I have been tracking my glucose using a CGM on and off for about 2 years. I have also been testing Acarbose in conjunction with Rapamycin to see the effects. I eat a very high plant rich diet so my glucose levels are generally quite good. And I have seen comments on this site about results from Canafliflozin and SGLT2 inhibitors – and listening to Peter Attia on this topic. In general I’m hearing that we want to keep all glucose spikes to under 130 or 140 and work towards an average blood glucose of under 100 and a Standard Deviation of 15 max. I guess my question is if we feel like these are good optimal numbers? Secondly, if we can keep the average under 100 without medication then there’s probably not a need for medication? Or do we feel that it’s just lower is better - period. Should we be shooting for >90 on average using the medications? Do we have any data on what is optimal from research ?
Good questions. 15 years ago my FG was 75. Now it’s 92-99. I assume that 75 is better than 99. That’s why I started Metformin.
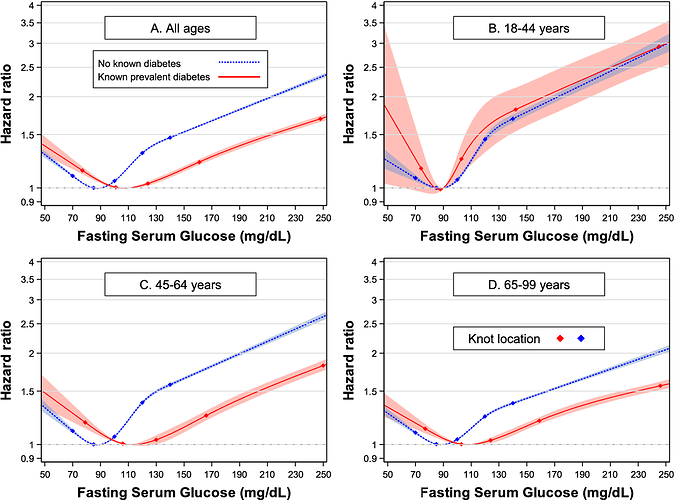
I think we probably want to target a fasting glucose level of around 80, based on this information:
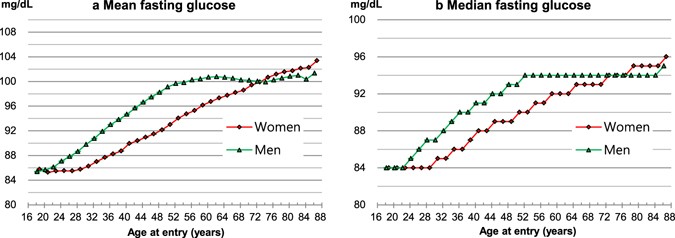
and here the typical blood glucose levels that map to higher risk of dying:
Source Documents:
Unless I am reading the charts wrong, people over 44 yrs old in this forum are overly concerned with their fasting glucose levels.
The hazard ratios for glucose levels between 90 and 110 are pretty small for that age group.
I quit worrying about fasting glucose levels years ago when I was on a keto diet. Now I rely on my HbA1c results.
I agree that HbA1c is more significant in many ways, but many of the algorithms for biological age rely on fasting glucose. I am also someone who although not diabetic at times uses a CGM (I intend to use one again once I have stabilised my lab arrangements). I think it is worth understanding how the body handles glucose with a view to working out if dietary changes are warranted or the times of eating are worth changing.
“The pro-longevity effects of rapamycin are conveyed through mTORC1 whereas mTORC2 inactivation is believed to be responsible of the insulin resistance phenotype associated with rapamycin treatment (Saxton and Sabatini, 2017).”
This may be a guide to rapamycin dosing. If your fasting glucose rises too much, you are probably suppressing mTOR2 too much.
My path has changed from dosing at 15 to 20mg with GFJ and EVOO to my present dose of 5mg of rapamycin with EVOO once a week, coincidentally the same dosage Dr. Green recommends for most of his patients.
5mg/week with EVOO is producing no unwanted side effects and my blood test markers including HbA1c are now in the normal range.
I believe this article has been cited before but it is one of the most comprehensive articles I have read regarding lifespan and healthspan interventions.
But then, in rodent studies hyperglycaemia was also noted with chronic Rapa administration - yet it did not seem to affect the increases in lifespan. So how do we know whether taking a dose so low that you would avoid hyperglycaemia may hopefully also result in any increases in lifespan. Or we may be dosing too low to reap any benefits at all.
The fact is no one knows the most effective dose in humans, but the dosage appears to have benefits over a wide range.
“First, rapamycin is effective over a wide dose range.”
Also here is a video (sorry if this was posted before) of Dr. Green discussing dosage.
Yes - a key issue, that sadly we don’t have any good answers to yet.
Optimal glucose levels are only optimal if you don’t have to use high insulin levels to achieve ![]() Many people have great glucose and A!c levels only to become diabetics because know one is paying attention to their insulin levels.
Many people have great glucose and A!c levels only to become diabetics because know one is paying attention to their insulin levels.
Do you have any studies or citations to back that up?
Yes, it looks like the significance of FBS up to 110 in older people is low.
