That makes sense. Thanks. fwiw I’m 41 so I’m not too worried about falls
That was a great video.
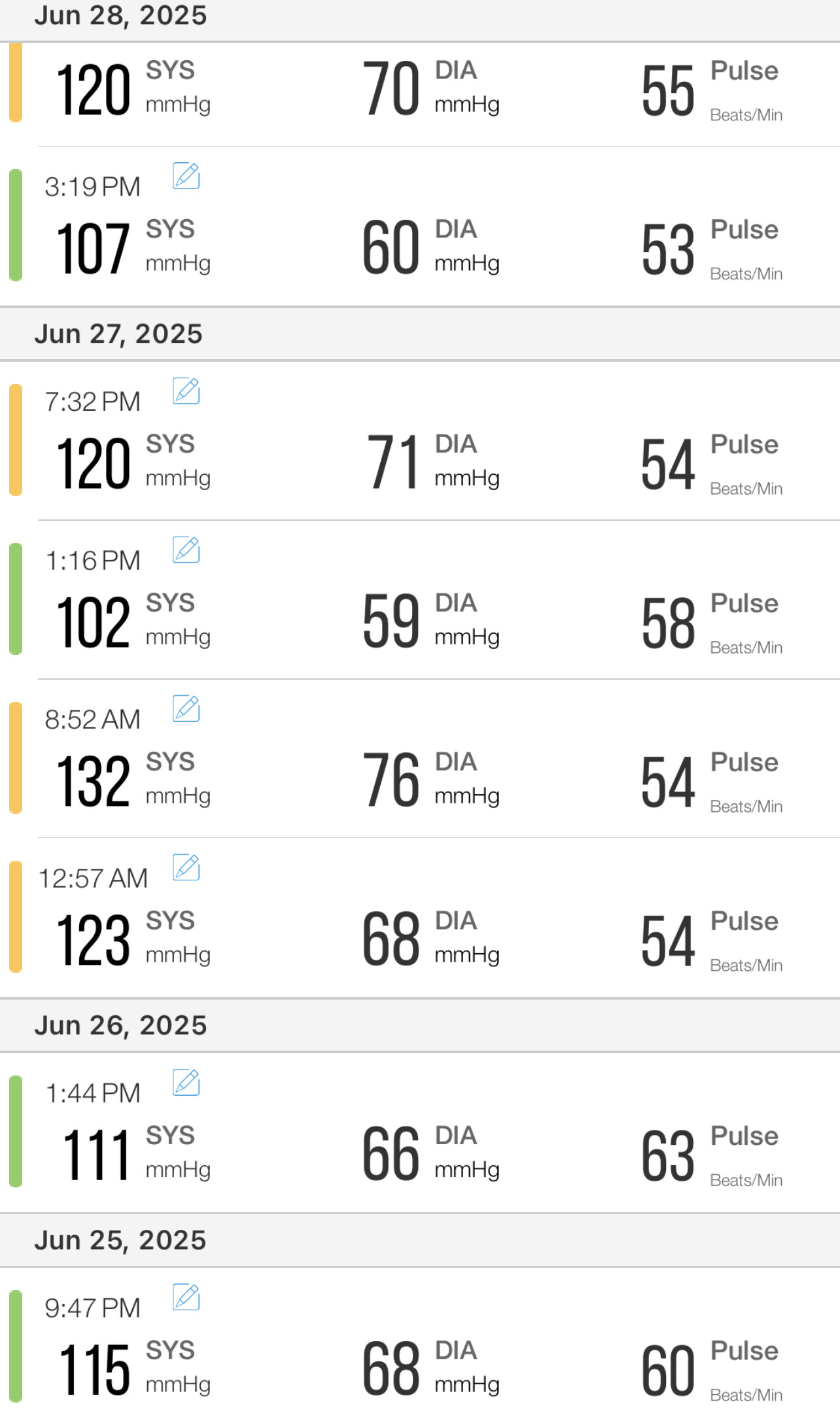
My bp was averaging 122/80 on 80mg of Telmisartan.
When I started on just half a tablet of Dutasteride I quickly noticed every time I got up from a squatting position I had orthostatic hypotension. Measured my bp and 10 points had dropped off.
Have gone back to 40mg on the Telmisartan to get it back up to around 120/80 again.
If height has anything to do with it I’m 6ft 2” Maybe shorter people can get away with a lower bp. I need the 120 level.
I’m much shorter, 5’3”, and also have orthostatic BP and also prefer 120 to function. I usually measure my BP in standing and then in sitting position. The difference in systolic is sometimes 15-20 points. Most of the day I’m either standing or moving, therefore I rely more on t standing readings, which I prefer to be 120.
I was not sure what his wrap-up was, so I asked for a synthesis of his message. Yet, at the beginning, he cited a whack-a-mole, but then at the end, he leaves it in suspension? Has anyone grasped his take-home message?
