Thanks. In summary, more UV ages the face (and anywhere else skin was exp) while less oxygen (partial pressure) reduces oxidative stress in the body. At higher altitudes, you age more slowly but look like you age more quickly.
I lived in Colorado for 25 years. The people who lived their entire lives at higher altitude (mile high city) looked eaten up with sun damage. If they had been more careful with hats and sunscreen perhaps they would have avoided looking older than their biological age. On the other hand, these Colorado “natives” I encountered tended to be vigorous and healthy outdoor athletes (frequently hiking, biking, skiing, etc)…with a probable lower biological age.
The question that I have is how much of an impact does that “premature” aged skin have on overall health? I believe it is true that skin health is a reflection of overall health, in general (poor health will lead to unhealthy skin). But does it go both ways? Does extra UV damage reduce overall health (probably to some extent) or just look like poor health (fingers crossed)?
My conclusions are:
(1) wear a hat and sunscreen (but outdoor physical activity is healthful so don’t avoid it).
(2) lower oxidative stress, without moving to high altitude, by getting plenty of cardiovascular exercise to increase the body’s ability to deal with oxidative stress.
What did I miss?
@John_Hemming you posted it a few weeks ago here ![]() Oxygen, hypoxia and hyperoxia - #73 by John_Hemming
Oxygen, hypoxia and hyperoxia - #73 by John_Hemming
Agree, I’m trying to make fishing hats and bucket hats popular. I’ve always worn farmer hats, which are free but don’t cover ears or back of the neck. If you’re out all day in the summer sun, should cover that. Trying to get the dosage right.
Yea, I live here now and sunscreen and hats are often missed as I never burn. Face is definitely showing signs of too much sun though.
OTOH I am super fit ![]()
Now, scientists at Gladstone Institutes have developed a drug that mimics the effects of breathing low oxygen. In mice with Leigh Syndrome—the most common childhood mitochondrial disease—the HypoxyStat drug extended lifespan by more than 3-fold and reversed brain damage and muscle weakness, even when given during late stages of disease.
“It’s not practical for every patient with this disease to move to the mountains,” says Gladstone Investigator Isha Jain, PhD, senior author of the new study, published in Cell. “But this drug could be a controlled and safe way to apply the same benefits to patients.”
Short bouts of hypoxia improve insulin sensitivity in adults with type 2 diabetes 2025
Hypoxia stimulates glucose uptake independently from the action of insulin. The purpose of this study was to determine the effect of intermittent hypoxia, consisting of alternating short bouts of breathing hypoxic and room air, on glucose concentration, insulin concentration, and insulin sensitivity during an oral glucose tolerance test in adults with type 2 diabetes and adults with normal glycemic control. Nine adults with type 2 diabetes (two women, HbA1c: 7.3±1.5%, age: 52±13 years) and nine adults with normal glycemic control (four women, HbA1c: 5.4±0.1%, age: 24±4 years) performed a 2-hour oral glucose tolerance test on two separate visits to the laboratory. Following ingestion of the glucose drink, participants were exposed to either an intermittent hypoxia protocol, consisting of eight 4-min hypoxic cycles at a targeted oxygen saturation of 80% interspersed with breathing room air to resaturation, or a sham protocol consisting of eight 4-min normoxic cycles interspersed with breathing room air. Intermittent hypoxia did not attenuate the increase in glucose concentration but attenuated the increase in insulin concentration in response to an oral glucose tolerance test in comparison with the sham protocol in adults with type 2 diabetes. Insulin sensitivity was greater during intermittent hypoxia in comparison with the sham protocol in adults with type 2 diabetes (0.043±0.036 vs. 0.032±0.046 μmol/kg/min/pmol, p=0.01), but did not change in the control group (0.122±0.015 vs. 0.128±0.008 μmol/kg/min/pmol, p=0.12). In conclusion, intermittent hypoxia improved insulin sensitivity in adults with type 2 diabetes.
This would be hard to do just by shallow breathing. I can just stay under 90%…although I could hold it there for a long time if I wasn’t so bored. I currently hold it for 3 minutes following 5x 30 second exhale breath holds with 10 seconds recovery between.
I like this study. I think I’ll extend my shallow breathing a bit. Thanks
Background/Objectives: Post-COVID-19 condition (PCC), also known as long COVID, has emerged as a recognized syndrome affecting millions of people worldwide, significantly impairing their quality of life. Currently, no effective therapeutic options are available to manage this condition. The objective of the present study was to evaluate the long-term effects of personalized, algorithm-based intermittent hypoxia–hyperoxia conditioning (IHHC) on quality of life and pain in patients with PCC.