@desertshores - I don’t have any specific studies, but 25 years of medical practice and watching patients being told that their glucose and A1c are normal and then slowly start to be come abnormal over the years. Any diabetic ( on insulin ) can tell you if you want to make your glucose levels look good, just take more insulin. Checking a fasting insulin level became popular in evaluating women with polycystic ovarian syndrome and later metabolic syndrome. A classic patient I see is 50+ pounds overweight and they very proudly tell me how great their sugars are, but when you check an insulin level, its sky high. My point is, you should really check both in order to best evaluate since a high insulin level can make your sugars look good, but create weight gain, inflammation and ultimately diabetes by pancreatic depletion of the beta cells that produce insulin.
If you have a BMI of <22.5 I think it would be an unnecessary test if your fasting glucose and A1c are normal. I wish you were my doctor. My doctor is smart but is loath to prescribe tests that are not indicated by other factors.
A BMI that low probably means you’re a skeleton.
Sorry, that is the second time I’ve done that. I stand corrected. ![]()
For various reasons I have studied HbA1c over the past day. I find that in fact HbA1c has two elements an aldimine adduct and a ketoamine adduct. Glucose starts reacting to create the admine adduct and then more slowly reacts to create the ketoamine adduct. Although the latter reaction is slowly reversible it is that which arguably follows the average glucose level over multiple days. The former part follows glucose levels by about 2 hours.
Some tests distinguish ketoamine from aldimine and others don’t.
You are correct! A normal BMI helps the accuracy of sugar tests, but not always the case with PCOS women and infertility. Some have low BMI and respond well to metformin in regulating ovulation.
BMI is another standard that may need more attention. Body fat percentage is a much better predictor of health and sugar than BMI, especially when dealing with an athletic population.
I would guess that most overweight people with normal sugar levels have a sugar problem that is being hidden by high insulin. Insulin then coverts the sugar to body fat. Unfortunately, this can go on only so long before the pancreas can not keep up with the demand and then sugars start to climb. Amazing how many primary care providers are puzzled when patients with perfect sugar labs for years become diabetics. I think all overweight patients have a sugar problem no matter what their levels are. This is one of the main reasons big pharma is changing its approach to weight loss using medications that control sugar and insulin.
Why is fasting glucose of 70 riskier?
The mechanism for low fasting glucose level conferring harmful effects may be related to the activation of counter-regulatory hormones, especially epinephrine.33 Such a hormone stimulates glucose production and inhibits glucose clearance when hypoglycaemia occurs and could provide enough energy to various organs, especially the brain, under stress. However, Q wave to T wave (QT) interval prolongation also occurs, caused mainly by sympathoadrenal stimulation due to higher epinephrine levels during hypoglycaemia.34 35 For instance, a previous study on insulin-induced hypoglycaemia in healthy individuals showed that changes in R and T waves were associated with counter-regulatory adrenergic activation, with elevations in norepinephrine and epinephrine.34 This acquired long QT interval syndrome and T wave abnormality would affect ventricular repolarisation and increase risk of ventricular arrhythmia,36 as shown in a study of non-diabetic men with a median follow-up of 23.3 years, in which fasting glucose concentration was inversely related to incident risk of ventricular arrhythmias.37 As such, an increased risk of sudden cardiac death related to ventricular arrhythmias36 due to low fasting blood glucose levels could explain increased all-cause mortality in our meta-analysis. Although mortality related to cancer could be a concern, studies that analysed the relationship between glucose level and cancer incidence did not show low fasting blood glucose level to be related to increased risk of cancer.1 8 38
Brain glucose concentration has a linear relationship with blood glucose concentration.39 Since the major energy source of the brain is glucose, hypoglycaemia may damage the brain and cause stroke-like symptoms.40 Brain imaging changes could be observed if severe long-term hypoglycaemia occurs.40 41 Also, arrhythmia caused by hypoglycaemia may increase stroke risk.36
There have been some systematic reviews and meta-analyses exploring the association of hypoglycaemia and mortality/cardiovascular disease.18 42 Goto et al 42 found that hypoglycaemia was associated with a higher risk of cardiovascular disease in patients with diabetes, and Yeh et al found that hypoglycaemia was a risk factor for adverse vascular events and mortality across different populations.18 The novelty of the current meta-analysis we conducted is we only included studies enrolling people without diabetes and cardiovascular disease at baseline, and therefore, the majority of studies included in our meta-analysis were not included in the previously published two meta-analyses mentioned above.18 42 Although the detrimental effects of hypoglycaemia are well established in people with diabetes or critical illness,18 42 this is the first met-analysis, to our knowledge, to show that low fasting glucose (ie, <4.0 mmol/L) is associated with increased risks of all-cause mortality and stroke in people without baseline diabetes or cardiovascular disease. Low fasting glucose concentration found in people without diabetes and cardiovascular disease is not typically regarded as a marker of potential danger for future mortality and cardiovascular disease. However, the current meta-analysis suggests that non-diabetic people with a fasting glucose <4.0 mmol/L may be at future higher risk of mortality and stroke, and therefore might merit a more comprehensive evaluation and regular follow-up.
^I don’t think I believe that this mechanism is primary for those with low BG