I think it was £33 per 1-h session. But that was a discount for first-time users. And other places were way more expensive. I stopped after 3 sessions as I didn’t feel good during the third session at 15% FiO2. I wonder if the sensor had an issue. The clinic was also far from my home. I need to find one that is closer and try again.
If this really works and has profound benefits, isn’t there some kind of home device option? Do you need a nurse to be always present?
There are many home devices: Oxygen, hypoxia and hyperoxia - #86 by adssx
You don’t need a nurse, they’re super easy to set up and they automatically stop if anything goes wrong.
That’s very expensive. But in the end it’s only money. I mean big improvements are worth almost any money.
Hypoxico is the main supplier in the US it seems, and their machines are on the order of $2000-4000. They do not appear to have the option for hyperoxia, so a separate machine would be needed if you wanted to go that route.
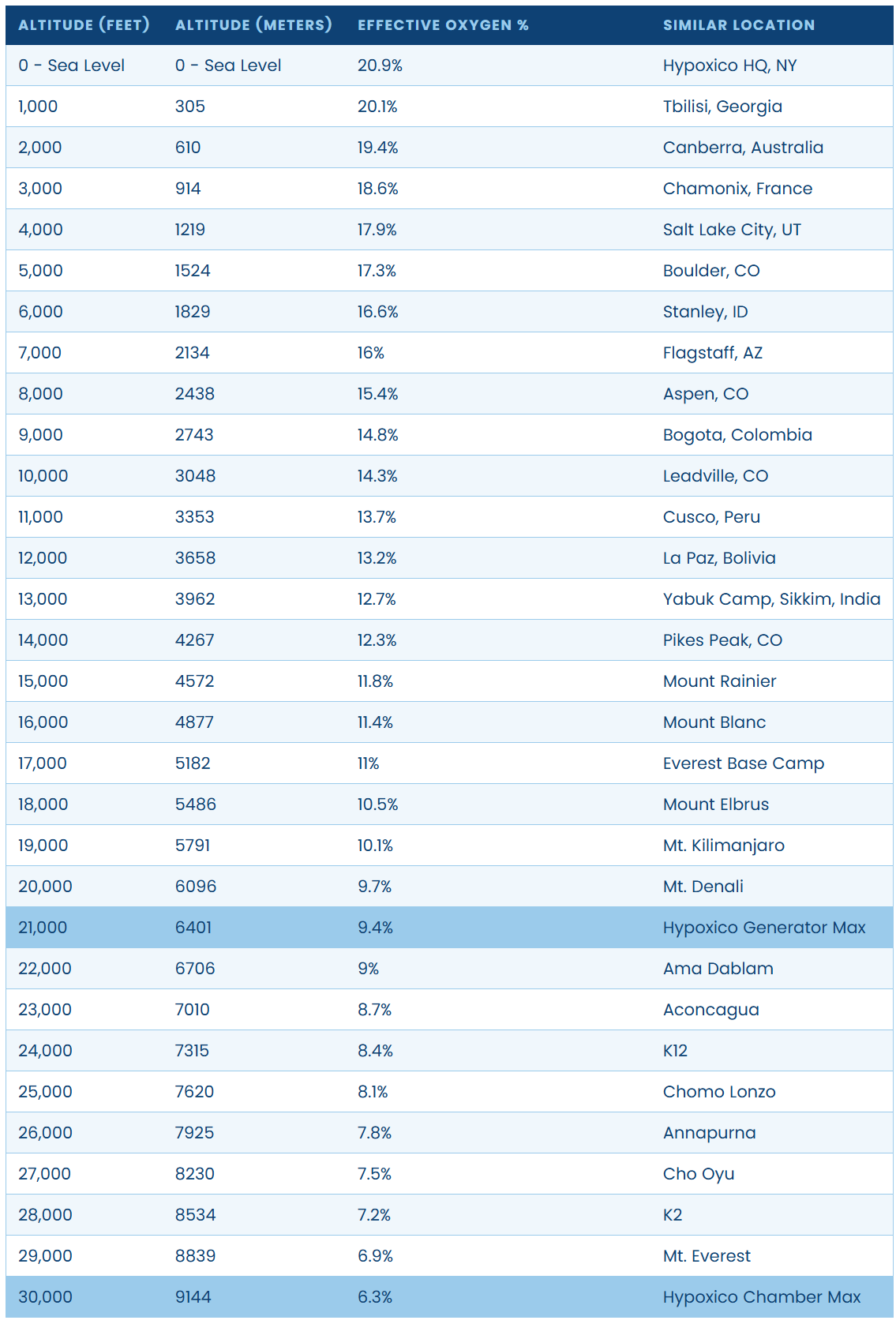
They also have a nice chart of oxygen percentage as a function of altitude. The spreadsheet version on their website also has values for the partial pressure of oxygen at each altitude.