Methods: This open-label cohort study included 199 PCC patients, aged 11–87 years (female-to-male ratio: 67:33) and experiencing moderate-to-severe fatigue, between 1 January 2020 and 31 December 2023. Each patient received an algorithm-based treatment plan tailored to their demographics, symptom duration, and baseline pain (NRS) and quality of life (SF-36) scores. Patients received an average of six treatment sessions (range: 2–21), each consisting of intermittent hypoxic–hyperoxic cycles, with hypoxia (9–13% O2) lasting 3–8 min and hyperoxia (34–36% O2) lasting 1–3 min. The primary outcomes were changes in the NRS and SF-36 scores at the 6-week and 6-month follow-ups.
Results: At the 6-week follow-up after treatment initiation, the SF-36 scores increased by 102 points (p < 0.001, 95% CI: 78.4–127), and this improvement persisted at the 6-month follow-up (Δ106, p < 0.001, 95% CI: 57.0–154). Pain was reduced by 28–32% at both follow-up time points, exceeding the clinically relevant threshold. Health transition scores indicated a patient-perceived improvement in health status.
Conclusions: In this study, a personalized, algorithm-based IHHC alleviated pain and improved quality of life in patients suffering from persistent long-term sequelae after COVID-19 infection. The effects were sustained for up to six months. Further research is warranted to elucidate the mechanisms underlying IHHC’s therapeutic effects in this patient population.
MDPI, no placebo.
I had a new experience related to hypoxia that I thought it would share. Yesterday I took my 12mg rapa dose while in day 1 of a FMD. This AM i did my regular hypoxia work and discovered that my spo2 would not drop as per usual.
I started at 99% vs a normal 97%
Doing my 5 rounds of 30 second exhale breath holds, my spo2 would not drop at all for the first few rounds and never below 92%. Normally I will drop to 75-85% during this exercise. Subjective air hunger was lower than normal.
Then I did my <90% shallow breathing drill for 3 minutes. Normally it take me between 0-30 seconds to settle into 90 +- 1. Today it took 1 minute to settle into my target and the air hunger was much less than normal.
Any ideas on how rapamycin or FMD is having this effect?
Eight days of MIH consisting of twelve 2-minute bouts of hypoxia interspersed with 2 minutes of normoxic recovery. Slight hypercapnia (+2 mmHg) was maintained throughout.
Upper airway collapsibility improved (n=4, 0.45±0.31, d=0.7) and was present 2 weeks postintervention (0.66±0.46, d=0.4). Apnea-hypopnea index reduced following MIH (0.44±0.20, d=0.6) and 2 weeks after (0.63±0.28, d=0.2). A significant reduction in sleep fragmentation was also observed (0.64±0.14, d=0.95).
These findings, along with the reduction in the number of arousals, suggest that the neural plasticity elicited by MIH may improve sleep quality in individuals with motor incomplete SCI, which may have positive effects on autonomic function and cognition.
Eight days of MIH consisting of twelve 2-minute bouts of hypoxia interspersed with 2 minutes of normoxic recovery. Slight hypercapnia (+3mmHg) was maintained throughout.
Mitochondrial extraction improved from 55±10% to 89±9% after 8 days of MIH (P=.07). On day 1, oxygen extraction increased from 4.70±1.62 to 4.78±2.14%, respectively. On day 8, the amplitude of oxygen extraction was 2.94%±1.25% and 3.55%±0.76% during initial and final bouts, respectively. Notably, on day 8, the amplitude in oxygen extraction was lower across all bouts compared with day 1. However, the amplitude changes from initial to final bouts were smaller on day 1 (17%±29%) than day 8 (56%±42%). After the 8-day MIH, systolic blood pressure and diastolic blood pressure changes during AD improved by 44%±8% (P<.01) and 43%±5% (P=.01) as OH improved by 88%±21% (P=.01) and 128±50% (P=.02).
Eight days of MIH improved mitochondrial capacity coupled with the reduced oxygen extraction during hypoxia on day 8, suggests an increased oxygen reserve. Likewise, these improvements in mitochondrial function were concurrent with improvements in AD and OH, suggesting that mitochondrial function may be a potential mechanism impacting autonomic function.
In vivo, 8-week-old male Wistar rats were injected with monosodium iodoacetate to induce osteoarthritis and then reared in 12% hypoxia for 24 h, followed by 24 h in steady oxygen, repeated alternately for a total of 28 days. A histological analysis was performed on days 8 and 28.
Intermittent hypoxia increased cartilage metabolism by increasing hypoxia-inducible factor-1α proteins in articular chondrocytes, which may be effective in preventing articular cartilage degeneration in a rat osteoarthritis model.
There are some basic cellular controls one is hif 1 alpha.
What are you using for a pulse oximeter? Googling a bit, it seems most oximeters are accurate to only about 2-4%, and many factors can make it worse such as cold hands, movement etc. Seems like a reading of 97 vs 99% is basically the same. Have you noticed the same behavior since posting this a month ago?
