These can move in hours to respond to an issue. I think it is sensible when getting a CBC to get a HsCRP. If that is elevated, then there is inflammation that will drive neutrophils up, or in some cases of a viral infection lymphocytes go up. The experience with covid was we usually got a neutrophilia even though it is a viral infection.
Even though I quit rapa I love this forum - have never heard of this ratio. Thanks for all your input to various questions DrFraser.
I do all the lifestyle modifications mentioned by dr Fraser including a near-perfect diet, yet my NLR is 8 and lymphocyres abysmally low. The downhill journey probably started with extensive radiation a few years ago, but it has become even worse lately.
I have tried a number of supplements to no effect. Just started my latest effort, injecting peptide Thymosin Alpha 1
On the bright side, I have had no infection or cold or sickness for ages. All around me catch colds but not me. Could it be that the dismal numbers somehow don’t matter in my case? All my other biomarkers are fine, e.g. hsCRP 0.17, in line with my life-style. I realize this is almost certainly wishful thinking, stemming from something I read with the gist that a strong body doesn’t need a high lymphocyte count… probably bs.
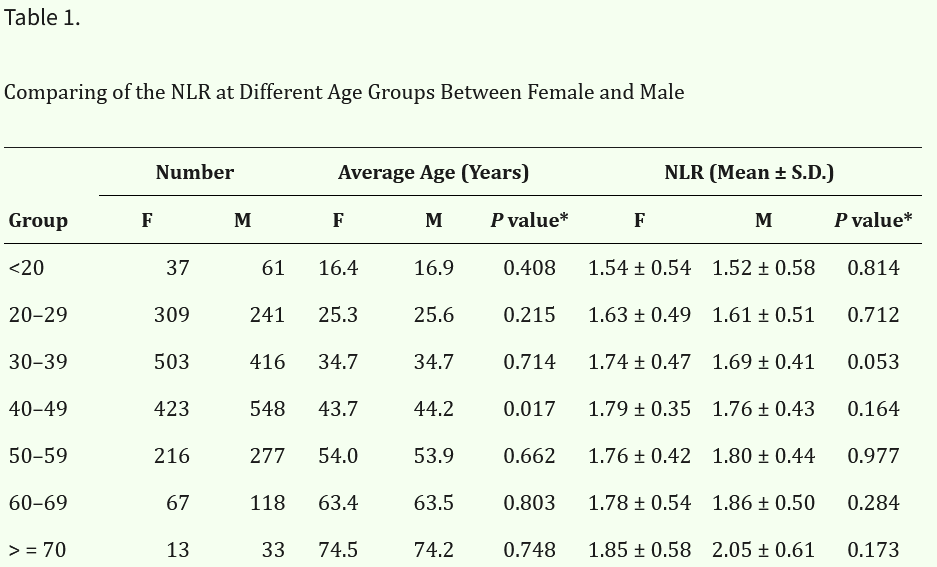
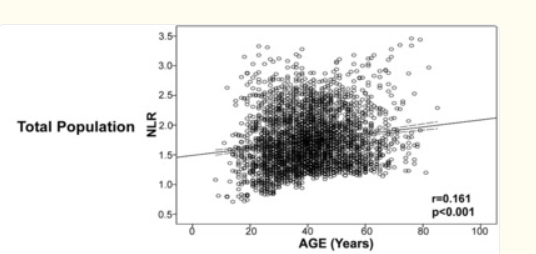
This study gives average lymphocytes by age in a healthy population:
with no significant difference between men and women:
other tidbits from the paper: NLR tends to go up with blood pressure, BMI, and various diseases.
NLR 8 is very high. Are you sure that you are calculating the ratio correctly?
I think the main issue in terms of Rapa and NLR is that the different types of WBC have different half lives. Hence as Rapa reduces the production of new WBC it hits Neutrophils first.
You can see that in my results on this topic.
To be honest, however, although NLR is a good target for improvement, the improvement from Rapamycin is I think meaningless.
Its a bit like the reduction in MCV which generally is good, but that from inhibiting mTOR does not mean otherwise the circumstances are good.
Just checking on your use protocol for this one. It has a short shelf life once reconstituted. It’s recommenced that once reconstituted a vial should be used in 5 days or less.