Does the AI construe the takehome the same you guys construed?
__________________________________________________________________________________AI Gemini flash 2.5
In the video, Dr. Brad Stanfield shares his personal journey in managing high blood pressure and high cholesterol, highlighting how his experience reflects important principles in disease prevention and longevity.
Summary of Content:
Dr. Stanfield recounts discovering he had high blood pressure (140) back in 2011, during his second year of medical school, a value not optimal for his age. Despite an initial false sense of security due to a lower reading in a medical setting, consistent home monitoring revealed persistent values between 140 and 150. He ruled out secondary causes and, despite maintaining a healthy lifestyle, concluded that genetics played a significant role.
For blood pressure management, he opted for a combined pharmacological approach:
- He started with candesartan (an angiotensin receptor blocker), gradually increasing the dose.
- He added empagliflozin (an SGLT2 inhibitor), despite not being diabetic, for its benefits on blood pressure and potential effects on male longevity (according to mouse studies), a choice that required specialist approval.
For cholesterol:
- He noted a slight increase in LDL cholesterol due to empagliflozin.
- He started with rosuvastatin (a statin) to reach a very low LDL cholesterol level (below 1.4 mmol/L or 50-60 mg/dL), a level associated with the absence of plaque.
- He added ezetimibe to enhance the cholesterol-lowering effect.
