My meclizine vs rapamycin experiment:
As I have posted earlier, I tend to sail with the wind. I am too old to do anything else.
At the halfway point of this year, it seems reasonable to me to switch from rapamycin to meclizine. After reading many papers I am looking forward to giving meclizine a trial run.
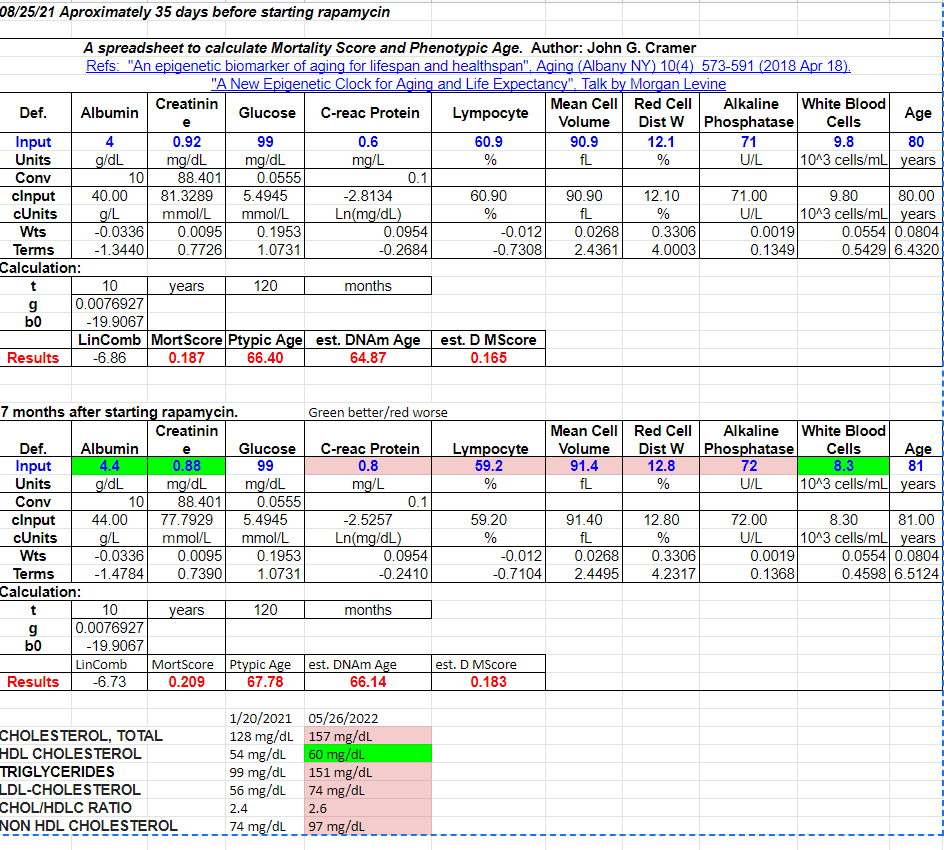
I will get my blood work done in ~ 3 weeks, ~30 days after my last rapamycin dose which was 15 mg taken with grapefruit juice. This will establish a personal baseline to measure the meclizine results against. The plan is to get my basic bloodwork done monthly.
