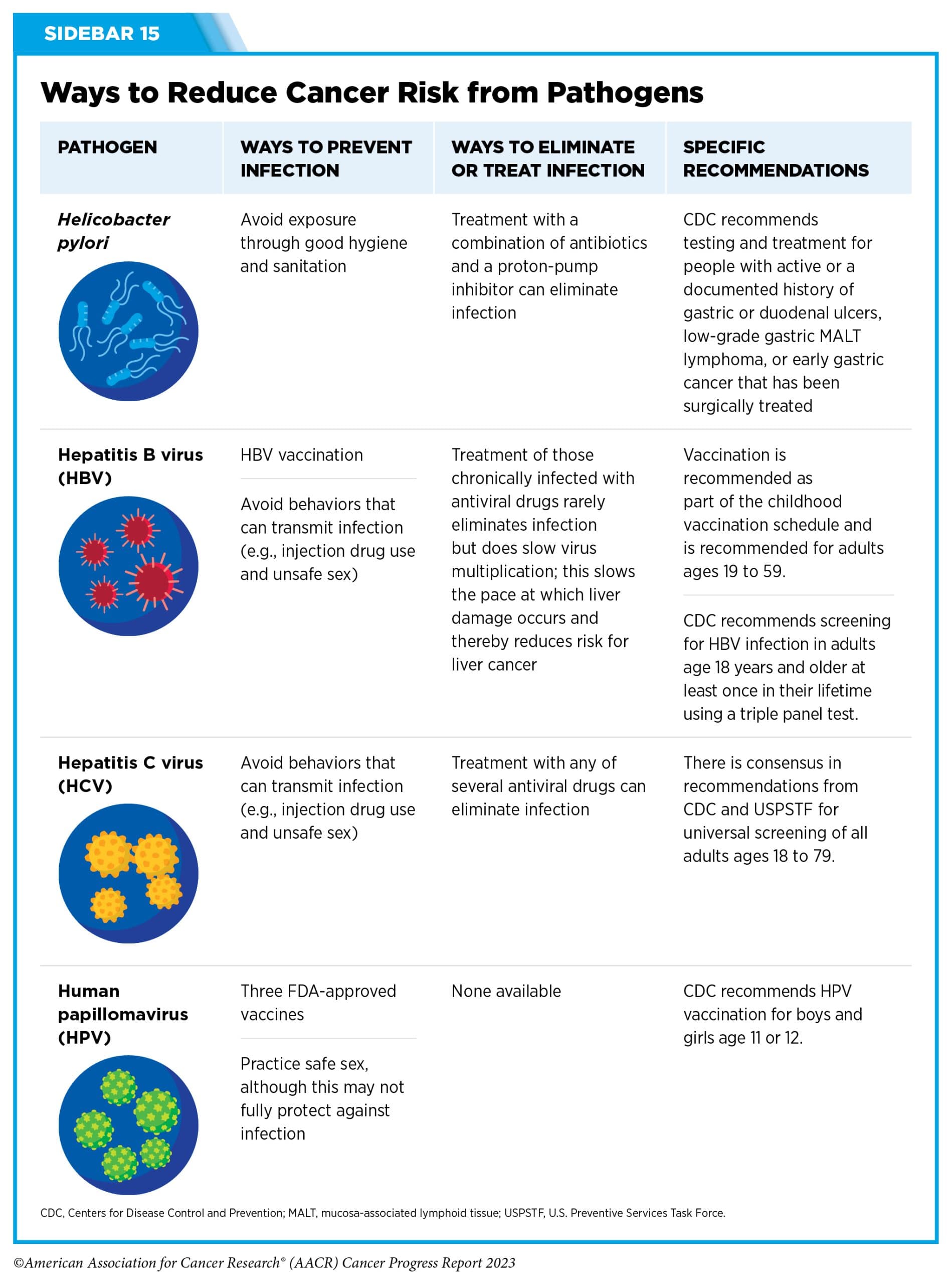
An estimated 40% of all cancer cases and nearly one half of all cancer deaths in the United States in 2019 were attributable to the evaluated potentially modifiable risk factors. These findings reinforce that the morbidity and premature mortality from cancer in the United States can be substantially reduced through broad and equitable implementation of known preventive initiatives, such as excise taxes on cigarettes to reduce smoking, screening for and treating HCV infection, and vaccination against HPV infection.
