Reading the paper again, a few interesting bits:
Specifically, PFF-induced α-syn aggregation resulted in brain tissue hyperoxia, lipid peroxidation and DA neurodegeneration in the SNpc of mice breathing 21% oxygen, but not in those breathing 11% oxygen.
Because prior studies showed mitochondrial respiratory chain dysfunction induced by α-syn, and because primary mitochondrial dysfunction can result in tissue hyperoxia, we wondered if the partial pressure of oxygen (pO2) is elevated in the SNpc of our PD mouse model. To our knowledge, no prior study measured brain pO2 in patients with PD or in mouse models of α-syn toxicity. We measured the pO2 in the SNpc using a fiber-optic fluorescence oxygen sensor 6 weeks after intrastriatal injection of PFF or monomer. When breathing 21% O2, mice injected with PFF exhibited higher brain tissue pO2 in the SNpc compared to mice injected with α-syn monomer (Fig. 2c). In contrast, breathing 11% O2 inhibited the PFF-induced increase in brain tissue pO2 in the SNpc. There could be multiple mechanistic explanations for the observed relative hyperoxia, including decreased oxygen consumption by the mitochondrial respiratory chain due to PFF inhibiting MCI.
We hypothesized that local hyperoxia in the PFF-injected SNpc of mice breathing 21% O2 could promote lipid peroxidation. Recent genome-wide CRISPR genetic screens revealed a strong synthetic lethal interaction between mitochondrial respiratory chain inhibition and genetic loss of GPX4, a lipid hydroperoxidase33. Moreover, oncocytic thyroid carcinoma is associated with somatic genetic loss of MCI and is highly sensitive to death from lipid peroxidation34. To test this hypothesis, we measured malondialdehyde (MDA) levels in the SN 6 weeks after intrastriatal injection of α-syn PFF or monomer. In mice breathing 21% O2, those with PFF-induced α-syn aggregates exhibited higher MDA levels in the SN compared to monomer-injected mice (Fig. 2d). In contrast, breathing 11% O2 attenuated the PFF-induced increase in MDA levels in the SN. These observations suggest that hypoxia attenuates lipid peroxidation in the SN after α-syn aggregation by mitigating brain tissue hyperoxia without affecting iron accumulation.
While the precise mechanisms responsible for the toxicity of α-syn aggregates to neurons remain an unsolved problem, many prior studies have shown that PFF-induced α-syn aggregation compromises the activity of the mitochondrial respiratory chain in DA neurons of the SNpc. Because more than 90% of oxygen is consumed by mitochondria, unused oxygen is theorized to accumulate when oxidative phosphorylation is impaired. Classic studies have shown that patients with inherited mitochondrial disease can exhibit tissue hyperoxia because of poor oxygen extraction, especially during exercise. In fact, we previously reported hyperoxia in the vestibular nucleus and striatum of the Ndufs4−/− mice breathing 21% O2. In this study, we uncovered that α-syn aggregation induced brain tissue hyperoxia in the SNpc of mice. It will be interesting to determine whether brain hyperoxia is also a feature of human PD. Although tissue hyperoxia could be a direct consequence of respiratory chain impairment and oxygen use, we acknowledge that there could be other mechanistic bases (for example, changes in vascularity, low neuronal and hence metabolic activity, changes in pH leading to more O2 offloading). Regardless, the brain tissue hyperoxia observed in the SNpc of mice breathing 21% O2 that also had PFF-induced α-syn aggregation supports the notion that high oxygen itself may be mediating the neurotoxic effects of α-syn aggregates.
α-Syn aggregation induces neuronal iron accumulation in the SNpc35. Our RNA-seq results, which revealed upregulation of Tfrc and Fpn by PFF and breathing 11% O2, support the potential role of iron accumulation in PD pathogenesis. Along this line, a recent study using a nonhuman primate model of PD reported that intranasal administration of α-syn PFF increased iron deposition and protein levels of TFR1 (encoded by Tfrc) and FPN in DA neurons in the SN of Macaca fascicularis44. We speculate that the combination of iron accumulation and tissue hyperoxia can jointly lead to neuronal toxicity via Fenton chemistry, which contributes to lipid peroxidation. IRP2 is a key posttranscriptional regulator in the iron starvation pathway including TFR1 and FPN. We previously reported that genetic ablation of FBXL5, the ubiquitin ligase that targets IRP2 for degradation, is tolerated in hypoxia but not normoxia41. Hence, activation of this pathway in normoxia is detrimental. Moreover, recent CRISPR genetic screens and cancer literature revealed that cells with compromised MCI are particularly susceptible to loss of GPX4, the key phospholipid hydroperoxidase that guards against death caused by lipid peroxidation. The inhibition of tissue hyperoxia and lipid peroxidation by breathing 11% O2 for 6 weeks in PFF-treated mice further supports the critical pathogenic role of tissue hyperoxia that is probably induced by mitochondrial dysfunction.
These observations suggest that it is possible to reverse motor and non-motor symptoms even if the treatment is started after LB-like inclusions have accumulated in the SNpc and symptoms become clinically evident, a situation that more closely recapitulates a treatment scenario in human PD. To the best of our knowledge, hypoxia is the only intervention that not only prevents, but also reverses, neurological defects in this model.
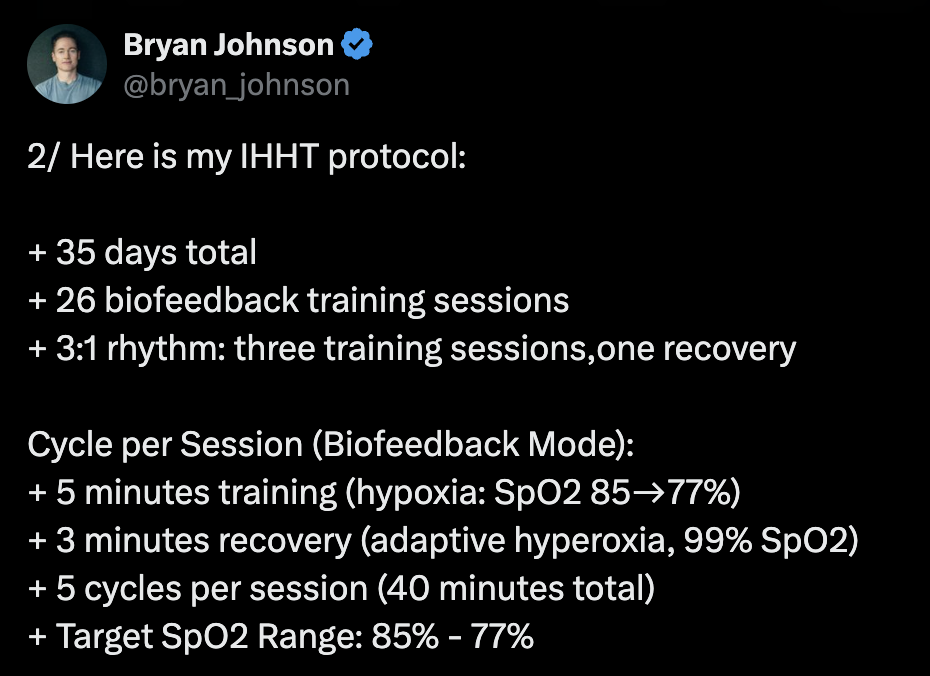
Of course, these are animal models (worm and mouse) but it suggests that hyperoxia might be detrimental in PD @John_Hemming so I think that for people with PD HIF activation via intermittent moderate hypoxia might be more beneficial than via intermittent hyperoxia. Or at least, there’s a potential risk that is worth being studied more.