- Subsequently, he replaced rosuvastatin with pravastatin (a less potent statin but with a lower risk of inducing type 2 diabetes), once he reached his LDL target.
The Key Takeaway (Take-Home Lesson):
Dr. Stanfield’s main lesson is that, while a healthy lifestyle (diet and exercise) is absolutely fundamental for health and longevity, in many cases genetics plays a predominant role. Therefore, it may be necessary and wise to resort to pharmacological interventions to achieve and maintain target blood pressure and cholesterol values, even in otherwise healthy individuals with an exemplary lifestyle.
He also emphasizes the importance of regularly monitoring one’s values at home and the strategy of using combinations of low-dose medications to maximize effectiveness and minimize side effects.
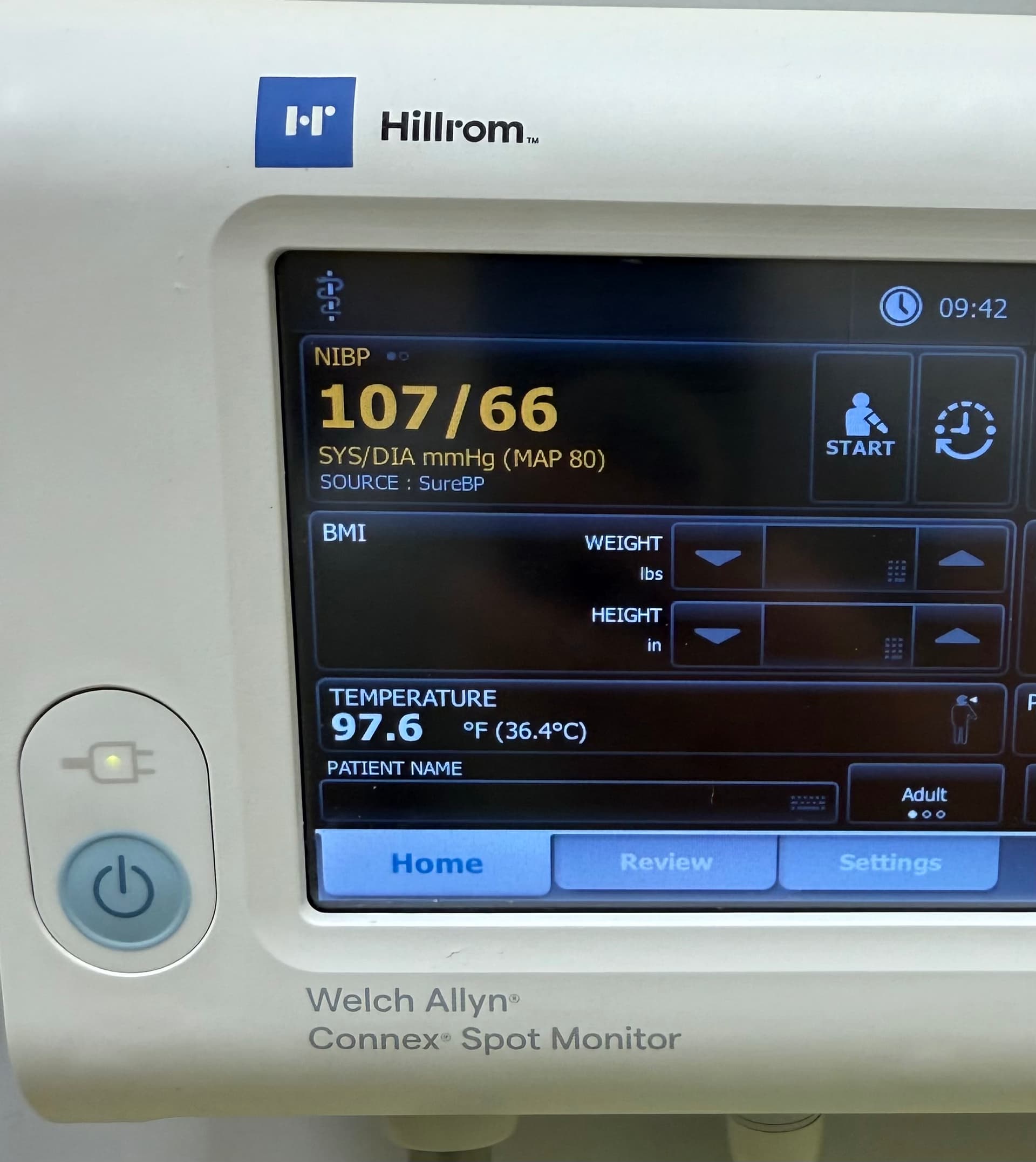
I went for a work physical this week and the staff that took my BP thought something was wrong because it was 107/70. She said she needed to recheck it because it was so low. I told her that was actually on the higher side for me and she said she had never seen a reading that low. Thankfully I found out when she went to place my PPD that she was a student. It’s still pretty sad that she never sees people with a BP like mine. I figured if there was anyone in the world who would appreciate my little story it would be the contributors to this thread!
I automatically assume doctors won’t cooperate with my needs so I order meds from these online pharmacies instead. So then when I actually go to a doctor, I pretend I was getting it prescribed from the last doctor already and ask if they can take over the prescription. It works sometimes.