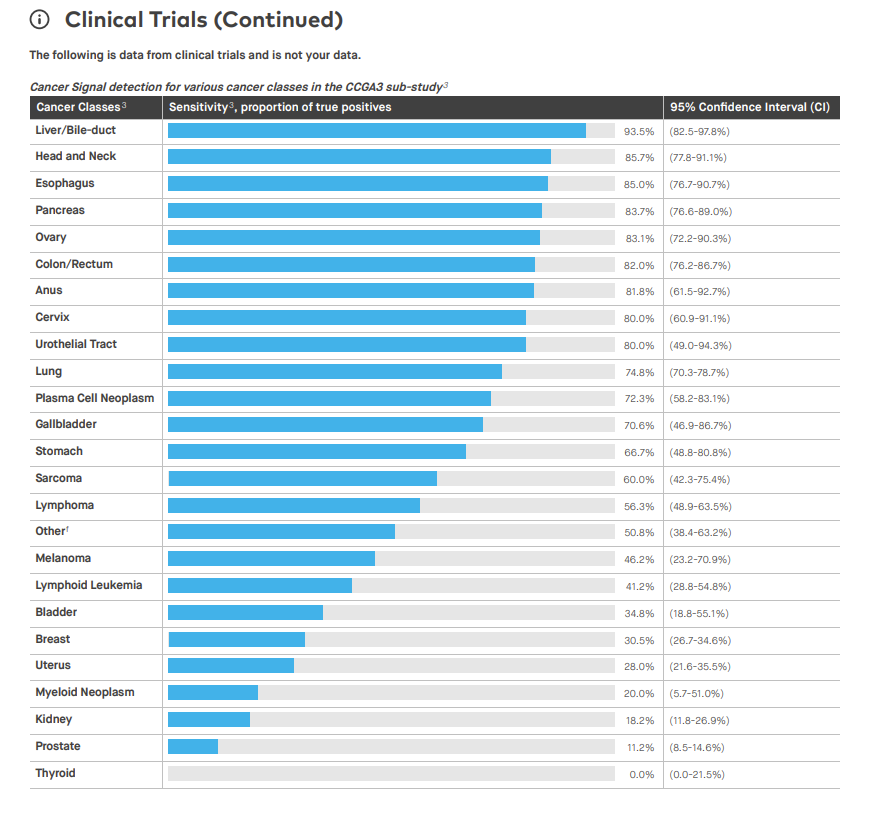
What about Galleri? They claim to be able to detect 50+ cancer types: Blood Test to Detect Cancer Signal Presence | Galleri®
In Europe there’s also TruCheck that can detect 70 types: https://health.goodbodyclinic.com/product/early-cancer-screening-blood-test
I don’t know how Galleri and TruCheck compare.
My understanding of the Galleri test is that it has a sensitivity of 50%.
That’s correct, on their website they say: Frequently Asked Questions (FAQs) for Providers | Galleri®
Less aggressive cancers, such as many thyroid cancers, release less cell-free DNA into the bloodstream and are less likely to be detected. More aggressive cancers, such as pancreatic cancer, tend to release more cell-free DNA into the bloodstream at early stages and are more likely to be detected. Higher Galleri sensitivity for the deadliest cancers helps minimize overdiagnosis and/or overtreatment of indolent cancers. Galleri has high sensitivity (76.3%) for 12 deadly cancers that comprise two-thirds of all cancer deaths, and an overall sensitivity of 51.5% for all cancers and across all stages.
What I wonder is: if you do Galleri (or TruCheck or whatever) every year, how much do you lower your lifetime risk of cancer death? I can’t find any data on this besides “The Galleri test could result in a 26% reduction in 5-year cancer-related mortality when added to usual care (based on modeled data)”.
Several leading UK cancer researchers criticized Galleri in January this year: GRAIL-Galleri: why the special treatment?
GRAIL’s primary advantages would appear to be large financial resources (the company has raised over $2 billion in private capital) and political influence, with former UK Prime Minister David Cameron consulting for parent firm Illumina, and the CEO of GRAIL Europe being Harpal Kumar, former Chief Executive of Cancer Research UK and member of the UK Research and Innovation Board. What role might these advantages have played in the selection of the Galleri test for evaluation in the NHS, when rival technologies are available?