Hyperoxia at normobaric pressures is quite cheap.
Hmm. At that price it looks tempting. I kind of think exercising at high altitude might be healthy.
Yes there are cheaper ones for instance for €2.6k (used in the PD trial): Altitude generator | Altitude training at home | b-Cat High Altitude
It seems that inhaling low levels of carbon monoxide (CO) is much more efficient at eliciting hypoxic responses than normal hypoxia due to better binding to hemoglobin than O2. [paper].
Carbon monoxide (CO) is an important endogenous molecule that can also be inhaled (Prabhakar, 1998). It has long been established that CO has an Hb binding ability greater than that of O2. Therefore, when an individual inhales CO, this can be considered to induce mild hypoxia in vivo, as carboxy-hemoglobin (HbCO) is incapable of carrying enough O2 and there is reduced amount of O2 bound to Hb and delivery to active muscle. As persistent CO inhalation reduces Hb ability to carry O2, acute exposure to small doses of CO could, in theory, induce similar performance benefits to that of altitude training. Previous research showed that increased ventilation in mild exercise rapidly removes CO from the blood in humans (Zavorsky et al., 2012). The clearance half-time in males is slower in comparison to their female counterparts due to their larger tHb (Zavorsky et al., 2014). If CO can enhance sporting performance, a sample of well-trained male individuals, who can have up to a 37% higher tHb in comparison to untrained athletes, (Kjellberg et al., 1949) is a suitable subject population as CO can remain in the blood for prolonged periods of time. Hence, it is hypothesized that an appropriate dosage of inhaled CO might have sufficient time to provoke mild hypoxia before clearance, causing similar physiological adaptive responses to that of altitude training.
For it to work, it may require combination with exercise:
Since a periodic inhalation of small amounts of CO at sea level might have potential to simulate the hypoxic effects of altitude and increase tHb mass and enhance maximal aerobic power, it is worthwhile to investigate if CO inhalation could offer a more convenient and less expensive method of improving exercise performance. In a study, by Fröscher and Uhlmann (2016) 10 days of intermittent, low-dose CO inhalation at rest did not lead to improvements in Hb mass or aerobic peak power, but to the best of our knowledge combined inhalation of CO and exercise training intervention has not been performed. Consequently, the aim of this study was to examine the effect of inhaling a small amount of CO on EPO secretion and total hemoglobin mass (tHb), running economy and maximal aerobic power in a combination with treadmill training in well trained young adults.
The protocol only requires 2 minutes (!) of breathing low-dose CO:
Twelve male college student athletes, who were well-trained soccer players, participated. They performed a 4-week treadmill-training program, five times a week. Participants were randomly assigned into an experimental group with inhaling CO (INCO) (1 mL/kg body weight for 2 min) in O2 (4 L) before all training sessions and a control group without inhaling CO (NOCO). CO and EPO concentrations in venous blood were first measured acutely at the 1st, 2nd, 4th, 6th, and 8th hour after INCO, and total hemoglobin mass (tHb), running economy and VO2max were measured before and after the 4 weeks training intervention.
They got an impressive 40% increase in EPO, and an increase in VO2 max:
HbCO% increased from 0.7 to 4.4% (P < 0.05) after 1 h of CO inhalation and EPO increased from 1.9 to 2.7 mIU/mL after 4 h post CO inhalation (P < 0.05) acutely before the intervention. After the training, the tHb and VO2max in the INCO group increased significantly by 3.7 and 2.7%, respectively, while no significant differences were observed in the NOCO condition. O2 uptake at given submaximal speeds declined by approximately 4% in the INCO group.
This paper shows similar results:
For more typical hypoxia protocols, this compares to intermittent and continuous protocols that take anywhere from 45-120 minutes to complete:
- 8x4 minutes hypoxia at 80% SaO2 (45% increase in EPO)
- 2 hours continuous hypoxia at 80% SaO2 (85% increase in EPO)
https://journals.physiology.org/doi/epdf/10.1152/japplphysiol.00941.2020
Here’s a nice article about the controversy of CO rebreathing in cycling:
CO rebreathing machine. It does not look cheap:
Yes, that’s why smokers have significantly lower risk of Parkinson’s disease. There is an ongoing trial of CO in PD. Some hypoxia trials also combine it to CO. What are other (healthier) ways than smoking to get 2 min of low-dose CO?