I just tested my 15 year olds BP and his SBP was 145! I think he may be too young for meds, but I’m unsure what to do. Maybe citrulline…
Remember that these things vary a lot. Take a few measurements when things are calm at different times.
I concur, a single measurement is not meaningful. Also, there might have been an averse reaction to the cuff tightening, triggering an alarm.
Yeah, you’ll need a lot of validation on that reading. The kid could experience white coat effect, simply stress from a novel procedure, or it could be measured wrong (did he cross his legs?). Take a few readings and average them, do so over a few days. Don’t make any far going conclusions and decisions without being sure you’re operating from valid data.
Since I started taking Citrulline my BP has improved. My glucose also dramatically improved (wearing monitor) and I don’t know why. It’s now on a lower side, with fasting 70-90 and no higher than normal spikes. Would like to figure out the reason.
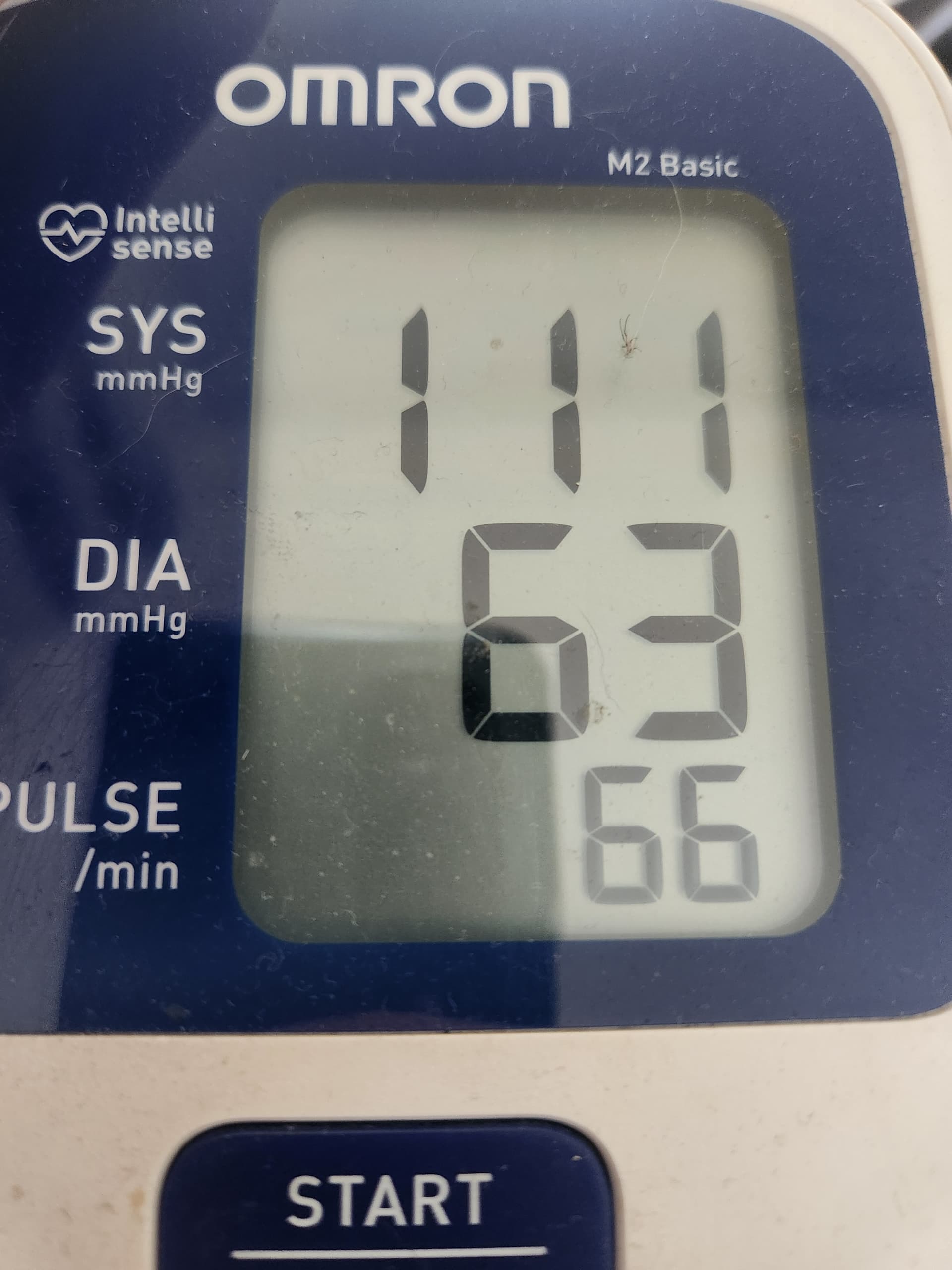
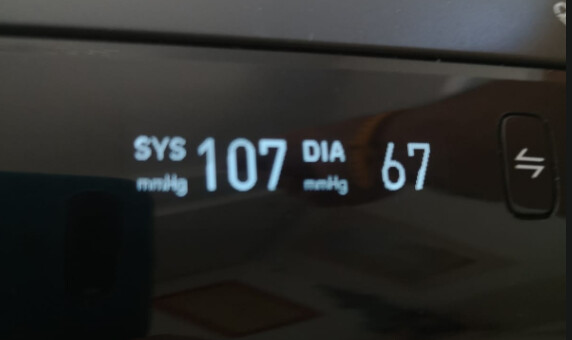
Guys, I just had to take my Omron out…
Just been out to a restaurant, but sober
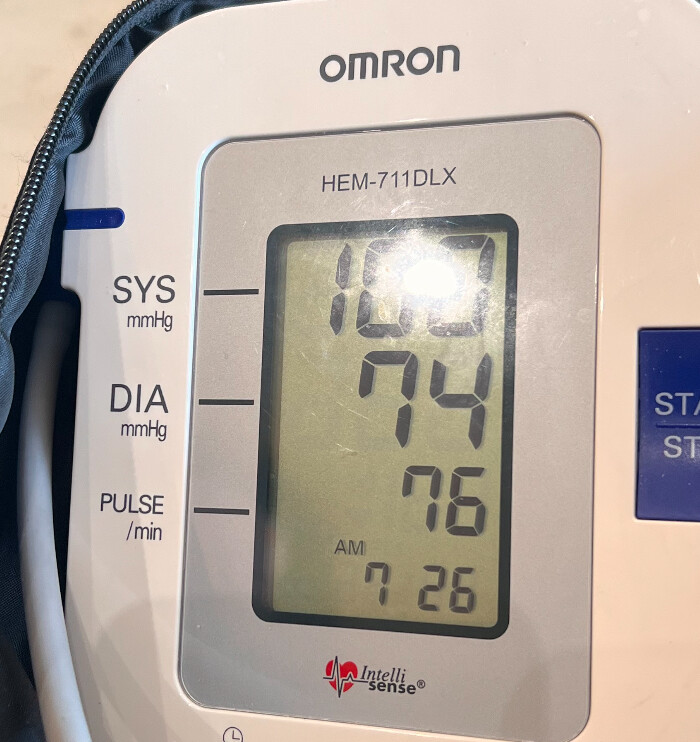
I go for the average arterial pressure which is 1/3 up from the diastolic.
Hard to see due to the glare, but it’s 100
Sys is often around 107-ish but has been as low as 90-95, too.
| Sys | Dias | AAP |
|---|---|---|
| 120 | 80 | 93.33333333 |
| 100 | 74 | 82.66666667 |
| 111 | 63 | 79 |
| 107 | 66 | 79.66666667 |
| 107 | 67 | 80.33333333 |
Solid numbers from all you guys!