“All screening programmes do harm; some do good as well, and, of these, some do more good than harm at reasonable cost.” A cancer screening programme that offers no improvement in cause-specific mortality (or quality of life) is only doing harm and wasting money. The GRAIL-Galleri trial must, as a minimum, show direct benefit in reducing cancer-specific mortality. This observation should feed into an independent, scientifically valid evaluation as is standard for other new candidate cancer screening programmes. Although commercial interests are powerful, world-firsts are politically attractive and patient groups champion screening for their cancer type, the NHS can ill-afford to be a world leader in the adoption of poorly evaluated interventions that might be of little or no benefit, harm people, and waste resources that could be better used elsewhere.
More on the NHS trial: An update on the ongoing NHS-Galleri trial May 2024
The NHS-Galleri trial was designed with three consecutive years of screening, and it is vital to evaluate the primary objective and endpoints at the end of the study in 2026. The primary endpoint of the trial is an absolute reduction in the number of late stage (stage 3 and 4) cancers diagnosed, and cancer-specific mortality will also be analysed after five years of follow up.
So we’ll only know in 2031 if Galleri reduces 5y mortality…
I had the Galleri test a couple of years ago shortly after it came out ($1K). I tested “positive” or “elevated” for breast cancer (very highly elevated) and prostate cancer (very low).
The low cancer “bar” was not shocking. Several close male relatives over the years have had prostate “cancer”, but none of them died of it. It is “indolent”, which my wife didn’t know the definition of, and she laughed when I told her it basically meant “lazy” or a “lay-about”. So my male relatives make it into their 80’s and even 90’s