I set up my vials for 3 to 4 doses in 5 days. Did a low dose run a couple months ago, had a small bump up in lymphocytes and we have just started a 1 month, higher dose (1.67mg per). One month = 4 vials, only reconstituted prior to use.
It was almost 11:1 the last time before TA1. 4300 neutrophils per micrliter, 400 lymphocytes.
Maybe that was an extreme, it used to be more around 2800 and 600.
Now 2800 and 1000. Can’t wait for my order of TA1 to arrive.
I tend to be leucopenic even when not on rapa. My last result was 980 n vs 830 l. I think my protocol soups up short transcripts and i dont take any exogenous peptides.
I did 1.67 mg on three consecutive days. Can hardly get better results, but still ask do you think there is any advantage in spacing it more?
In clinical use, TA-1 is often dosed every day for months but that is for immune compromised individuals.
I’d do a more conservative approach like you are doing, 3 to 4 doses a week for 4 weeks and then test.
How long is the improvement expected to last? Can TA-1 be taken for a month every N months?
I also don’t gave an optimal NLR and do everything positive mentioned in this topic. ChatGPT suggested low-dose naltrexone, so I started 2mg/day 2 weeks ago. This is a good article about LDN for autoimmunity;
My neutrophil-to-lymphocyte ratio went down:
2.62/1.43 = 1.832 (March 10)
2.68/2.17 = 1.235. (Apr 14). Now worry it’s too low.
It could be bc of medication change: replaced Labetalol by Nebivolol, changed to Rapamycin 1 mg/week. Positives: feel overall better, occasional face puffiness is completely gone, some skin spots became lighter, skin in general improved much. Negatives: very slight occasional headache, lower HR (49 daytime and 38 sleep).
I’m going to throw some chit at the wall ![]() I’m going to use my engineering logic on this one. Which is probably different from a bio-science person with expertise in this area. So here goes…
I’m going to use my engineering logic on this one. Which is probably different from a bio-science person with expertise in this area. So here goes… ![]()
- TA-1 is one of the 3 hormones the Thymus produces that maturate T-cells.
- The Thymus eventually stops producing all the hormones that maturate T-cells (Thymic involution)
- T-cells continue to be produced over our life span in an non-maturated condition
- T-cells produced during Thymic involution may not be properly or fully maturated?
- T-cells produced when Thymic involution is inevitably complete, are not maturated at all.
- There are 4 main groups of T-cells with variances within those groups
- Each T-cell type has different half-lives
My “if > then” statement ![]()
As Thymosin A1 is a key “maturator”
If - T-cells become maturated by exogenous use of TA-1
Then - the effect of exogenous TA-1 on any T-cell that gets maturated should last for the life of that T-cell as it does for those maturated during the functional life of the rapidly involuting Thymus.
How long do naive T cells live and how are they replenished? A short life span for naive T cells would necessitate faster rates of replenishment, whereas in- creased life span would accommodate slower rates of replenishment. Work in this issue of Immunity by den Braber et al. (2012) examines the longevity of naive T cells. Their data suggest that mechanisms maintaining T cells with naive phenotypes might differ in humans and mice
And that is why I also use LL 37 when I’m working on my short term immune failures.
Posted this a while ago, my understanding is you want to be close to 1?
N = Neutrophil (innate) L = lymphocytes (acquired and innate)
Rapamycin mainly affect Neutrophil (?) @DrFraser
As to NLR , my understanding per Gork is you want your L higher than R but the ratio between 0.78-3.5 is considered normal.
And FWIW, my own blood works has shown little change in lymphocytes over the course of rapamycin, but my neutrophil to some degree is a function of rapamycin dose (suppressed lower but still normal). Hence, I monitor the trend and ratio of my NLR as a way to gauge my rapamycin dosing.
I agree - I think the major impact of Rapamycin is a decreased neutrophil count, and with that, you’ll improve ratio. I’ve seen some people have a little rise in lymphocytes, but not consistently. My average Rapamycin patient has a total WBC of around 3.5.
AIUI because neutrophils have a short half life intermittent rapamycin hits them quickly
I’ve got mild neutropenia according to my latest blood test. You think rapamycin is a likely cause? I took between 1 and 2 weeks off before the blood test, but I had quite bad mouth sore from the last dose so I think it might have hit me hard.