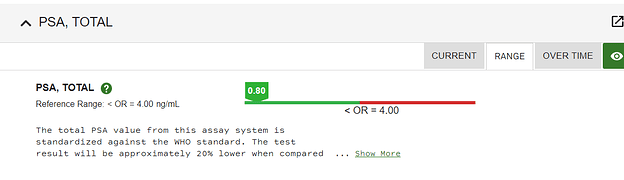
I will be taking meclizine at the 25 mg dose nightly. It was once part of my sleep stack so I am familiar with the possible side effects. It had no effect on my prostate that I am aware of. Meclizine didn’t have any effect on max urine flow. I have been taking tamsulosin for over 25 years and my PSA is 0.80 ng/mL
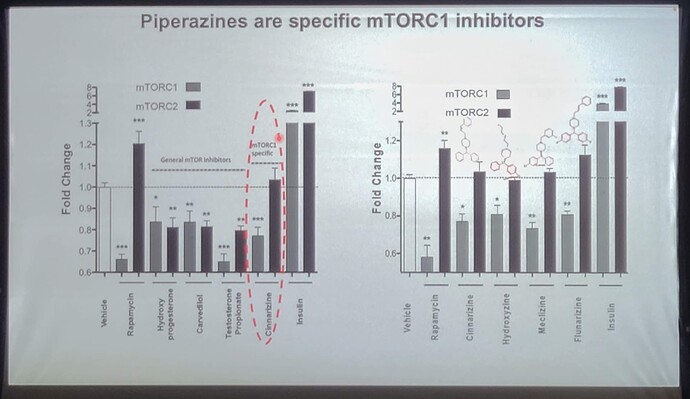
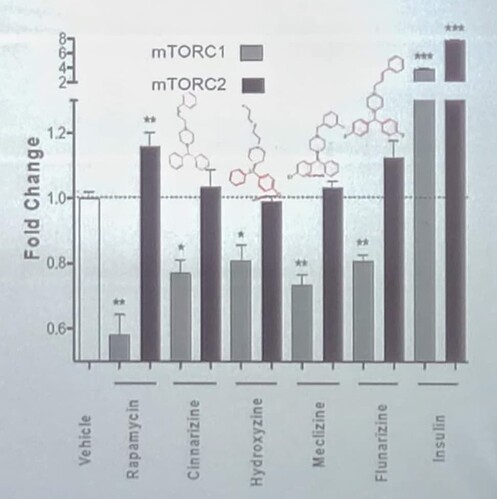
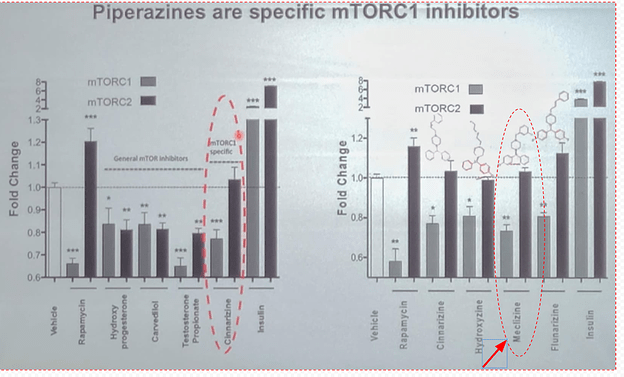
Meclizine seems to suppress mTORC1 without suppressing mTORC2. This is my main reason for switching at least temporarily.
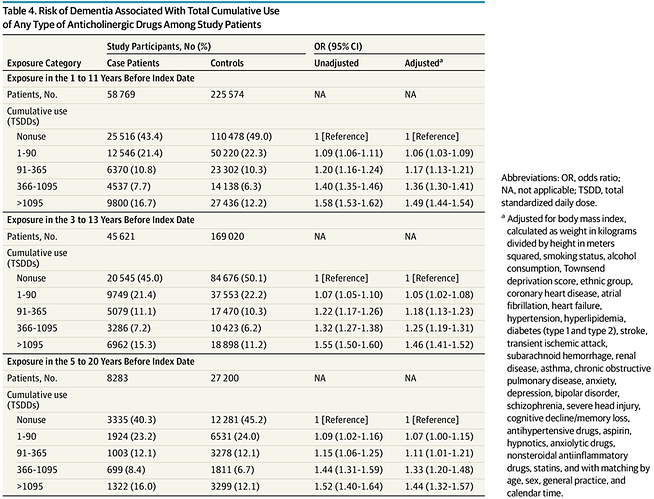
The fact that meclizine is anticholinergic is not much of a worry to me as these first-generation anti-histamines are being purchased by the boatload by elderly people as part of their constant fight to get a good night’s sleep. The danger, while real, is also small.
To be frank, I have been a little underwhelmed by rapamycin, I don’t doubt its positive effects, but I was hoping for a little more subjective well-being and energy. Perhaps its negative effects on mTORC2 account for that fact, or, maybe I am just too old.
I am excited to be embarking on a new track for a while.
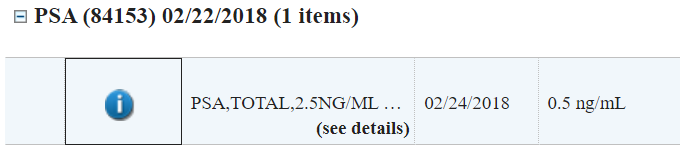
As you can see my doctor only orders this test every few years.