and the cancer never acts up and they end up generally dying of cardiovascular disease. I talked with my PCP and he said to get an exam every couple of years and if the yearly blood test of PSA was not elevated and if I was peeing OK, then the “do-nothing” approach works just fine, which was OK by me.
But the breast cancer high bar was weird. Still, I took a mammogram and several other tests but bupkis, nothing, as I expected. About 500 men in the U.S. die of breast cancer every year, so it’s a real thing, but not very likely.
I think the company “dials the cycle#” way high for breast cancer because they really really don’t want to miss a case, especially when they were first coming out a couple of years ago when they were trying to get approved/certified for more states. If they had “missed” a case, especially from a high-profile person, it would have wrecked their chance of full approval and/or acceptance. So from their viewpoint, it’s far better to vastly over-diagnose and have 10% or even more of male patients experience (and pay) for mammograms.
So I wasn’t impressed by it. In my case, the early version was useless, imho.
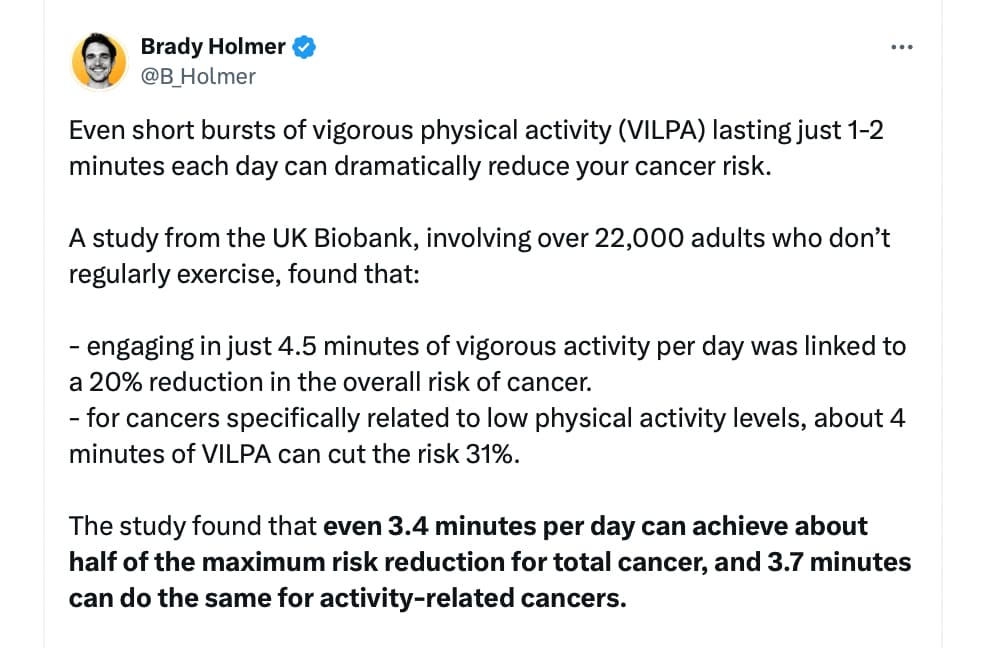
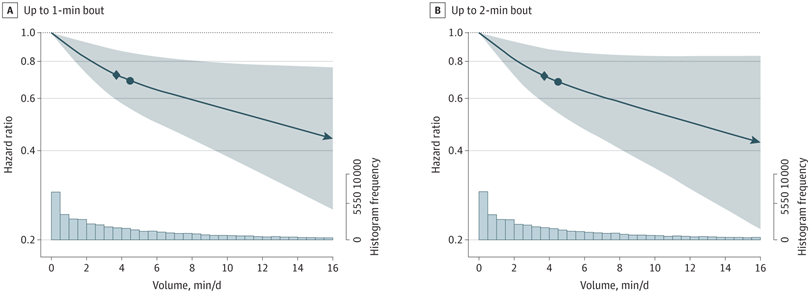
Research Paper:
July 27, 2023
Vigorous Intermittent Lifestyle Physical Activity and Cancer Incidence Among Nonexercising AdultsThe UK Biobank Accelerometry Study
Open Access: https://jamanetwork.com/journals/jamaoncology/fullarticle/2807734
What about full body MRI for cancer prevention @DrFraser @KarlT? Besides the cost, do they suffer from the same issue as Galleri (low sensitivity and many false positives)? As cancer grows quickly, do you need to do it yearly for it to be useful? Will the technology improve?