The thing about breathing CO is that it reacts with haemoglobin to create carboxyhemoglobin that leads to tissue hypoxia for a while. I am not myself a fan of hypoxia although I recognise that it has some positives. If I were to try hypoxia I would prefer to use a mask rather than disabling haemoglobin.
I recently received a 2.0 HBOT chamber and a generator capable of hypoxia and hyperoxia. I don’t have any particular condition that I’m looking to treat, mostly just looking for any improvements in athletic performance (ie VO2 max) and longevity (ie any health marker improvements, vascular improvements/maintenance, telomere length, etc). In part, I figured I’d give the hypoxia/hyperoxia a try because I can stack it with parts of my routine that I’m already doing like zone2, HIIT and sleeping. I’d be curious if anyone has thoughts on controlled experiments to run with before/after testing. I can easily test anything on the labcorp/quest test menus, and am willing to also pay for specialty testing.
Some ideas:
- HBOT 5/week for 8 weeks. 60m at 2.0 pressure (75m session). Measure: telomeres, VEGF, oxidative stress markers
- Zone 2 Rowing x 3/week for 8 weeks. 5m hypoxia@10-15% targeting 80% SPO2, 3m hyperoxia at 35%, repeat 8 times. Measure: VO2max, LT1, RHR
- 4x4s x 3/week for 8 weeks @ 100% oxygen. Measure: VO2max, LT1, RHR
- Sleep in altitude tent working my way down to 12%.
Subjectively would be great to see memory improvements and/or hippocampus volume increase (as measured by neuroquant), but I’m not holding my breath. Neuroquant I get once per year, so we wouldn’t be able to pinpoint a particular intervention.
If I were you I would get a CBC done to get Hematocrit and hemoglobin mass, and probably Ferritin as well. A 1 g/dL increase in Hb mass usually corresponds to a 5% increase in VO2 max. If Ferritin is low, you likely want to supplement with iron (with folate+Vitamin C) to support the increase of Hb.
You could also get EPO tested as well, but that will have a more time-dependent behavior post hypoxia exposure.
Only abstracts, mostly by the same team at Wayne State University:
- Repeated Daily Exposure to Mild Intermittent Hypoxia Improves Sleep Architecture and Sleep Quality in Individuals with Obstructive Sleep Apnea
- Repeated exposure to mild intermittent hypoxia enhances walking endurance and microvascular function in OSA patients for up to 4 - 8 weeks post therapy
- Treatment with mild intermittent hypoxia and CPAP is most effective in mitigating OSA disease severity and reducing nighttime blood pressure
- Intermittent Hypoxia Reduces Aortic Stiffness in Association with Increased Matrix Metalloproteinase Expression in Male Mice
So you are saying that since sleep apnea causes intermittent mild hypoxia, it improves sleep architecture, enhances waking endurance, microvascular function, and reduces airtic stiffness?/jk/ How can I induce this beneficial sleep apnea🤓?
Yes, there is a sleep apnea paradox: mild sleep apnea confers a survival advantage in old people (I posted papers about that earlier). Too much is bad, of course. And surprisingly, short-term hypoxic treatment during the day seems to improve OSA!
Oh look! Poking @John_Hemming and @adssx in particular.
They Inhaled a Gas and Scaled Everest in Days. Is It the Future of Mountaineering?
A group of British men went from London to the summit of Everest and back in less than a week with the help of xenon gas. Mountaineers and the Nepalese government weren’t pleased. (NY times)
As you go higher, less oxygen is absorbed into the bloodstream with each breath. That is why so many people who climb Everest use supplemental oxygen.
Xenon, an odorless gas, has been known for years to activate a molecule called the hypoxia-inducible factor, which is also turned on when people acclimate to low oxygen, said Hugh Montgomery, a professor of intensive care medicine at University College London and a mountaineer who led an expedition to Mount Everest to study how humans respond to hypoxia.
“So what these people claim to have done,” he said, “is basically found a way to switch on the adaptation to low oxygen levels.
According to this article, Xenon doesn’t provide a clear boost to EPO. Seems like CO rebreathing has better data at the moment.
Yes but the proof of the pudding is in the eating of it. They were able to climb the mountain in record slashing time.
They slept in hypoxic tents to train and then used the gas, but the kicker
The British group, which included four former special forces members
They weren’t normal people. They were top 1% already, so this is not necessarily significant.