I recently started doing this protocol in an effort to increase EPO/hemoglobin for a race I have coming up; the paper showed a 24% increase in EPO using apneas.
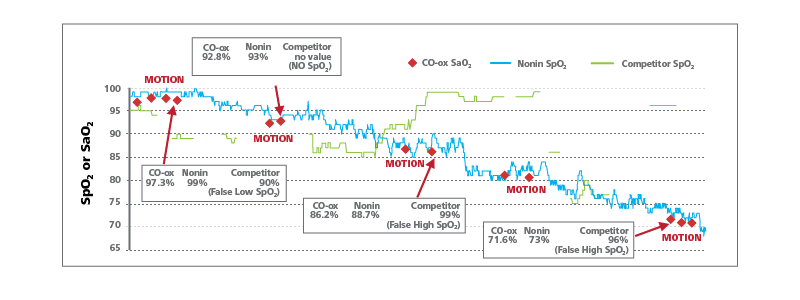
They did 3 sets of 5 max breath holds, but stopped the hold when about 60% SaO2 was reached (since this was a study, they had catheter O2 measurements rather than SpO2 pulse readings). I’d imagine there is probably a lag in SpO2 vs SaO2.
Protocol is:
- 1 minute of hyperventilation followed by a max breath hold
- 2 minutes rest between holds, repeat 5 times
- 10 minutes rest between sets of 5
Using a pulse oximeter off Amazon, I typically start off at 95%+ and get to around 50-60% at the end of a hold. It’s probably very inaccurate at the lower range, but at least O2 seems to be getting quite low.
It seems like oximeters are just not calibrated below 80%, and peripheral blood flow may be altered when more hypoxic, so all bets may be off when trying to use them below that level.
It was a one time thing. The next time and every time since my spo2 patterns were back to my normal. “Normal” doesn’t mean always the same. Some days my spo2 drops fast on every set, while other days it is resistant to falling (drops slowly and not as far). I never get the “won’t drop at all” effect except that one time with rapa, which is why I posted about it.
I use a Wellue Viatom (see photo).
I will do it again on a rapamycin day (take at night; spo2 in next AM).
I’ve noticed the lag. I do a 10 second recovery (pressure breathing) between aches of the 5 30 second long sets. My spo2 recovers to 96 or 97% each time but the recovery occurs / is seen / is felt at different times.
(1) my lungs get the o2 and dump the co2 immediately
(2) my brain senses the drop in co2 after about 5-10 seconds
(3) my spo2 recovery takes 20-30 seconds to show up at my finger
How reducing oxygen-transport may lower the risk of developing Parkinson’s disease 2025
Carbon monoxide (CO) produced during smoking has been proposed to be a protective factor for Parkinson’s disease (PD). In rats, increasing CO levels have recently been shown to induce hypoxic response-like pathway activation. Smoking thus may strengthen the hypoxia response systems by challenging the oxygen transport system, resulting in increased cellular resilience. Here we outline the overlaps between two novel promising approaches against PD, low-dose CO inhalations and hypoxia conditioning.
Deficits in cellular and systemic responses to altered oxygen availability are increasingly acknowledged features of PD. Various approaches can restore these responses and possibly benefit people with PD. Smoking—at least in part via increasing CO-levels and thereby repeatedly challenging the oxygen transport system—may reduce the risk for PD by “training” the hypoxia response systems and leading to increased cellular resilience and maintained adaptive capacities on the systemic levels (e.g. hypoxic ventilatory response). However, the adverse effects of tobacco smoking greatly outweigh potentially protective components of smoking or smoking behavior in PD. Smoking is associated with increased risks for many non-communicable diseases, including vascular and respiratory diseases or neoplasms, and therefore clearly is not suitable as a preventive strategy. Accordingly, although PD smokers may die from fewer neurological causes, their risk to die from smoking-related cancers has been shown to be significantly increased. Should the beneficial effects of increased CO-levels in PD be confirmed, low-dose CO inhalations may be one interesting novel strategy to target one crucial aspect of PD. If short, repeated exposures to hypoxia have similar consequences like CO, hypoxia conditioning, strategic altitude exposures or adapted breathing exercises will be important alternative approaches.
The experimental group showed periodic desaturation, with minimum and maximum oxygen saturation values of 80.19 ± 0.34% and 97.68 ± 0.31%, respectively.
After 3 hours of exposure, ABR and the spontaneous firing rate (SFR) of auditory cortical neurons were recorded.
Short-term IH induces high-frequency hearing loss, reduces ABR latency, and enhances cortical neuronal excitability, implicating both peripheral and central auditory pathways.
There’s clearly a trade-off with hypoxia @John_Hemming. I don’t have access to the whole paper to check the exact protocol.
Out of curiosity, what was the cost of a session?
Have you continued to do sessions regularly? If so, anything to report?