I’m recommending whole body plus MRI’s from SimonOne to most of my patients over 50 years. As a screening for vascular disease, having an MRA of the neck and head is pretty valuable, so I know how worried to be about their lipids and how tightly to manage them. Someone who is 75 years old and has not a bit of plaque in their carotids, no small vessel disease in their brain, nothing we see in their aorta … I’m pretty happy not being less aggressive on lipid management.
They also provide Neuroquant and tell you %tile of your hippocampus for example.
You’ll know if you have brain atrophy.
It’s important with the MRI’s and other imaging to not do invasive diagnostics, unless something is truly concerning. Not every abnormality requires investigation. This is where working with an experienced physician is helpful, as most of the time, abnormalities simply get tracked on yearly MRI and not investigated.
For the cancer screening on blood, I’ve gone to the product TruDiagnostic has, as it looks better than Galleri - I don’t routinely pursue that due to risk of results I’m not sure what to do with … probably happier just sticking with the MRI right now.
I would say it’s of use if you are looking for something specific. If you are just scanning to look for anything worrisome then the problem of false positives arises. My experience has been that if you look enough, you will find something, but often it’s not anything of concern but it has to be evaluated which can be expensive and with possible adverse events.
American Association for Cancer Research, Cancer Report 2024:
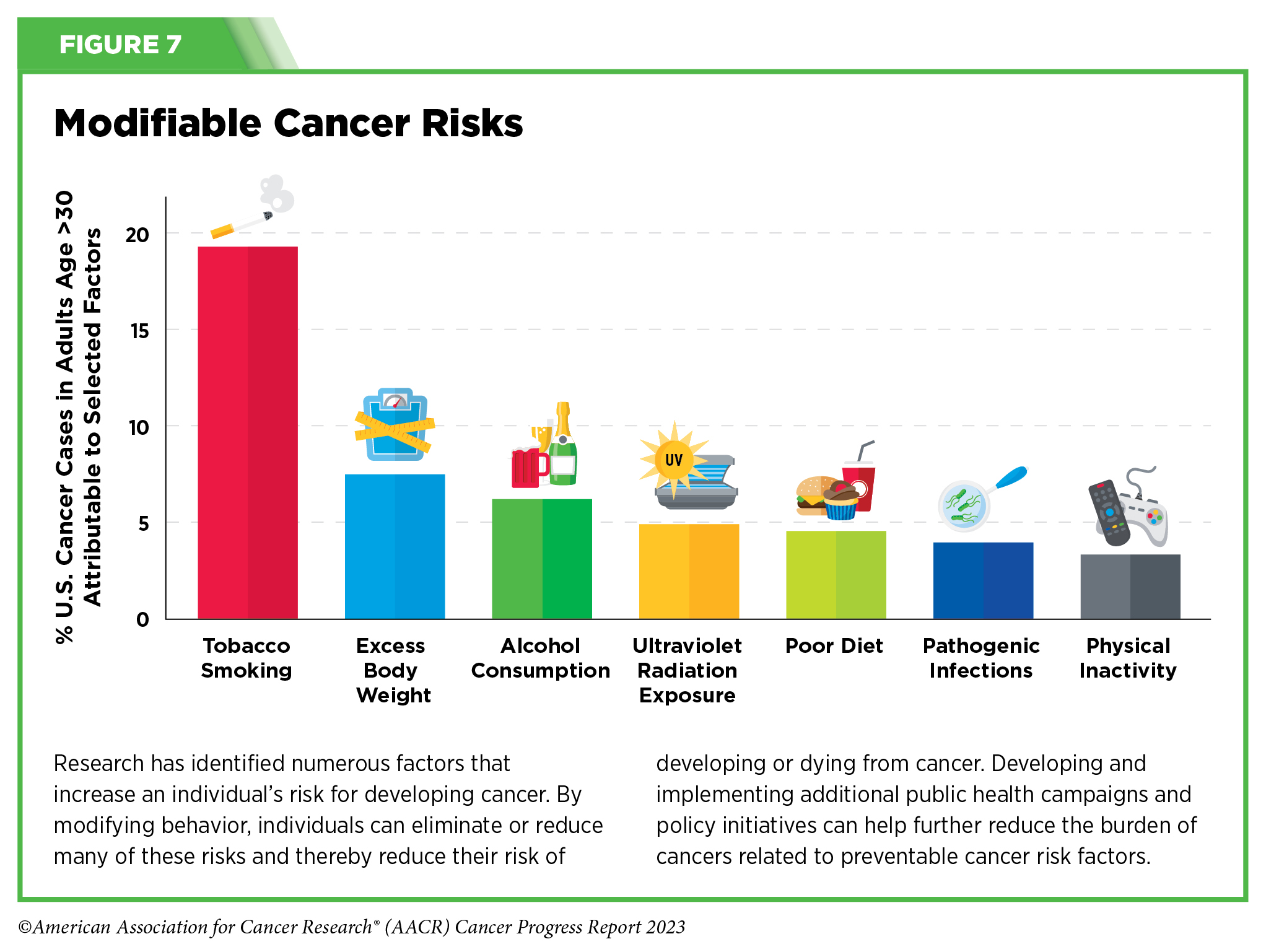
In the United States, 40 percent of all cancers are associated with modifiable risk factors.
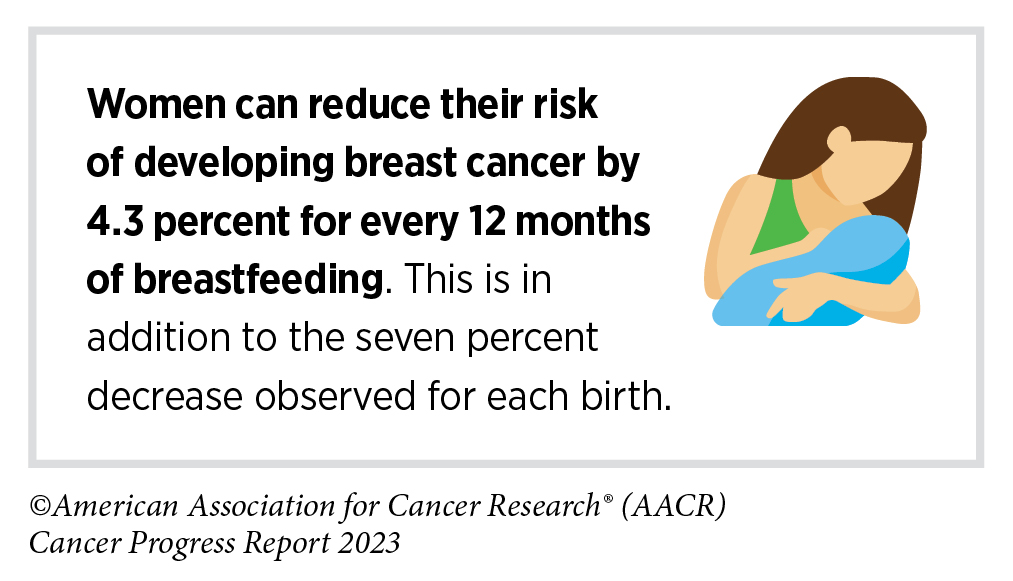
Historically, parous women – women who have given birth – were known to be less likely to develop breast cancer than nulliparous women – women who have never given birth. This protective effect of pregnancy reduces the risk of developing a type of breast cancer called estrogen receptor-positive tumor.
Chinese paper from last year (“Hebei Province Hospital of Chinese Medicine”, so not the best university out there…): Impacts of ezetimibe on risks of various types of cancers: a meta-analysis and systematic review 2023
Nine trials enrolling 35 222 patients were included in the analyses. Compared with the control group, ezetimibe increased the number of new intestine cancer patients [relative risk (RR), 1.30; 95% confidence interval (CI), 1.02–1.67; P = 0.03] and had a trend to increase the number of new breast cancer patients (RR, 1.39; 95% CI, 0.98–1.98; P = 0.07). There was no significant difference in new hepatobiliary cancer, prostate cancer, skin cancer or cancer of other sites. Ezetimibe did not significantly increase the risk of new cancer in total (RR, 1.03; 95% CI, 0.96–1.11; P = 0.38), cancer-related death (RR, 1.11; 95% CI, 0.98–1.26; P = 0.10) or cancer events (RR, 1.04; 95% CI, 0.97–1.12; P = 0.30). In terms of lipid-lowering effect, ezetimibe significantly reduced total cholesterol and low-density lipoprotein cholesterol, increased high-density lipoprotein cholesterol.
Very bad if true. Any thoughts on this @Neo?
Also: does “intestine cancer” here refer to colorectal cancer (aka bowel or colon cancer) and/or small intestine cancer?
Maybe this whole model, where healthy people take medications intended for diseases, is flawed. Perhaps all medications have some drawbacks, meaning they increase the risk of some cancer or other illness. Now, if you’re healthy and don’t know your personal genetic risk factors, you might do more harm than good. The situation is much more clear when it’s known that there’s a significantly high risk of a certain disease. This is just a thought.
What do you call “healthy” and “disease” here? I mean: from which levels of ApoB (or whatever other marker) do you consider someone to have a “disease” and not being “healthy”?
I mean the actual clinical recommendations for the use of medications.The comment was made on a general level, not specifically directed at Ezetimibe. I use it myself, but on the other hand, I have a known elevated genetic risk for cardiovascular diseases.
I use few medications for which there are no clinical indications, but I have often thought about what I wrote.
Yes, I think they are referring to colon cancer. Fortunately, it’s easy enough to screen for.
Full story:
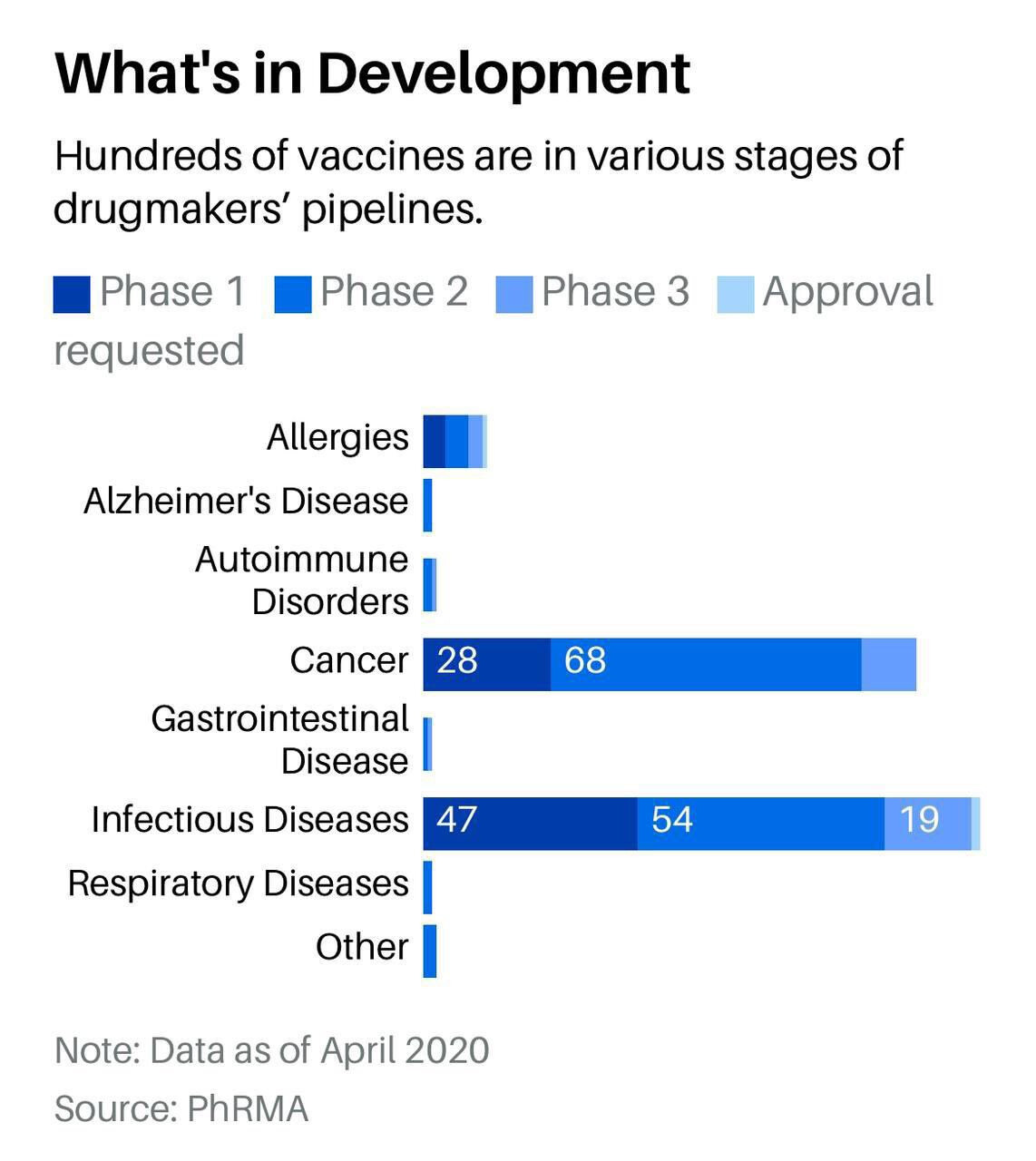
New generation of cancer-preventing vaccines could wipe out tumors before they form
Shots enter early clinical trials for healthy people at high risk for disease
When Dave Dubin learned at age 29 that he had colon cancer, it wasn’t a big surprise. His grandfather and father had both survived the disease. “It was almost the Dubin way, and we just went on,” Dubin says. He had surgery and chemotherapy, but his cancer came back 10 years later. Genetic testing finally found an explanation for his family’s trials: a mutation in a DNA repair gene that lets genetic errors pile up in dividing cells. The disease, Lynch syndrome, comes with up to a 70% lifetime risk of cancer.
Dubin, 55, gets annual colonoscopies, endoscopies, and imaging scans, which caught a third cancer, in his kidney. His eldest son, Zach Dubin, 26, inherited the DNA repair mutation and also regularly gets checked for cancer. “It’s no fun. Nobody enjoys it,” Dave Dubin says—not the 2-day colonoscopy prep and procedure, nor the worrying about possible tumors. The disease also turned him into an activist. He and his family in Haworth, New Jersey, launched a nonprofit, AliveAndKickn, to promote research and awareness of Lynch syndrome, which affects an estimated 1.1 million people in the United States.
…
Vaccines to prevent certain types of cancer already exist. They target viruses: hepatitis B virus, which can trigger liver cancer, and human papillomavirus, which causes cervical and some other cancers. But most cancers are not caused by viruses. The Lynch vaccine trial will be one of the first clinical tests of a vaccine to prevent nonviral cancers.
The idea is to deliver into the body bits of proteins, or antigens, from cancer cells to stimulate the immune system to attack any incipient tumors. The concept isn’t new, and it has faced skepticism.
https://www.science.org/content/article/new-generation-cancer-preventing-vaccines-wipe-tumors-form